Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4673
Revised: June 6, 2024
Accepted: June 7, 2024
Published online: July 26, 2024
Processing time: 62 Days and 10.5 Hours
Data from the World Health Organization’s International Agency for Research on Cancer reported that China had the highest prevalence of cancer and cancer deaths in 2022. Liver and pancreatic cancers accounted for the highest number of new cases. Real-world data (RWD) is now widely preferred to traditional clinical trials in various fields of medicine and healthcare, as the traditional research approach often involves highly selected populations and interventions and controls that are strictly regulated. Additionally, research results from the RWD match global reality better than those from traditional clinical trials.
To analyze the cost disparity between surgical treatments for liver and pancreatic cancer under various factors.
This study analyzed RWD 1137 cases within the HB1 group (patients who underwent pancreatectomy, hepatectomy, and/or shunt surgery) in 2023. It distinguished different expenditure categories, including medical, nursing, technical, management, drug, and consumable costs. Additionally, it assessed the contribution of each expenditure category to total hospital costs and performed cross-group comparisons using the non-parametric Kruskal–Wallis test. This study used the Steel–Dwass test for post-hoc multiple comparisons and the Spearman correlation coefficient to examine the relationships between variables.
The study found that in HB11 and HB13, the total hospitalization costs were significantly higher for pancreaticoduodenectomy than for pancreatectomy and hepatectomy. Although no significant difference was observed in the length of hospital stay between patients who underwent pancreaticoduodenectomy and pancreatectomy, both were significantly longer than those who underwent liver resection. In HB15, no significant difference was observed in the total cost of hospitalization between pancreaticoduodenectomy and pancreatectomy; however, both were significantly higher than those in hepatectomy. Additionally, the length of hospital stay was significantly longer for patients who underwent pancreaticoduodenectomy than for those who underwent pancreatectomy or liver resection.
China Healthcare Security Diagnosis Related Groups payment system positively impacts liver and pancreatic cancer surgeries by improving medical quality and controlling costs. Further research could refine this grouping system and ensure continuous effectiveness and sustainability.
Core Tip: To analyze cost differences and their influencing factors in surgical treatments for liver and pancreatic cancer within the China Healthcare Security Diagnosis Related Groups (CHS-DRG) payment system, this study aims to examine the appropriateness of the current diagnosis-related groups groupings and provide recommendations for improvement. The CHS-DRG payment system has shown a positive impact on the surgical treatment of liver and pancreatic cancer by enhancing medical quality and managing costs. However, additional research is necessary to refine the grouping system and ensure its continued effectiveness and sustainability.
- Citation: Hu YH, Yu F, Zhou YZ, Li AD. Surgical treatment of liver cancer and pancreatic cancer under the China Healthcare Security Diagnosis Related Groups payment system. World J Clin Cases 2024; 12(21): 4673-4679
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4673.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4673
The China Healthcare Security Diagnosis Related Groups (CHS-DRG) is a tool for clinical management based on the first page of medical records, considering individual characteristics such as disease diagnosis, treatment methods, comorbidities, complications and age of cases, and then dividing diseases into several disease diagnosis groups according to the principle of similar clinical pathways and similar resource consumption. The CHS-DRG payment system plays a vital role in reforming the payment modalities for health insurance. Its main objectives include controlling medical expenditures, improving the efficiency of medical services, standardizing medical service practices, and optimizing the use of health insurance funds[1].
Real-world data (RWD) are research data that originate from the actual medical environment and reflect real diagnoses, treatment processes, and patient health statuses. This type of data differs from traditional clinical trials, in which populations are often highly selected and interventions and controls are strictly regulated. Apparent differences exist in various aspects, such as follow-up procedures and real-world conditions. Based on the data source, RWD can be divided into research and non-research data[2]. Owing to research results from the RWD matching reality and their extrapolation potential, RWD is now widely used in various fields of medicine and healthcare[3].
The latest data from the World Health Organization’s International Agency for Research on Cancer on the global cancer burden indicate that China had the highest number of new cancer cases and deaths in 2022. Liver and pancreatic cancers were the most common cancers in China and constituted the top list of new cases[4]. These two cancers also have the lowest 5-year survival rates[5]. The surgical treatment of hepatobiliary and pancreatic tumors is complicated, the overall cost is relatively high, and the economic burden of patients is relatively heavy. Establishing a scientific and reasonable diagnosis-related groups (DRGs) grouping scheme for hepatobiliary and pancreatic tumors is particularly important.
This study used RWD to focus on a tertiary cancer specialty hospital in Beijing. The analysis included using the non-parametric Kruskal–Wallis test for comparing data between multiple groups and the non-parametric Tukey Steel–Dwass test for post-hoc multiple comparisons. Spearman’s correlation coefficient was used to assess the relationships between variables. This study investigated the differences in hospital costs and influencing factors for patients undergoing surgical treatment for liver and pancreatic cancer within the pancreatic and liver resection and/or shunt surgery groups under the CHS-DRG payment system. It evaluated the current DRG grouping scheme and proposed recommendations to improve the scientific and rational aspects of DRG payment standards. By aligning with clinical practice and promoting the efficient allocation and utilization of medical resources, this study aimed to facilitate collaboration among health insurance providers, hospitals, and healthcare providers, thereby enabling patients to benefit from the implementation of DRGs.
This study utilized data from the Beijing Region Inpatient Medical Service Performance Evaluation Platform, which collected information from the first page of patient records from January to December 2023. This information included details such as the length of stay, type of surgery, complications, and costs. Following the CHS-DRG 1.1 version of the grouping scheme, the study focused on 1137 patients in the HB1 group who underwent pancreatic and liver resection and/or shunt surgery. Surgical methods, including liver resection, pancreatectomy, and pancreaticoduodenectomy, were categorized based on inclusion criteria and surgical site. Patients were further categorized into subgroups based on complications/comorbidities during hospitalization: 462 HB11 patients with severe complications or comorbidities, 497 HB13 patients with severe complications or comorbidities, and 178 HB15 patients without complications or comorbidities.
This study analyzed the cost structure of inpatients by distinguishing between medical, nursing, medical technology, administrative, drug, and consumption costs. It also evaluated the contribution of various cost categories to the total hospitalization costs. Strict data encryption and privacy protection measures were taken to ensure the confidentiality of patients’ personal information. The variables were carefully controlled to enhance the scientific validity and reliability of the results. Measures were taken to avoid potential blind spots in data collection and ensure high standards of data quality.
Variables such as length of stay and hospital costs demonstrated a skewed distribution. The
Table 1 compares the total cost of hospitalization and length of stay for the different surgical categories within the various DRG groups. In HB11, the total hospitalization cost for pancreaticoduodenectomy was significantly higher than that for pancreatectomy, which in turn was significantly higher than that for hepatectomy. The duration of hospitalization for pancreaticoduodenectomy was not significantly different from that for pancreatectomy; however, both were significantly longer than those for liver resection. In HB13, the total hospitalization costs for the three operations followed a similar pattern as in HB11, with pancreaticoduodenectomy being significantly higher than pancreatectomy and hepatectomy. A comparison of the hospitalization days among the three groups showed a similar trend. In HB15, no significant difference was observed in the total cost of hospitalization between pancreaticoduodenectomy and pancreatectomy; however, both were significantly higher than those in hepatectomy. Regarding the length of stay, pancreaticoduodenectomy was significantly longer than pancreatectomy and hepatectomy, whereas no significant difference was found between pancreatectomy and hepatectomy.
| DRG | Surgery classification | Total hospitalization expenses | The number of days in hospital | ||||
| Median (quartiles) | χ2 | P value | Median (upper and lower quartiles) | χ2 | P value | ||
| HB11 | 158.75 | < 0.0001 | 125.9 | < 0.0001 | |||
| Liver resection | 74463.5 (60025.5, 94356)3 | 9 (7, 12)2 | |||||
| Pancreaticoduodenectomy | 142663 (133720, 179562.25)1 | 20 (14.25, 24.75)1 | |||||
| Pancreatectomy | 102252.5 (95235, 119203.25)2 | 13.5 (11, 18.75)1 | |||||
| HB13 | 234.83 | < 0.0001 | 131.83 | < 0.0001 | |||
| Liver resection | 63929 (51004.75, 78147)3 | 7 (7, 10.25)3 | |||||
| Pancreaticoduodenectomy | 136335 (120212, 165313.5)1 | 16 (12.5, 22)1 | |||||
| Pancreatectomy | 92788.5 (79258.5, 105594.25)2 | 10.5 (8, 14.25)2 | |||||
| HB15 | 44.60 | < 0.0001 | 15.06 | 0.0005 | |||
| Liver resection | 67274.5 (54285.25, 81836.25)2 | 9.5 (7, 13)2 | |||||
| Pancreaticoduodenectomy | 134561 (114775, 150848)1 | 19 (11, 22)1 | |||||
| Pancreatectomy | 82528 (76816, 95098)1 | 11 (8, 13.5)2 | |||||
For each patient, the proportion of individual expenditure categories in the total expenditure was calculated, and the mean value of the proportion in each group was determined. Table 2 presents the study’s results. In each DRG and surgical category, consumables and medicines accounted for the highest proportion of total expenditure, followed by medical expenditure. Nursing, medical technology, and management fees were the three categories with the lowest percentages.
| DRG | Surgery classification | Average medical expense ratio | Average proportion of nursing expenses | Average proportion of medical technology expenses | Average management fee ratio | Average proportion of consumables expenses | Average proportion of drug expenses |
| HB11 | Liver resection | 12.39 | 1.09 | 3.05 | 3.05 | 38.59 | 37.45 |
| Pancreaticoduodenectomy | 10.69 | 1.57 | 2.85 | 2.85 | 34.80 | 43.05 | |
| Pancreatectomy | 11.38 | 1.40 | 3.01 | 3.01 | 36.45 | 42.32 | |
| HB13 | Liver resection | 14.13 | 1.07 | 2.88 | 2.88 | 43.04 | 31.87 |
| Pancreaticoduodenectomy | 10.95 | 1.49 | 2.65 | 2.65 | 38.23 | 40.81 | |
| Pancreatectomy | 12.66 | 1.25 | 2.69 | 2.69 | 40.03 | 38.44 | |
| HB15 | Liver resection | 13.55 | 1.15 | 3.00 | 3.00 | 43.13 | 31.94 |
| Pancreaticoduodenectomy | 11.10 | 1.52 | 3.83 | 3.83 | 35.91 | 41.90 | |
| Pancreatectomy | 13.04 | 1.34 | 2.73 | 2.73 | 40.33 | 37.35 |
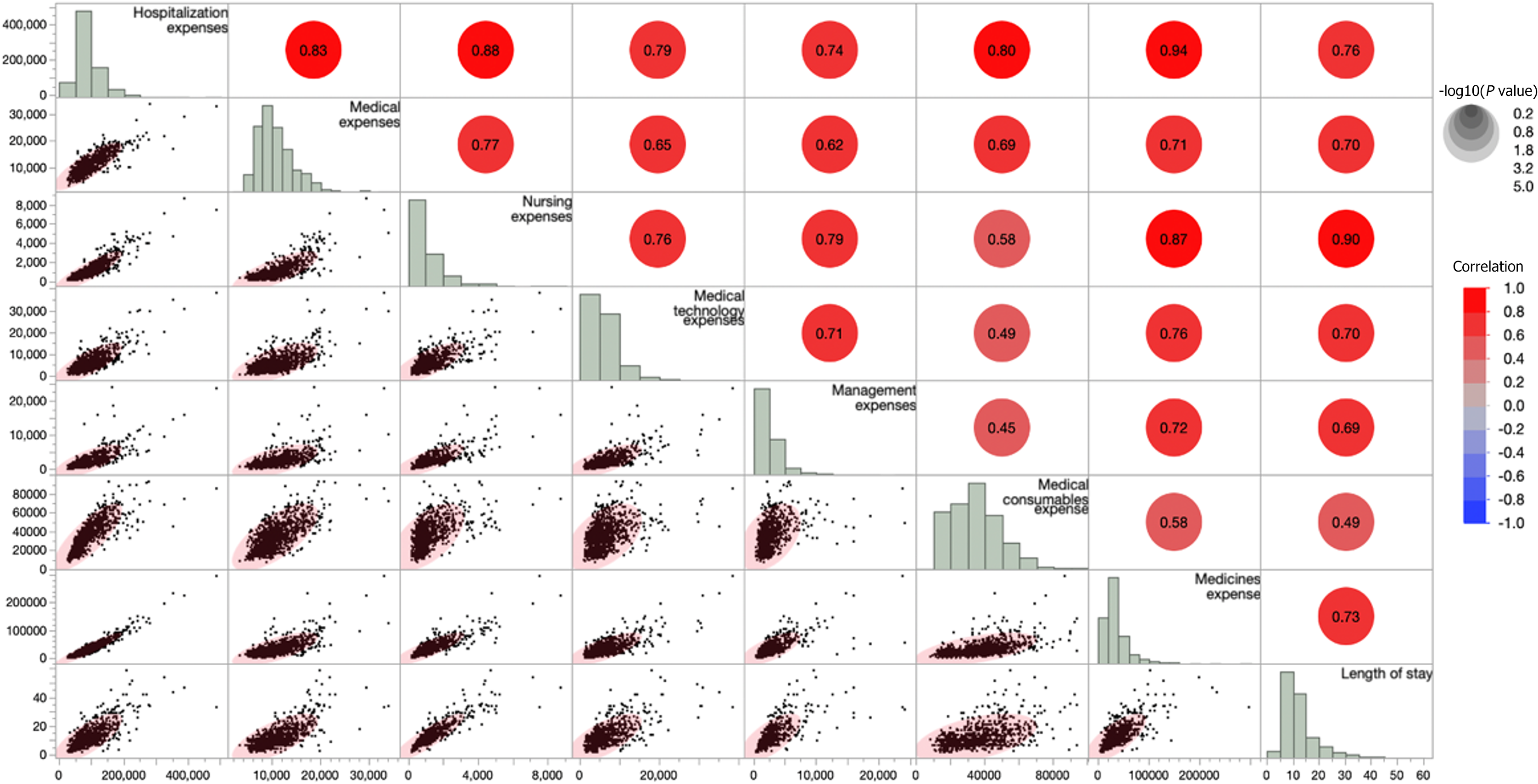
The correlation analysis results indicated a significant positive correlation between total hospitalization costs, sub-item costs, and length of stay (Figure 1). The strongest correlation (0.94) was observed between total hospitalization expenses and drug costs. Nursing, medical, and consumable expenses exhibited correlations of 0.88, 0.83, and 0.80, respectively, with total hospitalization expenses. Medical technology fees exhibited a correlation of 0.79, whereas management fees demonstrated the lowest correlation at 0.74 with total hospitalization expenses. The correlation between the total hospitalization cost and length of stay was 0.76.
The DRG transforms medical service output into a relatively measurable model, thereby aiming to reduce medical expenses and resource consumption. It is currently recognized as a payment method that provides better control over the impact of hospitalization[6]. This study performed multidimensional factor analysis on big data from hospitals to reveal the composition and determinants of hospitalization costs for patients undergoing surgical treatment for liver and pancreatic cancers. These findings highlight the significant impact of the CHS-DRG system on China’s medical care system.
Statistical analysis revealed significant differences in hospital costs and length of stay between liver resection and pancreatectomy within the HB1 subgroups (HB11, HB13, and HB15). Particularly, the cost of pancreatic surgery was found to exceed that of liver surgery. Pancreatic surgery is widely recognized in clinical practice as one of the most challenging general surgeries, with a high risk of complications. Surgical approaches vary depending on the location of the disease and range from complex radical pancreaticoduodenectomy (such as the Whipple operation) to robotic procedures. These operations are associated with high technical complexity and high treatment costs.
The current CHS-DRG grouping scheme has limitations because it combines pancreatic and liver surgery, making it challenging to accurately assess the complexity of pancreatic surgery and its associated clinical resource consumption. This grouping also results in pancreatic surgery being categorized as a more cost-effective liver surgery, which affects the cost standards for pancreatic surgery and hinders progress in clinical technology. To address this issue, it has been proposed that liver and pancreatic surgeries be grouped separately based on their characteristics. Alternatively, pancreatic surgery can be grouped separately, with further refinement based on specific surgical methods to better capture the complexity and resource requirements of each procedure. By accurately reflecting the treatment complexity and resource requirements of different surgeries, the value of clinical services can be maximized, ultimately increasing the enthusiasm for clinical services. Regular review, adjustment of details concerning the grouping plan, and holding discussions about it is recommended to ensure alignment with evolving medical technology and clinical practice. Additionally, clinical experts should be involved in assessing its adaptability and scientific validity. This will help ensure that the CHS-DRG grouping plan remains in sync with clinical progress.
With the continuous development of new clinical diagnostic and treatment technologies, using medical devices has become increasingly widespread. Strengthening the oversight of healthcare materials is essential to manage increasing costs[7]. According to surveys, DRG payments can reduce the overall cost of drugs for patients[8]. Statistical analysis of the composition of hospital costs in various subgroups of HB1 cases showed that drugs and supplies accounted for over 70% of the total costs. Specific analysis revealed that pancreaticoduodenectomy had the highest proportion of drug costs within each subgroup (HB11, HB13, and HB15 disease groups). The complexity of the procedure appears to be closely related to severe complications and the subsequent increase in drug costs; the group with severe complications (HB11) had the highest drug costs and a higher proportion of consumable costs. Drug costs for cases of serious surgical complications has significantly increased. Patients who underwent liver resection had the highest consumption costs. However, medical, administrative, and medical technology expenses account for a relatively low proportion, while consumable expenses such as drugs and consumables account for a relatively high proportion. Consequently, differences exist between the original intentions of the current medical care reform and the medical insurance benefit reform policies. The CHS-DRG aims to save medical resources, reduce treatment costs, and reduce unnecessary resource waste.
At the hospital’s internal management level, it is suggested that medical and insurance departments work with clinical departments to develop clinical pathways for specific diseases based on DRG disease groups and various surgical techniques. The implementation of clinical pathways has been proven to reduce patient hospitalization costs, reduce length of stay, and enhance medical care efficiency[9]. Improving the monitoring of the consumption of drugs and supplies, promoting the appropriate clinical use of these resources, and discouraging unnecessary tests and treatments to reduce hospitalization costs, is recommended to optimize medical resource allocation, and maximize benefits. It is also recommended that payment standards for complex pancreaticoduodenectomy and/or shunt surgery within the DRG group for pancreatic procedures should improve, particularly for pancreaticoduodenal surgery, and that a flexible adjustment mechanism for payment standards be established. Furthermore, it is recommended that the medical service department and medical insurance collaborate with clinical departments to develop clinical pathway management for relevant diseases. They must monitor the use of drugs and supplies, promote rational clinical practices, reduce unnecessary tests and treatments, reduce hospitalization costs, and optimize the allocation of medical resources to maximize efficiency and benefits.
Analysis of the total hospitalization costs and length of stay in the three HB1 subgroups revealed that severe complications were more common after pancreatic and liver resection and/or shunt surgery than in patients with general complications or those without complications (subgroups HB3 and HB5). Patients with HB11 disease (subgroup HB11) incurred significantly higher costs and had longer hospital stays. Although advances in surgical techniques have decreased perioperative mortality following pancreatectomy, the incidence of complications remains high[10]. Studies have reported perioperative complication rates of 25%–40%[11]. Preventing and effectively managing serious complications are essential for reducing patients’ length of hospital stay, costs, and postoperative recovery quality. Medical departments should establish appropriate standards and indicators for patients undergoing pancreatectomy and liver resection, conduct thorough preoperative assessments, execute precise surgical procedures, closely monitor postoperative progress, and implement robust perioperative management strategies. Tailored cost estimates and prognoses are critical for patients with severe complications or comorbidities.
To reduce the costs of drugs and medical consumables, emphasis should be placed on the use of centrally procured medicines and consumables by the state while ensuring clinical effectiveness. Implementing a system of evaluation indicators, introducing performance appraisal, adopting a risk-adjustment model, and considering the impact of serious complications and comorbidities on costs can help achieve a more equitable and rational cost structure. Through these measures, clinical departments can raise their awareness of its importance, improve their level of management, and better plan their medical resources.
Under the CHS-DRG payment system, hospital costs are influenced by factors such as the complexity of surgery and the presence of serious complications or comorbidities. By refining the CHS-DRG grouping scheme with the help of improved management, technological advancements, and personalized assessments, we can more effectively address the specific requirements for treating liver and pancreatic cancers. This approach is expected to help manage hospitalization costs appropriately without compromising medical quality. Continued research and practical implementation will contribute to enhancing the CHS-DRG payment system and ultimately improving the efficiency and equity of medical services.
| 1. | National Healthcare Security Administration. Notice on issuing the national pilot technical specifications and grouping plan for payment of disease diagnosis related groups (DRGs), (YiBaoBan Fa [2019] No. 34). Oct 24, 2019. [cited 6 June 2022]. Available from: http://www.nhsa.gov.cn/art/2019/10/24/art_104_6464.html. |
| 2. | Liu F, Panagiotakos D. Real-world data: a brief review of the methods, applications, challenges and opportunities. BMC Med Res Methodol. 2022;22:287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 247] [Reference Citation Analysis (0)] |
| 3. | Chew XH, Sultana R, Mathew EN, Ng DCE, Lo RHG, Toh HC, Tai D, Choo SP, Goh BKP, Yan SX, Loke KSH, Thang SP, Gogna A, Venkatanarasimha NK, Tong AKT, Moe FNN, Chua JSS, Ang RWT, Ong AD, Ng AWY, Hoang MTQ, Too CW, Thng CH, Chan WY, Kee W, Chan JHM, Irani F, Leong S, Lim KH, Wang MLC, Chow PKH. Real-World Data on Clinical Outcomes of Patients with Liver Cancer: A Prospective Validation of the National Cancer Centre Singapore Consensus Guidelines for the Management of Hepatocellular Carcinoma. Liver Cancer. 2021;10:224-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, Li L, Wei W, He J. Cancer incidence and mortality in China, 2022. J Natl Cancer Cent. 2024;4:47-53. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 1211] [Article Influence: 605.5] [Reference Citation Analysis (0)] |
| 5. | Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2279] [Cited by in RCA: 6031] [Article Influence: 3015.5] [Reference Citation Analysis (4)] |
| 6. | Liu R, Shi J, Yang B, Jin C, Sun P, Wu L, Yu D, Xiong L, Wang Z. Charting a path forward: policy analysis of China's evolved DRG-based hospital payment system. Int Health. 2017;9:317-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Zhang H, Hu H, Wu C, Yu H, Dong H. Impact of China's Public Hospital Reform on Healthcare Expenditures and Utilization: A Case Study in ZJ Province. PLoS One. 2015;10:e0143130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Bala MV, Zarkin GA. Application of cost-effectiveness analysis to multiple products: a practical guide. Am J Manag Care. 2002;8:211-218. [PubMed] |
| 9. | Yuan S, Liu W, Wei F, Zhang H, Wang S, Zhu W, Ma J. Impacts of Hospital Payment Based on Diagnosis Related Groups (DRGs) with Global Budget on Resource Use and Quality of Care: A Case Study in China. Iran J Public Health. 2019;48:238-246. [PubMed] |
| 10. | Bentrem DJ, Yeh JJ, Brennan MF, Kiran R, Pastores SM, Halpern NA, Jaques DP, Fong Y. Predictors of intensive care unit admission and related outcome for patients after pancreaticoduodenectomy. J Gastrointest Surg. 2005;9:1307-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Bassi C, Butturini G, Molinari E, Mascetta G, Salvia R, Falconi M, Gumbs A, Pederzoli P. Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg. 2004;21:54-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 231] [Article Influence: 10.0] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/