Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.3837
Revised: April 30, 2024
Accepted: May 16, 2024
Published online: July 6, 2024
Processing time: 121 Days and 2.2 Hours
The prominent symptoms of chronic pelvic pain syndrome (CPPS) are urogenital pain, lower urinary tract symptoms, psychological problems, and sexual dysfunction. Traditional pharmacological treatments have poor efficacy and more untoward reaction and complications. Magnetic vibration magnetoelectric therapy is a non-invasive form of physiotherapy. Nevertheless, its effectiveness in improving urinary discomfort and relieving pain in patients requires further exploration.
To investigate the clinical efficacy of the magnetic vibration magnetoelectric therapy instrument in the treatment of chronic prostatitis (CP)/ CPPS.
Seventy patients with CP/CPPS were collected from the outpatient clinic and ward of the Department of Male Medicine, Jiangsu Province Hospital of Traditional Chinese Medicine, and were treated with magnetic vibration magne
The total effective rate of treatment was 58.5%, and the total NIH-CPSI score, pain symptoms, voiding symptoms, quality of life, IIEF-5, PEDT, GAD, PCS and TCMS scores all decreased significantly (P < 0.05).
Magnetic vibration magnetotherapy is effective in improving urinary discomfort, relieving pain, improving quality of life, improving sexual dysfunction and relieving negative emotions such as anxiety in patients with CP/CPPS.
Core Tip: This study focuses on male in-and out-patients at Jiangsu Provincial Hospital of Traditional Chinese Medicine to evaluate the therapeutic effect of Magnetic vibration magnetoelectric therapy on chronic prostatitis (CP)/chronic pelvic pain syndrome (CPPS). Our research shows that it was effective in improving symptoms in patients with CP/CPPS symptoms, accommodating sexual dysfunction in some patients, and relieving negative emotions in others. This progress not only considers magnetoelectric therapy as an alternative treatment modality but also emphasizes the significance of non-invasive methods in improving patient outcomes within the field of pain and emotion therapy.
- Citation: Zhang ZH, Chang FJ, Chen Y. Clinical efficacy of magnetic vibration magnetoelectric therapy in the treatment of chronic prostatitischronic pelvic pain syndrome. World J Clin Cases 2024; 12(19): 3837-3844
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/3837.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.3837
Chronic prostatitis (CP)/chronic pelvic pain syndrome (CPPS) is a common condition in men, and approximately half of all affected patients have a history of infection[1]. Symptoms associated with the prostate are more predominant in Asia than in other regions[2]. CP/CPPS is treated in various ways, including medication, physiotherapy, and surgery; however, these treatments do not completely address patient concerns, and treatment using new technologies and methods is warranted. Magnetic vibration magnetoelectric therapy is a non-invasive form of physiotherapy that functions based on three principles: magnetic field effect, vibration, and electrical stimulation. In this study, we recruited out- and in-patients from the Department of Male Medicine of Jiangsu Provincial Hospital of Traditional Chinese Medicine to evaluate the therapeutic effect of magnetic vibration magnetotherapy on CP/CPPS.
Seventy patients attending our male outpatient clinics and wards between April 2021 and February 2022 were selected, all of whom met the guideline criteria for CP/CPPS. This study was approved by the ethics committee of Jiangsu Provincial Hospital of Traditional Chinese Medicine and was performed according to the Declaration of Helsinki. Informed, written consent was obtained from all patients.
Current diagnostic criteria: The following criteria were used to diagnose CP/CPPS according to the United Kingdom consensus guideline on diagnosis and treatment of chronic bacterial prostatitis and CP/CPPS[3]: (1) Pain or discomfort in the perineum, pubic bone, or groin; (2) urinary tract symptoms: Urinary frequency, urgency, incomplete urination, nocturia, or difficulty in urination; (3) sexual dysfunction: erectile dysfunction, premature ejaculation, or decreased libido; and (4) psychological problems: anxiety and depression.
Diagnostic criteria of traditional Chinese medicine: The following criteria were used to diagnose CP/CPPS according to the Chinese Association of Integrative Medicine consensus guideline on diagnosis and treatment of chronic bacterial prostatitis and CP/CPPS[4]: (1) Pain or discomfort in the perineum, testis, pubic bone, or groin; (2) urinary tract symptoms: urinary frequency, urgency, incomplete urination, odynuria, scorching hot symptom of the urinary tract, or difficulty in urination; and (3) inspection including tongue manifestation and pulse manifestation.
Inclusion criteria: (1) Male patients aged 21–72 years; (2) meeting guideline diagnostic criteria; (3) the main clinical manifestation was persistent or recurrent perineal or pelvic pain and discomfort for at least three of the past 6 months, which may have been accompanied by lower urinary tract symptoms and sexual dysfunction; (4) patients with a medical history of more than 3 months and who had not been administered any other medication for CP/CPPS within the previous week, including Western, Chinese, or proprietary Chinese medicines, and had not undergone physical or chemical treatment for chronic prostatitis; and (5) those who agreed and signed the informed consent form.
Exclusion criteria: (1) Age < 21 or > 72 years; (2) acute and chronic prostatitis caused by bacterial infection, recurrent and intractable lower urinary tract infections, acute and chronic orchitis or epididymitis, and sexually transmitted diseases; (3) patients with severe psychiatric abnormalities and serious chronic diseases; (4) metal implants in the body; (5) patients with previous urethral surgery or urethral strictures; (6) patients with local lesions or skin infections at the treatment site; and (7) patients who were allergic to electrical stimulation and magnetic therapy .
A physician first inspected the treatment instrument to ensure that the equipment was normal. The patient was then instructed to lie supine on the treatment bed and remain relaxed. The physician disinfected the magnetic vibration treatment head with alcohol cotton balls, placed the small head of the magnetic vibration treatment head on the perineum and the other on the top of the pubic symphysis. The patient's bilateral Sanyinjiao and Sansili acupuncture points were disinfected using alcohol cotton balls. Then, disposable electrode pads were placed on the four magnetic heads, which were placed on the bilateral Sanyinjiao and Sansili acupoints. Patients were instructed by the physician to use the treatment once a day for 14 d. During the treatment period, the patient was required to follow the doctor's instructions to refrain from smoking and drinking, eat a healthy diet, exercise, avoid sitting for long periods of time, and hold urine.
After 14 d of treatment, health-chronic prostatitis symptom index (NIH-CPSI), international index of erectile function 5 (IIEF-5), premature ejaculation diagnostic tool (PEDT), generalized anxiety disorder (GAD), Patient Health Questionnaire (PHQ), pain catastrophizing scale (PCS) and traditional Chinese medicine syndrome (TCMS) assessments were performed on patients before and after treatment. Total treatment efficiency, total NIH-CPSI scores, pain symptoms, voiding symptoms, quality of life (QoL) scores, IIEF-5, PEDT, GAD, PHQ, PCS and TCMS scores, before and after treatment, were compared. Adverse reactions and events were recorded to evaluate the safety level.
The following were considered as judgement criteria: Cure, NIH-CPSI score decreased by ≥ 90%; excellence, NIH-CPSI score decreased by ≥ 70% but < 90% compared to the pre-treatment level; Effective, NIH-CPSI score decreased by ≥ 30% but < 70% compared to the pre-treatment level; Ineffective, NIH-CPSI score decreased by < 30% compared to the pre-treatment level.
Statistical analysis was performed using Graphpad Prism statistical software (version 8.0). Measurement data were expressed as mean ± SD and a t-test was used. P ≤ 0.05 was considered statistically significant.
A total of 70 patients were included, of whom five were excluded as they were unable to participate throughout the study for personal reasons. The total effective rate of patients treated with the magnetic vibration magnetotherapy device was 58.5% and no adverse events occurred (Table 1).
| Cure | Excellence | Effective | Ineffective | Total effectiveness | |
| N | 0 | 3 | 35 | 27 | 38 |
| Percentage | 0 | 4.6 | 53.8 | 41.5 | 58.5 |
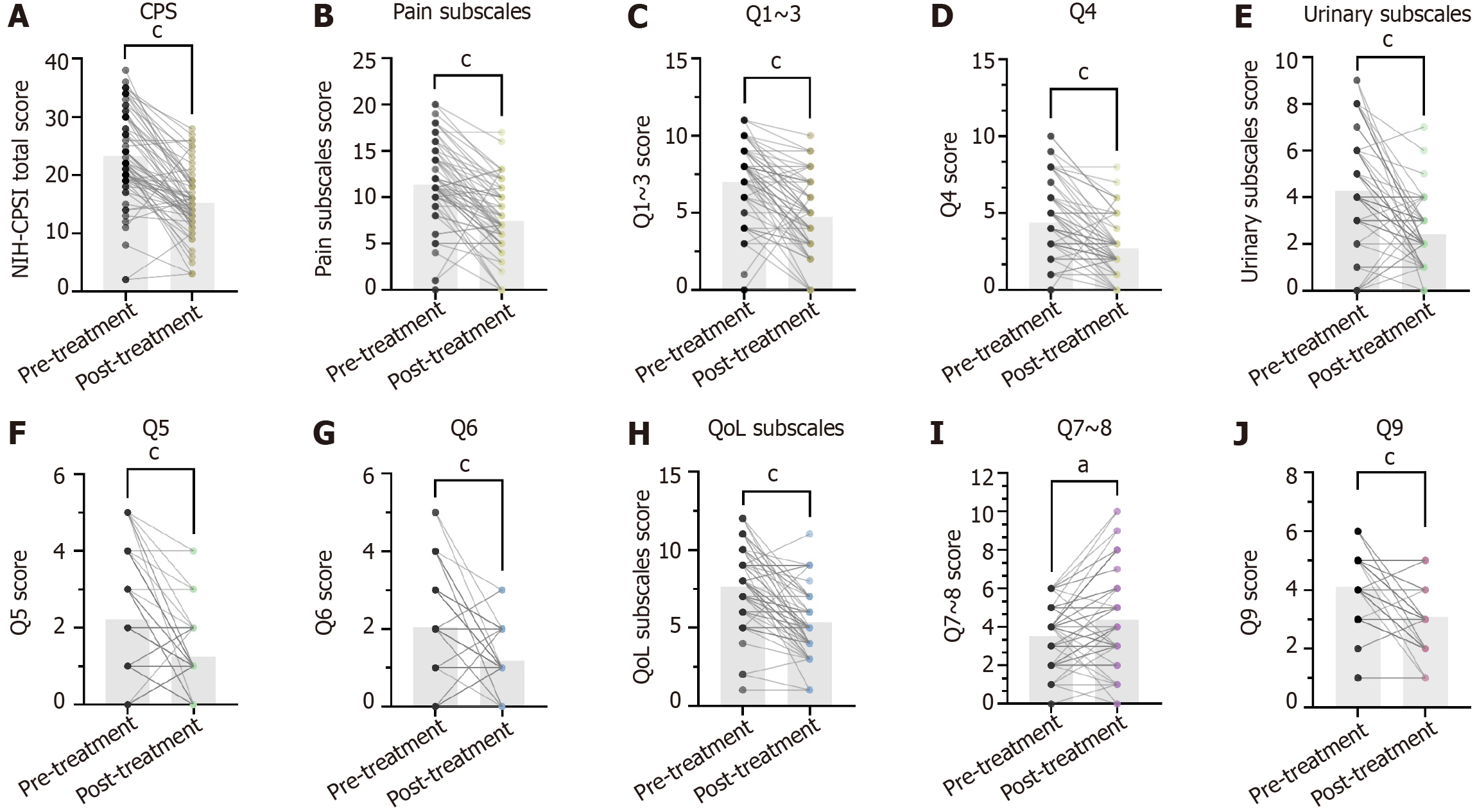
Patients showed a statistically significant decrease in total NIH-CPSI, pain symptoms, voiding symptoms, and quality of life scores before and after treatment (P < 0.05) (Table 2, Figure 1).
| Parameter | Pre-treatment (n = 65) | Post-treatment (n = 65) | P value |
| NIH-CPSI, (mean ± SD) | |||
| Total score | 23.29 ± 7.89 | 15.23 ± 5.67 | P < 0.001 |
| Pain subscales | 11.38 ± 4.61 | 7.45 ± 3.93 | P < 0.001 |
| Q1-3 | 7 ± 2.67 | 4.74 ± 2.59 | P < 0.001 |
| Q4 | 4.38 ± 2.51 | 2.71 ± 1.79 | P < 0.001 |
| Urinary subscales | 4.26 ± 2.35 | 2.43 ± 1.32 | P < 0.001 |
| Q5 | 2.22 ± 1.49 | 1.25 ± 0.9 | P < 0.001 |
| Q6 | 2.05 ± 1.3 | 1.18 ± 0.73 | P < 0.001 |
| QoL subscales | 7.65 ± 2.41 | 5.35 ± 2.16 | P < 0.001 |
| Q7-8 | 3.54 ± 1.56 | 4.38 ± 2.51 | P = 0.0012 < 0.01 |
| Q9 | 4.11 ± 1.08 | 3.08 ± 1.15 | P < 0.001 |
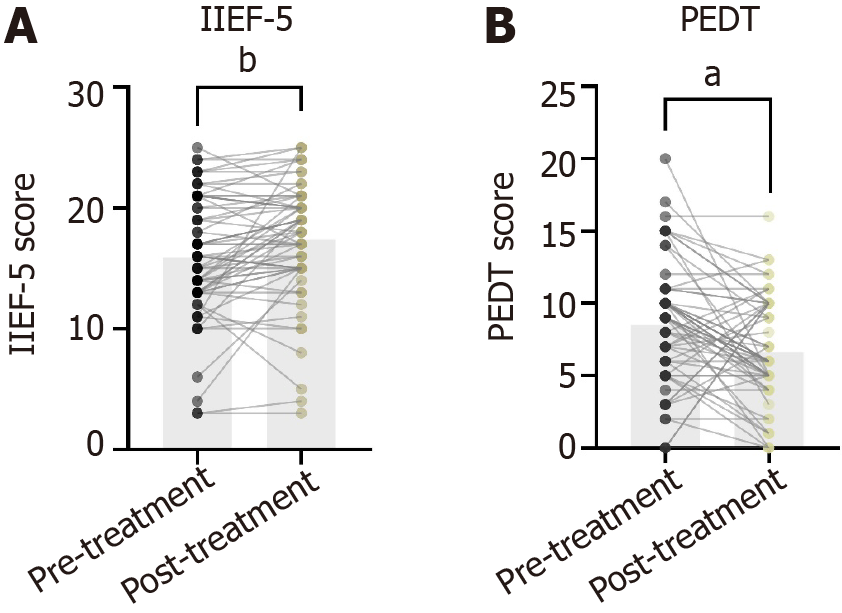
Patients' IIEF-5 and PEDT scores decreased and the difference were statistically significant (P < 0.05) (Table 3, Figure 2).
| Pre-treatment | Post-treatment | P value | |
| IIEF-5, (mean ± SD) | 15.92 ± 5.02 | 17.14 ± 4.81 | P = 0.0005 < 0.001 |
| PEDT, (mean ± SD) | 8.51 ± 4.31 | 6.63 ± 3.63 | P = 0.001 < 0.05 |
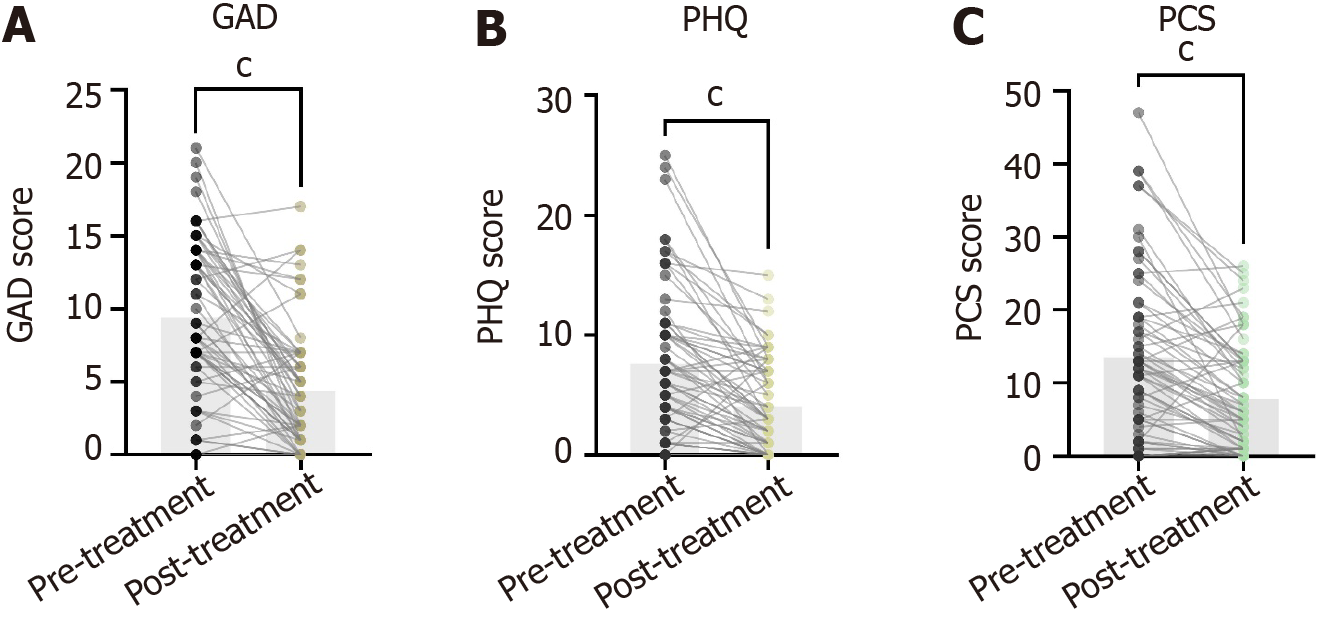
GAD, PHQ, and PCS scores decreased before and after treatment, with statistically significant differences in these scores (Table 4, Figure 3).
| Parameter | Pre-treatment | Post-treatment | P value |
| GAD, (mean ± SD) | 9.4 ± 5.52 | 4.38 ± 4.1 | P < 0.001 |
| PHQ, (mean ± SD) | 7.65 ± 6.3 | 4.05 ± 3.9 | P < 0.001 |
| PCS, (mean ± SD) | 13.55 ± 11.43 | 7.83 ± 7.42 | P < 0.001 |
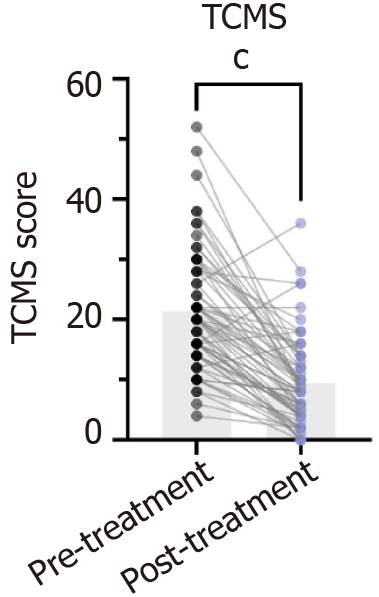
TCMS score were composed of three parts: lower urinary tract symptoms, radiating pain, inspection including tongue manifestation and pulse manifestation. According to three standards: None, medium and often, the scores are 0, 2, 4. The more points scored, the more severe the symptoms become, with a total score of 56 points. TCMS score decreased and the difference was statistically significant (P < 0.001) (Table 5, Figure 4).
| Parameter | Pre-treatment | Post-treatment | P value |
| TCMS, (mean ± SD) | 21.35 ± 10 | 9.42 ± 7.4 | P < 0.001 |
CP/CPPS is a chronic condition characterised by genitourinary pain, lower urinary tract symptoms, psychological problems, and sexual dysfunction[5]. Owing to its high prevalence and ineffective pharmacological treatment, physiotherapy, which is characterised by fewer adverse effects, has gained popularity among patients[6]. Common physiotherapy modalities include myofascial release, therapeutic exercise, biofeedback, and electrical stimulation. Relevant studies have shown that physiotherapy alone was effective for improving CP/CPPS and patients' discomfort when combined with medication and other modalities[7]. Magnetic vibration magnetoelectric therapy is a new type of physiotherapy treatment that can effectively improve patients' discomfort by applying magnetic fields, vibration, and electrical stimulation to specific areas.
Magnetic therapy and electrotherapy are common physiotherapy modalities used for treating CP/CPPS. Additionally, Sanyinjiao and Sansanli are common acupuncture points used in clinical practice for treatment. The magnetic effect can influence hemodynamics within the body's blood vessels to improve local microcirculation, accelerate blood flow to the prostate tissue, and enhance tissue immunity by promoting immune cell infiltration. In a previous study, Kim et al[8] performed extracorporeal magnetic stimulation in men with CP/CPPS who did not respond to pharmacological treatment and discovered that it significantly improved the patients' pain and lower urinary tract symptoms. Electrotherapy is another effective and widely used treatment modality. Although electrical stimulation is not curative, it can relieve pain by altering the neural pathways that mediate it[9]. Extracorporeal electrical stimulation has been shown to be effective up to 70% of the time in patients with refractory CP/CPPS, without significant adverse effects, resulting in effective and safe treatment[10]. Based on traditional Chinese medical theory, Sanyinjiao and Sansili are acupuncture points commonly used for the treatment of CP/CPPS, which have the effects of benefiting Qi, regulating the meridians, regulating the bladder and draining Qi flow; additionally, Sansili tonifies Qi, infiltrates dampness, and induces diuresis. Therefore, electrical stimulation of the two acupoints can achieve the electroacupuncture effect, which improves immunity and effectively relieves symptoms such as prostatitis, erectile dysfunction, anxiety, and depression in patients with CP/CPPS[11]. Thus, the magnetic vibration magnetoelectric therapy instrument intervenes in patients with CP/CPPS through multiple pathways, promoting the absorption of local inflammatory substances in the prostate, relieving patient discomfort, and improving mood and quality of life by stimulating local tissue microcirculation and immune system function in the prostate. Therefore, it showed a statistically significant decrease in the TCMS scores and its statistical difference.
In this study, the treatment effect was evaluated by comparing pre- and post-treatment NIH-CPSI scores. The NIH-CPSI scale is an internationally recognised tool for evaluating CP/CPPS symptoms[12] and consists of nine items that can be subdivided into three scales: pain, urinary symptoms, and quality of life. In this study, the overall effectiveness of the magneto-vibration magnetotherapy device in patients with CP/CPPS reached 58.5%, and the device significantly reduced NIH-CPSI-assessed pain, urinary symptoms, and quality of life scores, with statistically significant differences. Thus, magnetic vibration magnetotherapy is a trusted treatment modality for improving CP/CPPS symptoms in patients.
In addition, previous studies have reported a strong association between CP/CPPS and sexual dysfunction. A meta-analysis of sexual dysfunction in patients with CP/CPPS showed an overall prevalence of approximately 62%; the primary symptoms of erectile dysfunction and premature ejaculation accounted for 29% and 40%, respectively, and this trend is increasing year on year[13]. CP/CPPS and PE are common disorders in men and have a close association. A clinical study[14] found that the prevalence of PE was as high as 26% in Chinese patients with CP/CPPS, and it can be assumed that CP/CPPS is an important cause of PE. A clinical study in Korea showed that PE was significantly and independently associated with CP/CPPS and that the severity of CP/CPPS was strongly associated with PE. Moreover, CP/CPPS-related investigations in patients with PE and increased PE-related investigations in patients with CP/CPPS were recommended[15]. Previous studies have discovered that physiotherapy, such as pelvic floor muscle training and transcutaneous electrical stimulation, for patients with PE inhibits rhythmic contractions of the perineal muscles, increases the strength of the urethral sphincter closure, and has high safety and few side effects[16-18]. The difference in the patients' IIEF-5 scores before and after treatment was statistically significant in the current study. Their mean values decreased, which may have been related to relieving pelvic floor muscle spasm with magnetic vibration magnetotherapy. A previous study has found[19] that physiotherapy to relieve pelvic floor myofascial can improve erectile dysfunction (ED) because relieving pelvic floor spasm promotes arterial blood inflow and improves vascular endothelial dysfunction.
Further, this study investigated and analysed the mental state of patients with CP/CPPS. Previous studies have found that stress caused by adverse emotions, such as anxiety and depression, can exacerbate the symptoms of patients with CP/CPPS[20,21]. Previous meta-analyses of psychological factors and pain catastrophising in our department have shown that psychological factors and pain catastrophising are highly prevalent in patients with CP/CPPS and can affect the severity, symptoms, treatment, and prognosis of CP/CPPS[22]. In addition, poor mental status affects CP/CPPS and leads to sexual dysfunction. Previous studies have suggested that most patients with CP/CPPS experience mild ED, which is likely to be caused by negative emotions associated with CP/CPPS, such as anxiety and depression[23]. Magnetotherapy treatment improved negative emotions by relieving CP/CPPS symptoms; therefore, the GAD, PHQ, and PCS scale scores decreased, and the differences in these scores were statistically significant.
This study had several limitations, such as incomplete data on some patients due to the impact of the new crown epidemic, insufficient sample size, no control group for cross-sectional comparison, and no additional laboratory tests for relevant biological samples.
Although magnetotherapy has not yet been standardised, our study found that it was effective in improving symptoms in patients with CP/CPPS symptoms, accommodating sexual dysfunction in some patients, and relieving negative emotions in others. Therefore, it should be considered as an alternative treatment modality. However, future studies involving additional control and patient groups are required for objective measurements.
| 1. | Xu Y, Zhang L, Shen Y, Yao H, Yong S, You Y. Effectiveness of psychological interventions for treating chronic prostatitis/chronic pelvic pain syndrome: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e22151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Zhang Z, Li Z, Yu Q, Wu C, Lu Z, Zhu F, Zhang H, Liao M, Li T, Chen W, Xian X, Tan A, Mo Z. The prevalence of and risk factors for prostatitis-like symptoms and its relation to erectile dysfunction in Chinese men. Andrology. 2015;3:1119-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Rees J, Abrahams M, Doble A, Cooper A; Prostatitis Expert Reference Group (PERG). Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline. BJU Int. 2015;116:509-525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 188] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 4. | Zhang MJ, Chang DG, Bin B, Guo J, Jin BF, Li YF, Sun ZX, Dai JC, Du L, Zhou SH, Yang WT, Wang JH, Zhang CH; Andrology Committee of Chinese Association of Integrated Traditional and Western Medicine, People's Hospital Affiliated to Fujian University of Chinese Medicine, Affiliated Hospital Affiliated to Chengdu University of Chinese Medicine, First Affiliated Hospital of Guangxi University of Chinese Medicine, China Academy of Chinese Medicine, Xiyuan Hospital, Zhongda Hospital of Southeast University, Army Specialty Medical Center, Army Specialty Medical Center, Renji Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, West China Hospital of Sichuan University, Guangzhou University of Chinese Medicine, the First Affiliated Hospital, Ruikang Hospital of Guangxi University of Chinese Medicine, Hainan Provincial People's Hospital, Yunnan Provincial Hospital of Traditional Chinese Medicine. Guidelines of integrated traditional chinese medicine & western medicine for CP. Zhognguo Nankexue Zazhi. 2023;37:3-17. |
| 5. | Dun RL, Tsai J, Hu XH, Mao JM, Zhu WJ, Qi GC, Peng Y. A systematic review of cross-cultural adaptation of the National Institutes of Health Chronic Prostatitis Symptom Index. Health Qual Life Outcomes. 2021;19:159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 6. | Li J, Dong L, Yan X, Liu X, Li Y, Yu X, Chang D. Is Acupuncture Another Good Choice for Physicians in the Treatment of Chronic Prostatitis/Chronic Pelvic Pain Syndrome? Review of the Latest Literature. Pain Res Manag. 2020;2020:5921038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Masterson TA, Masterson JM, Azzinaro J, Manderson L, Swain S, Ramasamy R. Comprehensive pelvic floor physical therapy program for men with idiopathic chronic pelvic pain syndrome: a prospective study. Transl Androl Urol. 2017;6:910-915. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Kim TH, Han DH, Cho WJ, Lee HS, You HW, Park CM, Ryu DS, Lee KS. The efficacy of extracorporeal magnetic stimulation for treatment of chronic prostatitis/chronic pelvic pain syndrome patients who do not respond to pharmacotherapy. Urology. 2013;82:894-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Li Y, Chu L, Li X, Zhai W, Ma Y, He Y, Xu Y, Ding S, Gao H, Zhang J, Ye B, Wang J, Yao J, Wu C, Xiao L. Efficacy of different-frequency TEAS on acute pain after the total knee arthroplasty: a study protocol for a parallel group randomized trial. Trials. 2019;20:306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Schmid HP, Abt D, Engeler DS. Words of wisdom: Re: Refractory chronic pelvic pain syndrome in men: can transcutaneous electrical nerve stimulation help? Eur Urol. 2014;65:669-670. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Li Z, Liu J, Liu P, Zhang Y, Han W. Effects of Electroacupuncture with Different Waveforms on Chronic Prostatitis/Chronic Pelvic Pain Syndromes: A Randomized Controlled Trial. Contrast Media Mol Imaging. 2022;2022:6866000. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Clemens JQ, Mullins C, Ackerman AL, Bavendam T, van Bokhoven A, Ellingson BM, Harte SE, Kutch JJ, Lai HH, Martucci KT, Moldwin R, Naliboff BD, Pontari MA, Sutcliffe S, Landis JR; MAPP Research Network Study Group. Urologic chronic pelvic pain syndrome: insights from the MAPP Research Network. Nat Rev Urol. 2019;16:187-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 103] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 13. | Loh-Doyle JC, Stephens-Shields AJ, Rolston R, Newcomb C, Taple B, Sutcliffe S, Yang CC, Lai H, Rodriguez LV. Predictors of Male Sexual Dysfunction in Urologic Chronic Pelvic Pain Syndrome (UCPPS), Other Chronic Pain Syndromes, and Healthy Controls in the Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network. J Sex Med. 2022;19:1804-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Liang CZ, Hao ZY, Li HJ, Wang ZP, Xing JP, Hu WL, Zhang TF, Ge WW, Zhang XS, Zhou J, Li Y, Zhou ZX, Tang ZG, Tai S. Prevalence of premature ejaculation and its correlation with chronic prostatitis in Chinese men. Urology. 2010;76:962-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Lee JH, Lee SW. Relationship between premature ejaculation and chronic prostatitis/chronic pelvic pain syndrome. J Sex Med. 2015;12:697-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Uribe OL, Sandoval-Salinas C, Corredor HA, Martínez JM, Saffon JP. Transcutaneous electric nerve stimulation to treat patients with premature ejaculation: phase II clinical trial. Int J Impot Res. 2020;32:434-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Shechter A, Serefoglu EC, Gollan T, Springer S, Meiry G, Appel B, Gruenwald I. Transcutaneous functional electrical stimulation-a novel therapy for premature ejaculation: results of a proof of concept study. Int J Impot Res. 2020;32:440-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Pastore AL, Palleschi G, Fuschi A, Al Salhi Y, Zucchi A, Bozzini G, Illiano E, Costantini E, Carbone A. Pelvic muscle floor rehabilitation as a therapeutic option in lifelong premature ejaculation: long-term outcomes. Asian J Androl. 2018;20:572-575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Lee SW, Liong ML, Yuen KH, Leong WS, Cheah PY, Khan NA, Krieger JN. Adverse impact of sexual dysfunction in chronic prostatitis/chronic pelvic pain syndrome. Urology. 2008;71:79-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Koh JS, Ko HJ, Wang SM, Cho KJ, Kim JC, Lee SJ, Pae CU, Serretti A. The association of personality trait on treatment outcomes in patients with chronic prostatitis/chronic pelvic pain syndrome: an exploratory study. J Psychosom Res. 2014;76:127-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Koh JS, Ko HJ, Wang SM, Cho KJ, Kim JC, Lee SJ, Pae CU. The impact of depression and somatic symptoms on treatment outcomes in patients with chronic prostatitis/chronic pelvic pain syndrome: a preliminary study in a naturalistic treatment setting. Int J Clin Pract. 2014;68:478-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Huang X, Qin Z, Cui H, Chen J, Liu T, Zhu Y, Yuan S. Psychological factors and pain catastrophizing in men with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): a meta-analysis. Transl Androl Urol. 2020;9:485-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Li XC, Zhang XB, Liao ZC, Tang ZY, Li DJ. Is mild erectile dysfunction associated with severe psychological symptoms in Chinese patients with moderate-to-severe chronic prostatitis/chronic pelvic pain syndrome? Asian J Androl. 2021;23:319-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/