Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4762
Revised: May 11, 2024
Accepted: June 4, 2024
Published online: July 26, 2024
Processing time: 99 Days and 19.4 Hours
Retroperitoneal leiomyomas (RLs) are rare benign tumours that can occur in the pelvic and/or abdominal parietal retroperitoneum. Once torsion occurs, it causes acute abdominal pain and can even lead to serious consequences such as gan
Herein, we report the case of a 42-year-old woman with RL torsion. The patient visited our hospital complaining of lower abdominal pain for 6 d. Pelvic exami
In the case of a pelvic mass complicated with acute abdomen, the possibility of torsion should be considered.
Core Tip: Retroperitoneal leiomyoma torsion is extremely rare. We report a case of acute pedicular torsion of a leiomyoma in the posterior peritoneum, followed by a literature review. The review suggested that RL torsion mainly occurs in female patients, and the most prominent clinical symptom is abdominal pain. The possible imaging features of torsed retroperitoneal leiomyomas include a well-circumscribed mass separate from the uterus and adnexa, no enhancement, a torsed pedicle, and ascites. If the diagnosis is unclear, surgical exploration should be considered to confirm the diagnosis in a timely manner to reduce the risk of other complications.
- Citation: Li J, Zhu-Ge YY, Lin KQ. Torsed retroperitoneal leiomyomas: A case report and review of literature. World J Clin Cases 2024; 12(21): 4762-4769
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4762.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4762
Retroperitoneal leiomyomas (RLs) are rare benign tumours that can occur in the pelvic and/or abdominal parietal retroperitoneum. These tumours are characterized by smooth muscle differentiation and can be primary lesions or metastases from other sources[1]. Because of their rarity and uneventful clinical course, limited information is available about RLs.
RL torsion is extremely rare; once torsion occurs, it can cause acute abdominal pain and even lead to serious con
A 42-year-old woman (gravida 1, para 1) visited our hospital complaining of lower abdominal pain that started 6 d prior.
The patient came to our hospital complaining of severe, sudden-onset and constant dysmenorrhea-like pain localized to the lower abdomen 6 d prior. Her pain occurred while she was doing housework and was associated with loss of appetite but was not accompanied with fever, nausea, vomiting, or diarrhoea. The pain had nothing to do with food or body position. After 5 d of oral cefuroxime anti-inflammatory treatment, the pain gradually decreased, but there was still dull pain in the lower abdomen with no other discomfort.
She was first diagnosed with fibroids 6 years prior and underwent a Caesarean section 17 years prior and right mammary fibroma resection 1 year prior.
The patient denied having any relevant family history.
Her body temperature was normal. Pelvic examination revealed a tender mass superior to the uterus that was well circumscribed, medium in texture and approximately 10 cm × 10 cm × 10 cm in size.
The level of oncologic marker antigen 125 was 48.7 U/L, which was slightly greater than normal. No other abnormalities were found in routine blood analyses.
Ultrasonography revealed a hypoechoic mass in front of the uterus. Pelvic magnetic resonance imaging (MRI) revealed an anterior uterine mass, multiple uterine fibroids and slight pelvic effusion (Figure 1). No other pelvic abnormalities were found. MRI suggested the possibility of a subserosal myoma of the anterior uterine wall with degeneration.
The final diagnosis was RL torsion.
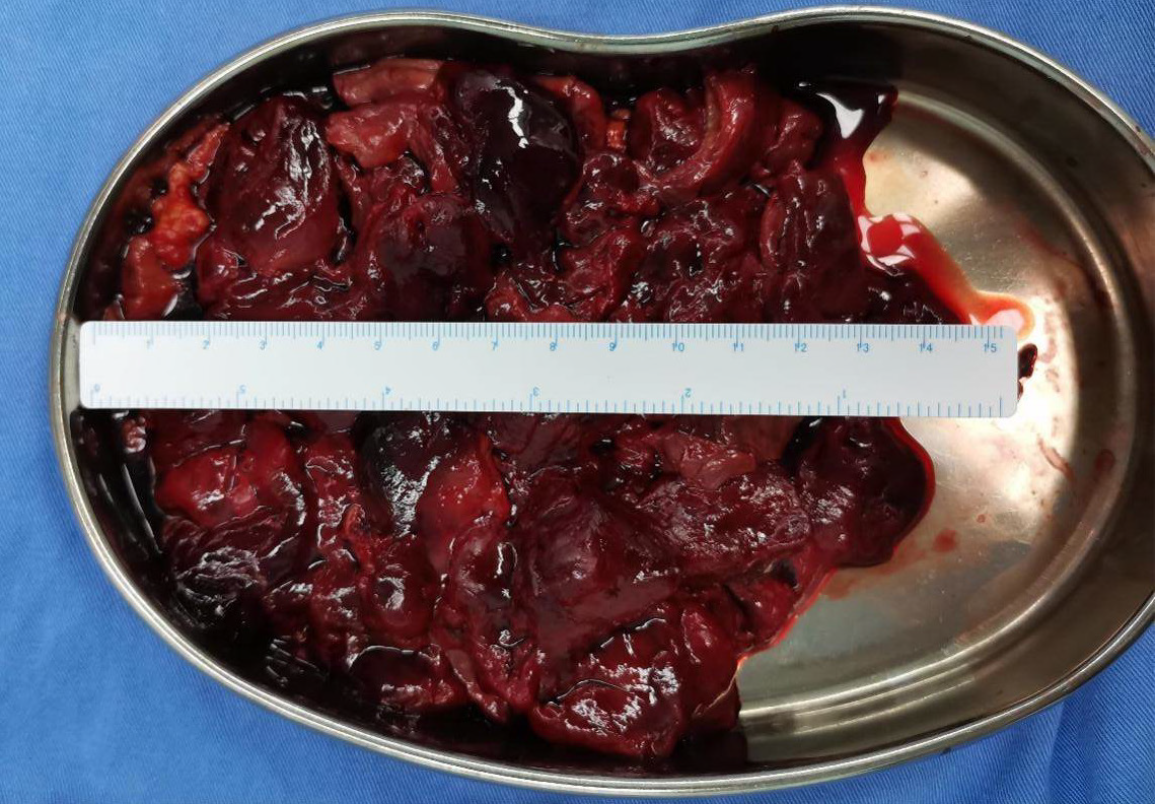
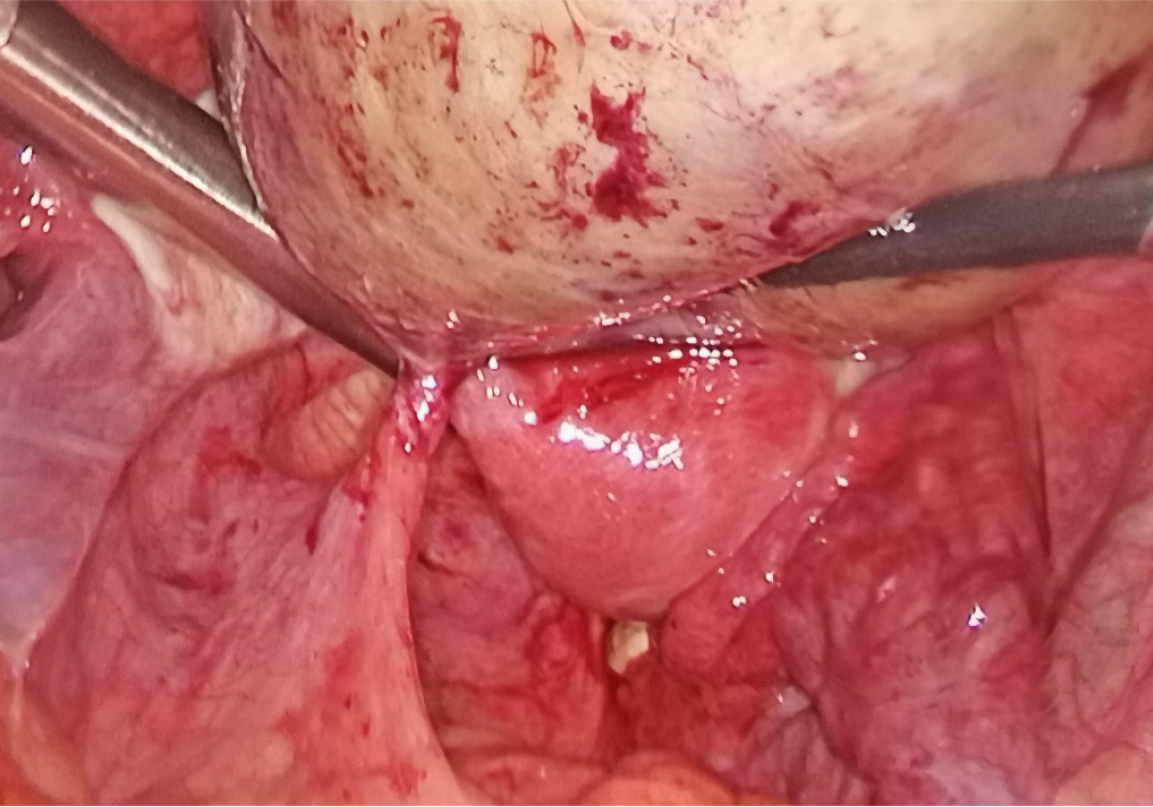
Based on her symptoms and age and the size of the mass, exploratory laparoscopy was performed. Intraoperative exploration revealed that part of the greater omentum was adhered to the anterior abdominal wall, and a large pedicled mass was observed in the pelvic cavity in front of the uterus, surrounded by and loosely adhered to the small intestine. The mass was 10 cm × 10 cm × 10 cm in size, greyish-red in colour, smooth on the surface and of medium quality (Figure 2). The pedicle was located 2 cm from the posterior peritoneum to the left of the rectum and was torsed 2 times (Figure 3). The upper and lower abdomens were explored, and no abdominal masses or enlarged lymph nodes were found. Pathological examination confirmed a retroperitoneal leiomyoma with a large area of haemorrhage and infarction. Immunohistochemical tests revealed positivity for desmin and smooth muscle actin, focal positivity for oestrogen receptor, individual positivity for Ki-67, and negativity for CD34 and S-100. The mass was removed laparoscopically, then placed in a specimen extraction bag and morcellated without spillage.
The patient recovered well and was discharged on postoperative day 5. After 2 years of follow-up, no tumour recurrence was observed.
A literature review identified 14 cases[2,6-18] of RL torsion in the PubMed database from 1960 through 2023 (Table 1). The PubMed database was searched with the following search terms or keywords: “torsion AND (fibroid OR myoma OR leiomyoma) AND (English[Language]) AND (("1960"[Date-Publication]: "2023"[Date-Publication]))”, yielding 188 results. Among these, 175 studies were excluded: 40 were reviews or guidelines only; 18 were retrospective or prospective articles not related to RL torsion; 19 were case reports not related to torsion; 36 were case reports of uterine torsion; 22 were case reports of adnexal torsion; 37 were case reports of uterine myoma torsion; 1 was a case report of testis torsion; 1 was a case report of appendix torsion; and 1 was case report of primary omental torsion, leaving 13 publications for review[2,6,8-18]. One article was found through a search of the bibliographies of the other articles[7], for a total of 14 English reports of RL torsion found via the PubMed database.
| Ref. | Year | Age in years | Size in cm | Origin of torsed myoma | Preoperative diagnosis | Route of surgery for the leiomyoma |
| Walrond et al[2] | 1973 | 59 | 20 | Posterior wall of the antrum of the stomach | Undiagnosed | Laparotomy |
| Brieger et al[6] | 1995 | 41 | 10 | Greater omentum | Torsion of an ovarian cyst | Laparoscopy |
| Yeh et al[7] | 1999 | 33 | 15 | Broad ligament | Torsion of a pedunculated fibroid | Not specified |
| Tan et al[8] | 2012 | 44 | Not specified | Greater omentum | Acute appendicitis | Laparotomy |
| Park et al[9] | 2013 | 45 | 7 | Mesentery | Not specified | Laparoscopy |
| Narasimhulu et al[10] | 2015 | 40 | 9.6 | Anterior wall of the rectum | Parasitic fibroids with degeneration | Laparotomy |
| Hirayama et al[11] | 2015 | 37 | 8.5 | Greater omentum | Torsion of left ovarian tumour | Laparotomy |
| Cho et al[12] | 2016 | 38 | 16 | Greater omentum | Omental torsion | Laparotomy |
| Kaya et al[13] | 2018 | 28 | 4.5 | Round ligament | Undiagnosed | Laparoscopy |
| Bajis et al[14] | 2018 | 47 | 25 | Mesentery of the ileocaecal junction | Ovarian cyst torsion | Laparotomy converted from laparoscopy |
| Sofoudis et al[15] | 2020 | 43 | 9 | Intestinal tube | Not specified | Laparoscopy |
| Stebbings et al[16] | 2021 | 39 | 10 | Greater omentum | Appendicitis | Laparoscopy |
| Miles et al[17] | 2021 | 48 | 19.3 | Posterior wall of the antrum of the stomach | Myoma torsion | Laparoscopy |
| Lu et al[18] | 2022 | 42 | Not specified | Greater omentum | Not specified | Laparoscopy |
| Our patient | - | 42 | 10 | Broad ligament | Undiagnosed | Laparoscopy |
The ages of the 15 patients, including ours, ranged from 33 years to 59 years, and the average age was 40.91 years. Eleven of the fifteen patients had a history of uterine leiomyoma surgery or were diagnosed intraoperatively with uterine leiomyomas.
The size of the fibroids was not recorded in 2 patients; the diameter of the fibroids of the other 13 patients was 4.5-25 cm, with a median of 10 cm and an average of 12.6 cm. The tumours mainly originated from the pelvic cavity, including the greater omentum in patients, the round ligament in 2 patients, the mesentery in 2 patients, the broad ligamentum in 1 patient, the anterior wall of the rectum in 1 patient, the intestinal tube in 1 patient, the bladder peritoneum in 1 patient and the posterior peritoneum in 1 patient. Only one tumour originated from the antrum of the upper abdomen.
Seven of the fifteen patients also presented with uterine leiomyomas that were identified intraoperatively, and three did not have complications. Complication information for the other 5 patients was not provided.
Six patients had a previous history of uterine fibroid surgery, including abdominal myomectomy in two patients, laparoscopic hysterectomy in one patient and laparoscopic myomectomy in three patients, while six patients had no surgical history. For all patients who underwent laparoscopic surgery, a morcellator was used. The surgical history of 3 patients was not indicated.
The aetiology of RL is unclear, but it mainly occurs in female patients, especially in perimenopausal or postmenopausal patients, and more than 40% of female patients with RL also have previous or concurrent uterine leiomyoma[1,19].
Subserous leiomyoma detachment and implantation may be a characteristic of RL. When the pedicle is narrower than the tumour diameter, a pedicled subserous fibroid may occasionally detach from the uterus and derive its blood supply from the adhesive tissue[20]. In another 2 patients with RL torsion[6,11], no uterine leiomyoma was found via pre
The seeding hypothesis is also considered an important pathogeny of the RL. Parasitic fibroids are thought to account for a large proportion of RLs. It is believed that parasitic leiomyomas can develop after surgery on uterine fibroids by seeding residual tissue fragments in the abdominal cavity[6,16,21-25]. The duration of steroid exposure after surgery might be a risk factor for the development of parasitic myomas[26]. Among the 15 patients with RL torsion, 6 had a previous history of leiomyoma surgery, including laparoscopic hysterectomy for 1 patient, laparoscopic myomectomy for 3 patients, and abdominal myomectomy for 2 patients. Three, two, three and six parasitic leiomyomas were detected intraoperatively in the 4 patients among these with a history of morcellation[8,10,15,18], while only one fibroid was found in the 2 patients with a history of abdominal myomectomy[9,12]. A greater number of parasitic leiomyomas were detected intraoperatively in patients with a history of morcellation, suggesting that laparoscopic morcellation may be more likely to lead to the development of parasitic leiomyomas. The use of a containment bag for decreasing the burden of tissue dissemination may mitigate the risk of tissue spread during morcellation[26]. Therefore, in patients with abdominal or pelvic pain, if there is a history of uterine fibroid surgery, especially hysterectomy or myomectomy with morcellation, torsion of parasitic myomas should be considered.
It is assumed that Caesarean section can also lead to the seeding of leiomyoma cells[16]. When Caesarean section is performed, uterine leiomyomas may be breached and seeded during the opening and closure of the uterine cavity. Among the 15 patients with RL torsion, 3 had undergone neither previous laparoscopic morcellation nor abdominal myomectomy but did have a history of Caesarean section[14,16]. The patient described by Stebbings et al[16], who had three elective Caesarean section deliveries but no other surgical history, was confirmed to have RL torsion complicated with uterine leiomyomas.
However, the seed and soil hypothesis cannot explain all of the cases. In the case reported by Bajis et al[14], the uterus was confirmed to be normal intraoperatively, which indicated that the torsed myoma may not have been a parasitic tumour. Our patient, whose case was confirmed to have RL torsion complicated by uterine leiomyomas intraoperatively, had no other uterine surgery history but underwent a Caesarean section 17 years prior to identification of the torsion. However, given the long time between the Caesarean section and the RL torsion, there may be other causes for the development of the RL. These findings suggest that these RLs may be primary RLs.
Most RLs are positive for oestrogen receptor or progesterone receptor and have pathological and histological characteristics similar to those of uterine leiomyomas[1,19], which suggests that these two types of leiomyomas may have the same aetiological basis. Stutterecker et al[27] speculated that the origins of RL may be embryonal remnants (e.g., the tubes of Müller and Wolff) or local vessel musculature. Pathologic and immunohistochemical findings of most RLs are similar to those of uterine fibroids but still cannot explain the origins of nonpelvic RLs, receptor-negative RLs, or RLs in males[1,19]. The pathogenesis of RL may involve multiple mechanisms and be related to multiple factors.
Given the rarity of RLs, RL torsion is exceptionally rare. Leiomyoma torsion, a known cause of acute abdominal pain, occasionally occurs in pedicled subserous uterine fibroids. The incidence of leiomyoma torsion has been reported to be less than 0.25% in patients who undergo surgical treatment for subserous uterine leiomyomas[28]. Factors associated with leiomyoma torsion include the presence of a pedicle, a larger size and weight, the size of the vascular pedicles of the leiomyoma, and pregnancy[3,28]. Like uterine leiomyoma torsion, a larger size and pediculation are associated with RL torsion. The 15 torsed RLs were all pedicled. Except for 2 patients whose tumour size was unknown, all the tumours were no less than 4.5 cm in size, and 6 of them were no less than 10 cm in size.
The most prominent clinical symptom of RL torsion was abdominal pain, which was present in all 15 patients. Once RL torsion occurs, in addition to the similar symptoms of uterine leiomyoma torsion, such as abdominal pain, nausea, and fatigue[9,12,16,17,28], different symptoms may also occur depending on the site of the lesion. Sofoudis et al[15] reported on a 43-year-old woman with intestinal parasitic myoma torsion who presented with diffuse abdominal pain, gas
As in cases of appendicular torsion and uterine fibroid torsion, in cases of RL torsion, the most common clinical signs are tender masses in the pelvis and abdominal cavity, followed by peritoneal irritation, distress and fever.
Although RLs do not seem to have any specific imaging features, imaging examinations, including ultrasound, computed tomography (CT) and MRI, are valuable for the preoperative diagnosis of RL torsion. These methods can aid in detecting pelvic or abdominal boundary masses and also help to explore the relationship between the masses and the uterus[3,7,29,30].
The possible imaging features of RLs include a well-circumscribed mass separate from the uterus and adnexa, no enhancement, a torsed pedicle, and ascites. Torsed RLs are often separate from both the uterus and adnexa. However, when the RL is adjacent to or even adhered to the uterus, as with the RLs observed in our study and in three other studies[7,16,17], it is more likely to be misdiagnosed as a uterine fibroid.
Torsed tissues, such as the adnexa, may not demonstrate any enhancement compared to normal tissues on CT and MRI[3], and the torsed RL demonstrated the same characteristics[10,11]. On ultrasound, the spectral Doppler flow within the vascular pedicle and the mass itself is sometimes absent[3].
A torsed pedicle can yield a more confident diagnosis of torsion. The “whirlpool sign” and “swirl sign”, indicating the appearance of vascular pedicular torsion, can be demonstrated on cross-sectional images[3,17]. When omental torsion occurs, a whirling pattern of fatty streaks within the omentum, which is considered a relatively characteristic feature of omental torsion, can be observed on coronal views[12].
Ascites is another sign of RL torsion[7]. Among the 15 patients identified here and in the review, effusion was found in our study and 5 others[7,8,12,14,16]. Ascites may first be caused by obstruction of the venous return; then, gangrene, inflammation and even bleeding can occur in torsed RLs[3-5], as can exudation of the surrounding tissues.
Notably, when the mass is outside or high within the pelvis, transvaginal ultrasonography may not visualize the area well[7], and transabdominal ultrasonography or CT or MRI scans are necessary. This was demonstrated in the case reported by Park et al[9], in which transvaginal ultrasonography was the only imaging examination performed before surgery, revealing that the torsed mass was in the right paracolic gutter and was not detected preoperatively.
Due to the lack of specific clinical and imaging features, it is difficult to make a preoperative diagnosis of leiomyoma torsion[3,28]. Moreover, the rarity and uncertain location of the RL increase the difficulty of preoperatively diagnosing RL torsion. However, imaging techniques are important and useful for diagnosis, not only because they can help to define the location and nature of the mass but also because they can be used to exclude other intraperitoneal lesions[4].
The main treatment for RL torsion is surgery, most commonly involving myomectomy. If the torsion is not relieved in time, it may be followed by gangrene, peritonitis, haemoperitoneum, or even shock[2-5]. Therefore, the possibility of RL torsion should be considered in patients with pelvic masses associated with acute abdominal pain and other related symptoms. In addition, if the diagnosis is unclear, surgical exploration should be considered to confirm the diagnosis in a timely manner to reduce the risk of other complications. Laparoscopic exploration may be a good option for making a clear diagnosis and excision.
Overall, the findings of this case suggest that when a patient presents with a pelvic mass complicated with acute abdomen, even if the mass is far from the uterus and accessory organs, the possibility of torsion should still be con
The authors would like to thank Dr. Chen Hao for his contribution to the pathological examination.
| 1. | Paal E, Miettinen M. Retroperitoneal leiomyomas: a clinicopathologic and immunohistochemical study of 56 cases with a comparison to retroperitoneal leiomyosarcomas. Am J Surg Pathol. 2001;25:1355-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 82] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Walrond ER, Sahoy RR. Torsion of a gastric leiomyoma. Br J Surg. 1973;60:326-327. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Bonney R, Revels JW, Wang SS, Lussier R, Dey CB, Katz DS, Moshiri M. A comprehensive radiologic review of abdominal and pelvic torsions. Abdom Radiol (NY). 2021;46:2942-2960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Levai AM, Rotar IC, Muresan D. Torsion of a uterine leiomyoma - a rare cause of hemoperitoneum; a case report and review of the literature. Med Ultrason. 2019;21:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Chen YL, Chen LR, Chen KH. Sudden rupture with internal bleeding and shock following torsion and necrosis of a large uterine leiomyoma. J Obstet Gynaecol. 2019;39:566-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 6. | Brieger GM, MacGibbon AL, Peat BP. Torsion of a parasitic fibroid. Aust N Z J Obstet Gynaecol. 1995;35:224-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Yeh HC, Kaplan M, Deligdisch L. Parasitic and pedunculated leiomyomas: ultrasonographic features. J Ultrasound Med. 1999;18:789-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Tan CH, Ho BC, Shelat V, Tan CH. Leiomyomatosis peritonealis disseminata presenting as omental torsion. Singapore Med J. 2012;53:e71-e73. [PubMed] |
| 9. | Park DS, Shim JY, Seong SJ, Jung YW. Torsion of parasitic myoma in the mesentery after myomectomy. Eur J Obstet Gynecol Reprod Biol. 2013;169:414-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Narasimhulu DM, Eugene E, Sumit S. Torsion of an iatrogenic parasitic fibroid related to power morcellation for specimen retrieval. J Turk Ger Gynecol Assoc. 2015;16:259-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Hirayama A, Matsushita H, Yanase T, Kurabayashi T. Torsion of the pedicle of a fibroid parasitized to the greater omentum. J Obstet Gynaecol. 2015;35:760-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Cho IA, Baek JC, Park JK, Song DH, Kim WJ, Lee YK, Park JE, Shin JK, Choi WJ, Lee SA, Lee JH, Paik WY. Torsion of a parasitic myoma that developed after abdominal myomectomy. Obstet Gynecol Sci. 2016;59:75-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Kaya C, Alay İ, Babayeva G, Güraslan H, Ekin M, Yaşar L. Laparoscopic Management of a Torsioned Round Ligament Fibroid. Oman Med J. 2018;33:441-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 14. | Bajis R, Eloundou G. Unusual Case of a Torted Mesenteric Fibroid. Case Rep Obstet Gynecol. 2018;2018:8342127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Sofoudis C, Trouvas D, Zioris K. Torsion of intestinal parasitic myoma after laparoscopic morcellation: a case report. J Surg Case Rep. 2020;2020:rjaa032. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Stebbings C, Latif A, Gnananandan J. Torsion of a parasitic leiomyoma: a rare but important differential in women presenting with lower abdominal pain. BMJ Case Rep. 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 17. | Miles S, Mansuria S, Foley CE. Laparoscopic Approach to Myoma Torsion. J Minim Invasive Gynecol. 2021;28:734-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Lu HF, Chuang YC, Peng FS, Liu HM, Chen SU. Recurrent Intermittent Abdominal Pain with Parasitic Myoma Torsion. J Minim Invasive Gynecol. 2022;29:814-815. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Poliquin V, Victory R, Vilos GA. Epidemiology, presentation, and management of retroperitoneal leiomyomata: systematic literature review and case report. J Minim Invasive Gynecol. 2008;15:152-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Jermy KV, Stanton SL, Nager CW, Kumar D. A leiomyomatous perineal hernia? Br J Obstet Gynaecol. 1999;106:507-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Thian YL, Tan KH, Kwek JW, Wang J, Chern B, Yam KL. Leiomyomatosis peritonealis disseminata and subcutaneous myoma--a rare complication of laparoscopic myomectomy. Abdom Imaging. 2009;34:235-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Huang PS, Chang WC, Huang SC. Iatrogenic parasitic myoma: a case report and review of the literature. Taiwan J Obstet Gynecol. 2014;53:392-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Darii N, Anton E, Doroftei B, Ciobica A, Maftei R, Anton SC, Mostafa T. Iatrogenic parasitic myoma and iatrogenic adenomyoma after laparoscopic morcellation: A mini-review. J Adv Res. 2019;20:1-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Sinha R, Sundaram M, Lakhotia S, Kadam P, Rao G, Mahajan C. Parasitic myoma after morcellation. J Gynecol Endosc Surg. 2009;1:113-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Bruno M, Pelaccia E, Di Florio C, Palumbo P, Sollima L, Ludovisi M, Guido M. Conservative Management and Ultrasound Follow-Up of Parasitic Myoma: Our Experience and Literature Review. Diagnostics (Basel). 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 26. | Van der Meulen JF, Pijnenborg JM, Boomsma CM, Verberg MF, Geomini PM, Bongers MY. Parasitic myoma after laparoscopic morcellation: a systematic review of the literature. BJOG. 2016;123:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 27. | Stutterecker D, Umek W, Tunn R, Sulzbacher I, Kainz C. Leiomyoma in the space of Retzius: a report of 2 cases. Am J Obstet Gynecol. 2001;185:248-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Lai YL, Chen YL, Chen CA, Cheng WF. Torsion of pedunculated subserous uterine leiomyoma: A rare complication of a common disease. Taiwan J Obstet Gynecol. 2018;57:300-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 29. | Ohgiya Y, Seino N, Miyamoto S, Takeyama N, Hatano K, Munechika J, Ishizuka K, Hirose M, Ohike N, Hashimoto T, Sekizawa A, Gokan T. CT features for diagnosing acute torsion of uterine subserosal leiomyoma. Jpn J Radiol. 2018;36:209-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Le D, Dey CB, Byun K. Imaging findings of a torsed pedunculated uterine leiomyoma: A case report. Radiol Case Rep. 2020;15:144-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/