Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4199
Revised: May 10, 2024
Accepted: May 29, 2024
Published online: July 16, 2024
Processing time: 83 Days and 16.3 Hours
Gustilo III fractures have a high incidence and are difficult to treat. Patients often experience difficulty in wound healing. Negative pressure drainage technology can help shorten wound healing time and has positive value in improving patient prognosis.
To explore the clinical value of the negative pressure sealing drainage technique in wound healing of Gustilo IIIB and IIIC open fractures.
Eighty patients with Gustilo IIIB and IIIC open fractures with skin and soft tissue injuries who were treated in the Second People’s Hospital of Dalian from March 2019 to December 2021 were selected as the research subjects. They were divided into a study group (n = 40, healed with negative pressure closed drainage) and a control group (n = 40, healed with conventional dressing changes) according to the variation in the healing they received. The efficacy of the clinical interventions, the variations in the regression indicators (time to wound healing, time to fracture healing, time to hospitalization), and the conversion and healing of bacterial wounds were compared 1-3 mo after the intervention.
The total effective rate of patients among the study group was 95.00% (38/40), which was notably higher than 75.00% (30/40) among the control group (P < 0.05). The wound healing time, fracture healing time, and hospital stay of the patients in the study group was shorter than the control group (P < 0.05). After the intervention, the negative bacterial culture at the wound site rate and wound healing rate of the patients among the study group increased compared to the control group (P < 0.05).
Negative pressure sealing and drainage technology has a good therapeutic effect on patients with Gustilo IIIB and IIIC open fracture wounds with skin and soft tissue injury. It can notably enhance the wound healing rate and the negative rate of bacteria on the wound surface and help to speed up the recovery process of patients.
Core Tip: Negative pressure sealing drainage technology can improve the treatment effect of Gustilo IIIB and IIIC open fracture wounds with skin and soft tissue damage. It can accelerate the patient recovery process and improve the wound healing rate.
- Citation: Fang B, Wang YS, Li W, Ying K, Zong G. Value of negative pressure sealing drainage on wound healing of Gustilo IIIB and IIIC open fractures. World J Clin Cases 2024; 12(20): 4199-4205
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4199.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4199
With the continuous development of China’s transportation industry and construction industry, Gustilo III fractures caused by high energy have shown an increasing trend year by year[1]. Such fractures often lead to soft tissue defects, and most of them will damage the nerves and blood vessels of patients. In severe cases, there may even be limb damage, which is more difficult to treat, and patients have an increased risk of nonunion or bone infection[2,3]. Both Gustilo IIIB and Gustilo IIIC fractures belong to the more serious types of open fractures. Such patients have large fractures and severe injuries and are prone to infection after surgery because of the large number of dead spaces[4].
Negative pressure sealing drainage technology is a mature intervention measure developed in recent years in the treatment of difficult to heal wounds, especially for open fractures with concurrent soft tissue defects or vascular injuries. Controlled studies have found that applying negative pressure sealing drainage technology to complex fracture patients can significantly reduce wound infection rates, shorten wound healing time, and improve patient prognosis[5]. In addition, controlled studies have found that negative pressure drainage can reduce postoperative pain in patients with open fractures and have a positive significance in improving local bacterial conversion rates[6]. This study aimed to explore the intervention effect of negative pressure sealing drainage technology on the wound healing of Gustilo IIIB and Gustilo IIIC fractures by setting up a control group in order to provide clinical reference for improving the prognosis of such patients.
Eighty patients with Gustilo IIIB and IIIC open fractures with skin and soft tissue injuries who were treated in the Second People’s Hospital of Dalian from March 2019 to December 2021 were selected as the research subjects. They were divided into the study group (n = 40, received negative pressure closed drainage therapy) and the control group (n = 40, received routine dressing change therapy). This survey was approved by the hospital ethics committee for implementation.
Inclusion criteria were as follows: (1) Those with a clear history of trauma, diagnosed as Gustilo IIIB and IIIC open fractures by imaging examination, and accompanied by obvious skin and soft tissue damage; (2) Complete medical records; (3) Appropriate for injury identification limb salvage operators; and (4) Increased body temperature and blood count, pain around the wound, purulent secretions on the wound surface connected with the fracture site, and positive bacterial culture of the secretions.
Exclusion criteria were as follows: (1) Patients with psychiatric disorders; (2) Patients with functional muscle damage resulting in inability to carry out repair and reconstruction; (3) Patients with malignant tumors; (4) Patients who lost the opportunity for limb salvage surgery; and (5) Incomplete clinical data.
Both groups of patients were first subjected to conventional debridement, and the fractures were fixed with an external fixator after thorough debridement. For those with bone defect or exposed bone, all inactivated and severely polluted small bone fragments and large bone fragments were removed while keeping as much as possible. Nerve, blood vessel, and tendon repair surgery was performed on patients as needed. After thorough debridement, patients needed to receive nutritional support healing. At the same time, the corresponding antibiotics according to the preoperative bacterial culture test of the patients were selected, and patients were directed to carry out functional exercise as soon as possible.
The patients in the study group used negative pressure sealing and drainage dressings for wound repair. The dressings were cut to an appropriate size to make them fully contact with the wound and then sutured and fixed around the wounds. At the same time, a transparent film with unidirectional ventilation was used to seal the negative pressure sealing and drainage dressing with a multi-hole drainage tube and the skin around the wound. It was connected to the central negative pressure suction and drainage bottle with negative pressure at -125 to -450 mmHg. The drainage fluid was recultured 4-5 d and 7-10 d after the operation. Then, the negative pressure sealing and drainage dressing was removed, and it was decided whether it was necessary to re-debride and use the negative pressure sealing and drainage. If the bone tissue was exposed and blackened, the necrotic bone tissue was moderately removed, and then the muscle flap transfer was performed. The skin graft was performed after the muscle flap survived.
The patients among the control group were treated with routine excipients, and the necrotic tissue, pus, foreign bodies, etc. of the patients were removed each time the dressing was changed. In the early stage of dressing change, patients often had granulation tissue growth and edema. Fresh granulation tissue could be found after several dressing changes. Then, the muscle flap transfer was performed, and skin grafting was performed after the muscle flap survived.
The effective rate of healing in the two groups of patients was evaluated based on the skin graft healing area/skin graft area × 100% at 20 d after the operation. The data showed that the data reached more than 85%, the effective rate was 60%-85%, and the ineffective rate was 60%. The wound healing time, fracture healing time, negative bacterial culture at the wound site rate, and hospitalization time of the two groups of patients were compared.
The Mann-Whitney U test was used to analyze the non-parametric data expressed as median (upper and lower quartiles), and the measurement data was analyzed by the χ2 test, which was expressed as cases (%). P < 0.05 was considered significant.
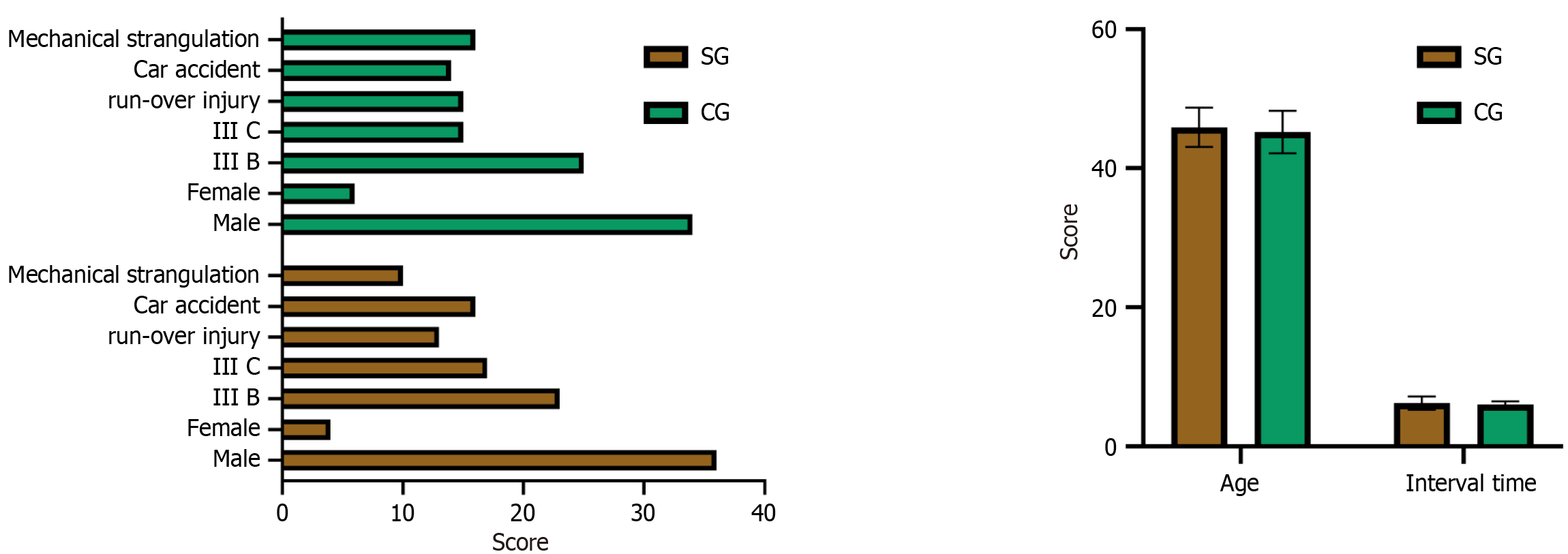
The sex, age, fracture type, fracture cause, healing interval, and other general clinical data of the two groups of patients was not significantly different between the two groups (P > 0.05), indicating that the two groups were comparable (Table 1 and Figure 1).
| General clinical information | Study group, n = 40 | Control group, n = 40 | t/χ2 | P value | |
| Sex | Male | 36 | 34 | 0.457 | 0.499 |
| Female | 4 | 6 | |||
| Mean age in yr | 45.90 ± 2.82 | 45.24 ± 3.05 | 1.005 | 0.318 | |
| Time between healings in h | 6.24 ± 0.95 | 6.01 ± 0.47 | 1.432 | 0.156 | |
| Degree of injury | IIIB | 23 | 25 | 0.208 | 0.648 |
| IIIC | 17 | 15 | |||
| Cause of injury | Crush injuries | 13 | 15 | 0.365 | 0.554 |
| Car accident injuries | 16 | 14 | |||
| Machine strangulation | 10 | 16 | |||
| Other | 1 | 5 | |||
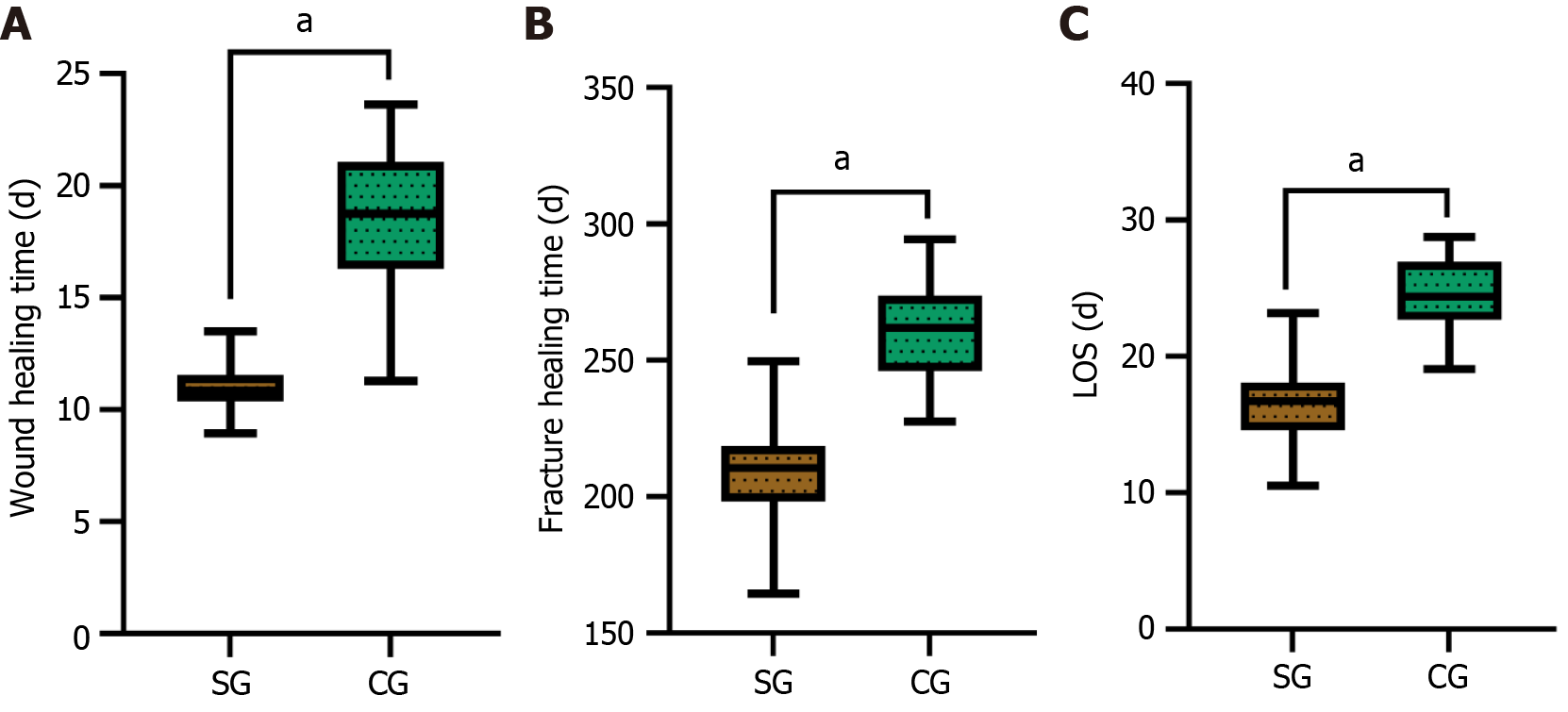
The wound healing time, fracture healing time, and hospitalization time of the patients among the study group were significantly shorter than those among the control group (P < 0.05) (Table 2 and Figure 2).
| Group | Cases | Wound healing time in d | Fracture healing time in d | Length of stay in hospital in d |
| Study group | 40 | 10.94 ± 0.99 | 209.41 ± 16.00 | 16.59 ± 2.78 |
| Control group | 40 | 18.50 ± 3.13 | 261.96 ± 17.66 | 24.40 ± 2.68 |
| t | - | 14.565 | 13.947 | 12.792 |
| P value | - | < 0.001 | < 0.001 | < 0.001 |
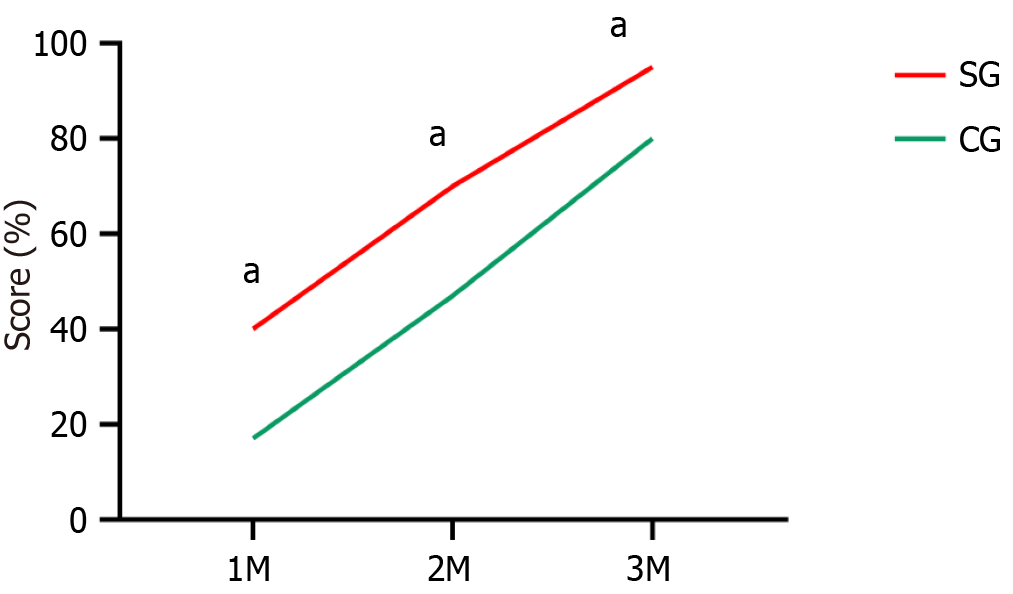
Statistics showed that the negative bacterial culture at the wound site rates of the study group 1 month, 2 months, and 3 months after the operation were 40.00%, 70.00%, and 95.00%, respectively, which were significantly increased compared to the control group (17.50%, 47.50%, and 80.00%, respectively) (P < 0.05) (Table 3 and Figure 3).
| Group | Cases | 1 month | 2 months | 3 months |
| Study group | 40 | 16 (40.00) | 28 (70.00) | 38 (95.00) |
| Control group | 40 | 7 (17.50) | 19 (47.50) | 32 (80.00) |
| χ2 | - | 4.943 | 4.178 | 4.114 |
| P value | - | 0.026 | 0.041 | 0.043 |
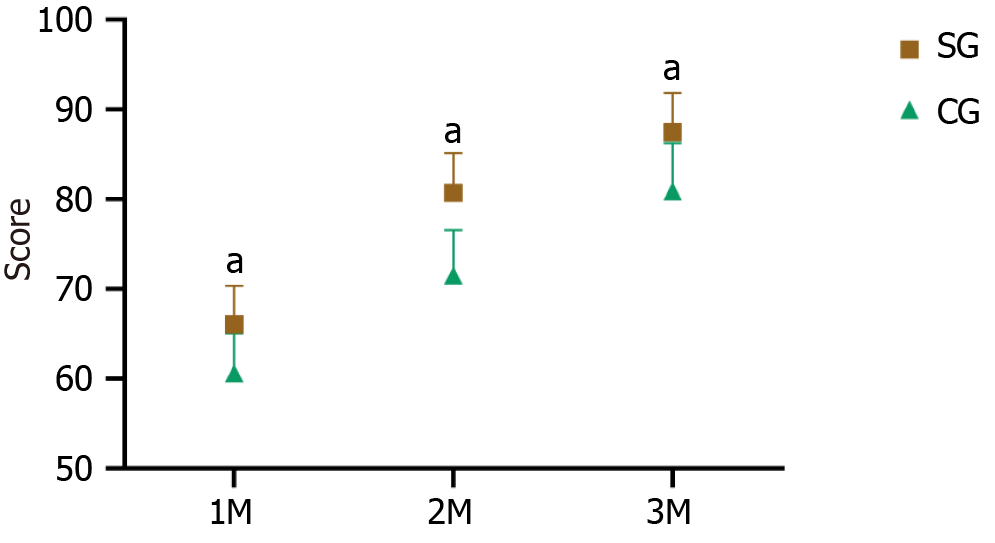
The injured limbs of the two groups of patients were marked after the operation using Puno criteria. The Puno injured limb marks of the patients in the study group were significantly increased compared to the study group (P < 0.05) (Table 4 and Figure 4).
| Group | Cases | 1 month | 2 months | 3 months |
| Study group | 40 | 66.06 ± 4.29 | 80.72 ± 4.41 | 87.49 ± 4.38 |
| Control group | 40 | 60.61 ± 4.46 | 71.54 ± 5.01 | 80.88 ± 5.39 |
| t | - | 5.570 | 8.699 | 6.019 |
| P value | - | < 0.001 | < 0.001 | < 0.001 |
The bone healing and functional recovery of injured limbs depend on the healing of their bone and soft tissue injuries[7]. The bone healing and functional recovery of injured limbs in patients with open fractures combined with soft tissue injuries depend on the management of their bone and soft tissue injuries. Only by considering early management of both can it contribute to the patient’s treatment. Therefore, the key points for the management of open fractures also includes when to cover the wound, how to cover the wound, etc[8,9].
A Gustilo type III open fracture is a severe trauma caused by high-energy external force, and it is a very unstable fracture type[10]. In recent years, with the use of modern tools, the incidence of Gustilo type III fractures has gradually increased[11]. These patients are often accompanied by extensive soft tissue damage and loss and are accompanied by serious pollution, which should be considered during treatment. Damaged bone also needs to be considered regarding deactivated soft tissue[12].
Gustilo IIIB and IIIC open fractures were analyzed by setting up a control group. The patients in the drainage study group had a notably shorter wound healing time, fracture healing time, and hospital stay, suggesting that negative pressure sealing drainage can speed up the recovery process of patients with Gustilo type III fractures. A study of 31 patients with chronic refractory wound infection after Gustilo type III open fractures found that after applying negative pressure sealing and drainage technology to treat the wound, the wound infection of the patients was notably controlled, the edema was notably reduced, and fresh granulation appeared. The wound area after the tissue was reduced by 15%-20%, and the bacterial culture was positive. After the negative pressure sealing and drainage healing, the patients were followed up for 6 mo, and the wound healed without reinfection[13]. Another study on 30 patients with Gustilo IIIB and Gustilo IIIC fractures who received negative pressure sealing and drainage within 8 h after surgery found that the wound healing time of 29 patients was 25-40 d, with an average of 27 d, and the skin grafts survived. The rates were excellent, and the degree of skin recovery was good. Only one case had postoperative infection and bone exposure, which enhanced after active healing[14].
The above studies all suggested that negative pressure sealing drainage had good application value in Gustilo type III open fractures. Creating a hypoxic or slightly hypoxic acid environment inhibits the growth of bacteria on the wound surface[15]. At the same time, the continuous drainage of necrotic tissue and secretions notably reduces the medium required for bacterial reproduction and can quickly enhance the wound infection of patients[16]. In addition, negative pressure sealing drainage also helps to increase the levels of interleukin 8 and vascular endothelial growth factor in local tissues. This accumulates neutrophils and accelerates angiogenesis, which helps to enhance the local microcirculation of wounds and provide sufficient nutrient supply for wound repair.
Moreover, the negative pressure environment can also bring a certain mechanical traction effect to the tissue, which can induce tissue cell proliferation. This promotes the growth of wound granulation tissue[17,18]. In the end, the joint function of the two groups of patients was compared. The Puno injured limb marks of the patients among the study group were higher than those among the control group during the postoperative follow-up period. The effective control of infection enables patients to carry out rehabilitation activities as soon as possible, which lays a good foundation for the recovery of their limb functions.
In summary, negative pressure sealing drainage technology has a good therapeutic effect on patients with Gustilo IIIB and IIIC open fracture wounds accompanied by skin and soft tissue injuries. It can significantly improve the wound healing rate and negative bacterial culture at the wound site rate, helping to accelerate the patient’s recovery process. The shortcomings of this study were that it was a retrospective study and the small sample size of included patients. Long-term follow-up of patients was not conducted. In the future, targeted large sample, multicenter randomized prospective studies are planned to improve the applicability of the results.
| 1. | Garner MR, Sethuraman SA, Schade MA, Boateng H. Antibiotic Prophylaxis in Open Fractures: Evidence, Evolving Issues, and Recommendations. J Am Acad Orthop Surg. 2020;28:309-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 2. | Tian R, Zheng F, Zhao W, Zhang Y, Yuan J, Zhang B, Li L. Prevalence and influencing factors of nonunion in patients with tibial fracture: systematic review and meta-analysis. J Orthop Surg Res. 2020;15:377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 127] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 3. | Rupp M, Popp D, Alt V. Prevention of infection in open fractures: Where are the pendulums now? Injury. 2020;51 Suppl 2:S57-S63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 4. | Riechelmann F, Kaiser P, Arora R. [Primary soft tissue management in open fracture]. Oper Orthop Traumatol. 2018;30:294-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Huang CG, Jia ZG, Gu ZQ, Zhao P, Lyu GZ. [Clinical effects of vacuum sealing drainage in the treatment of alkali burn wounds]. Zhonghua Shao Shang Za Zhi. 2020;36:534-539. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Wang A, Ma WG, Wang CD, Zhang HQ, Liu F. [Clinical effects of autologous platelet rich plasma gel combined with vacuum sealing drainage techno-logy in repairing refractory wounds]. Zhonghua Shao Shang Za Zhi. 2021;37:42-48. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Lin CA, O'Hara NN, Sprague S, O'Toole RV, Joshi M, Harris AD, Warner SJ, Johal H, Natoli RM, Hagen JE, Jeray KJ, Fowler JT, Phelps KD, Pilson HT, Gitajn IL, Bhandari M, Slobogean GP; the PREP-IT Investigators. Low Adherence to Recommended Guidelines for Open Fracture Antibiotic Prophylaxis. J Bone Joint Surg Am. 2021;103:609-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Foote CJ, Tornetta P 3rd, Reito A, Al-Hourani K, Schenker M, Bosse M, Coles CP, Bozzo A, Furey A, Leighton R; GOLIATH Investigators. A Reevaluation of the Risk of Infection Based on Time to Debridement in Open Fractures: Results of the GOLIATH Meta-Analysis of Observational Studies and Limited Trial Data. J Bone Joint Surg Am. 2021;103:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | McMahon HA, Stranix JT, Lee ZH, Levine JP. Management of Gustilo Type IIIC Injuries in the Lower Extremity. Clin Plast Surg. 2021;48:267-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Horton SA, Hoyt BW, Zaidi SMR, Schloss MG, Joshi M, Carlini AR, Castillo RC, O'Toole RV. Risk factors for treatment failure of fracture-related infections. Injury. 2021;52:1351-1355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Sagi HC, Patzakis MJ. Evolution in the Acute Management of Open Fracture Treatment? Part 1. J Orthop Trauma. 2021;35:449-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Hand TL, Hand EO, Welborn A, Zelle BA. Gram-Negative Antibiotic Coverage in Gustilo-Anderson Type-III Open Fractures. J Bone Joint Surg Am. 2020;102:1468-1474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Higgin R, Dean M, Qureshi A, Hancock N. Outcomes following the delayed management of open tibial fractures. Injury. 2021;52:2434-2438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Tan WJ, Kwek EBK. Outcomes after implementation of an open fracture clinical pathway. Arch Orthop Trauma Surg. 2020;140:1373-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Mener A, Staley C, Boissonneault A, Reisman W, Schenker M, Hernandez-Irizarry R. Infection After Open Long Bone Fractures: Can We Improve on Prophylaxis? J Surg Res. 2021;268:33-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Duan H, He Y, Zhang H, Wang F, Chen S, Wang J. Vacuum sealing drainage with instillation in the treatment of necrotising soft-tissue infection: a retrospective analysis. J Wound Care. 2020;29:510-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Li J, Shi JB, Hong P, Wang YS, Ze HR, Lee RJ, Tang X. Combined treatment with vacuum sealing drainage, TopClosure device, and Ilizarov technique for traumatic hemipelvectomy: A rare case report of successful repairing of large-size soft tissue defects. Medicine (Baltimore). 2019;98:e14205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Huang Q, Huang K, Xue J. Vacuum sealing drainage combined with free anterolateral femoral skin flap grafting in 16 cases of pediatric soft tissue damage to the foot and ankle. Transl Pediatr. 2021;10:2489-2495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/