Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.3734
Revised: May 13, 2024
Accepted: May 15, 2024
Published online: July 6, 2024
Processing time: 117 Days and 2.6 Hours
with the widespread application of computer network systems in the medical field, the plan-do-check-action (PDCA) and the international classification of diseases tenth edition (ICD-10) coding system have also achieved favorable results in clinical medical record management. However, research on their combined application is relatively lacking. Objective: it was to explore the impact of network systems and PDCA management mode on ICD-10 encoding. Material and Method: a retrospective collection of 768 discharged medical records from the Medical Record Management Department of Meishan People’s Hospital was conducted. They were divided into a control group (n = 232) and an observation group (n = 536) based on whether the PDCA management mode was imple
To study the adoption of network and PDCA in the ICD-10.
A retrospective collection of 768 discharged medical records from the Medical Record Management Department of Meishan People’s Hospital was conducted. They were divided into a control group (n = 232) and an observation group (n = 536) based on whether the PDCA management mode was implemented. The two sets of coding accuracy, time spent, case completion rate, satisfaction, and other indicators were compared.
In the 3, 6, 12, 18, and 24 months of PDCA cycle management mode, the coding accuracy and medical record completion rate were higher, and the coding time was lower in the observation group as against the controls (P < 0.05). The satisfaction of coders (80.22% vs 53.45%) and patients (84.89% vs 51.72%) in the observation group was markedly higher as against the controls (P < 0.05).
The combination of computer networks and PDCA can improve the accuracy, efficiency, completion rate, and satisfaction of ICD-10 coding.
Core Tip: Through research, it has been found that the combined application of computer networking and plan-do-check-action cycle management mode in the international classification of diseases tenth edition coding of medical records significantly improves coding accuracy, shortens coding time, increases the completeness of medical records, and achieves high satisfaction from coders and patients.
- Citation: Lian B. Adoption of network and plan-do-check-action in the international classification of disease 10 coding. World J Clin Cases 2024; 12(19): 3734-3743
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/3734.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.3734
In recent years, propelled by the swift advancement of medical information technology, computer networked systems have garnered widespread adoption within the medical domain[1]. The proliferation of medical information technology has not only enhanced the efficiency of hospital management but has also engendered challenges in medical record coding. Within the contemporary medical framework, precise coding of medical records constitutes the bedrock of hospital administration and decision-making processes, exerting direct influence on the caliber of medical services, the efficacy of medical records management, and the fiscal outcomes of medical establishments[2]. The international classification of diseases tenth edition (ICD-10) coding system[3,4], serving as a standardized medical coding schema, has found extensive utility across global medical institutions for delineating diverse diseases and medical procedures, and facilitating medical record organization, statistical scrutiny, and reimbursement procedures. Consequently, the precision of ICD-10 coding assumes paramount importance in patient care, medical institution quality assurance, and medical resource stewardship[5].
Nonetheless, the precision of ICD-10 coding in medical records remains a significant concern within the healthcare sector[6]. Particularly within the traditional manual coding milieu, the propensity for human error poses a notable risk, potentially resulting in the distortion of medical statistics, erroneous calculation of medical expenses, challenges in medical record administration, and even adverse ramifications on patient treatment and clinical decisions[7,8]. Against this backdrop, numerous medical institutions have embarked on endeavors to enhance the coding process, aiming to bolster the accuracy and efficiency of ICD-10 coding. Among these initiatives, the adoption of computer network systems[9] and implementation of the plan-do-check-action (PDCA) cycle management paradigm[10] are recognized as promising solutions with considerable potential.
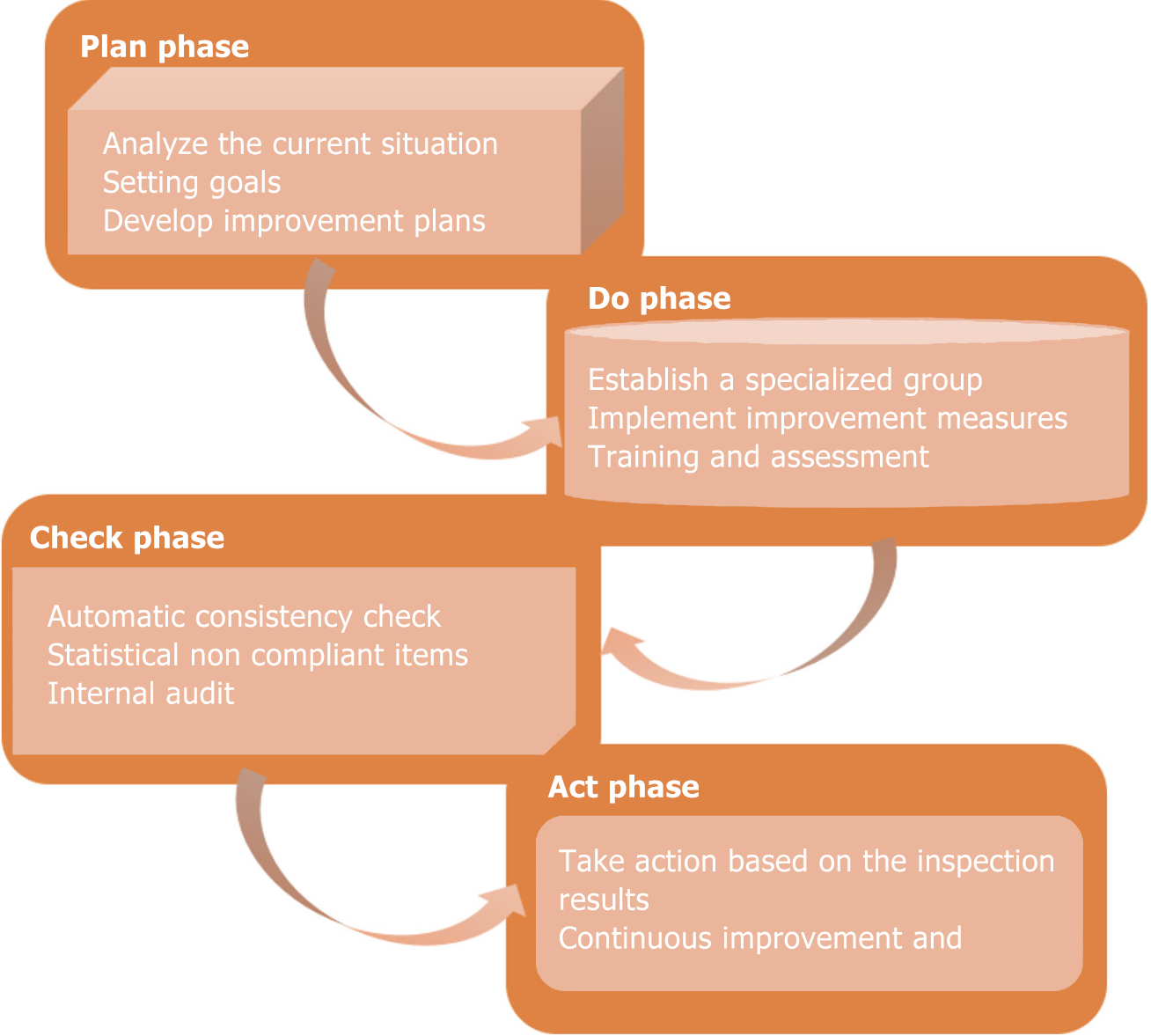
The term “computer network” denotes the amalgamation of computer and communication technologies to facilitate interconnectivity among devices for the sharing of information, resources, and services[11]. This technology finds ubiquitous application across diverse sectors including business[12], medicine[13], education[14], government[15], and social domains[16]. Notably, within the medical sphere, the utilization of computer network technology has witnessed significant strides, fundamentally transforming the landscape of medical information management. This technology enables rapid dissemination and sharing of information, enhances the efficiency of medical data storage and transmission, mitigates coding errors, and furnishes medical practitioners with enhanced workflow convenience and access to information resources[17,18]. The PDCA cycle management mode epitomizes a method of continuous improvement and governance, encompassing four primary phases: Plan, Do, Check, and Act[19]. This iterative cycle enables institutions to systematically identify areas for enhancement, thereby augmenting the quality and efficiency of their operations through ongoing refinement and iteration. In recent years, the PDCA cycle management mode has garnered widespread adoption across diverse domains such as quality management[20], healthcare[21], and education[22]. The application domains of computer network systems and PDCA cycle management mode exhibit significant overlap, with heightened attention directed towards their integration within the medical arena. While several studies have underscored the capacity of computer networks to enhance the utilization and statistical efficiency of medical record information[23], the PDCA cycle management mode has demonstrated tangible efficacy in augmenting the accuracy and quality of ICD-10 coding within medical records[24]. Nevertheless, empirical research concerning the combined application of these methodologies in the realm of medical record coding remains relatively scant.
Hence, this work endeavors to furnish crucial insights for medical institutions regarding strategies to enhance coding accuracy and elevate the quality of medical record management by investigating the influence of computer networks and the PDCA cycle management model on ICD-10 coding. Such an endeavor holds substantial promise for optimizing medical services, enhancing patient care quality, and judiciously managing medical resources. It is anticipated that this study will offer valuable lessons and guidance for future endeavors in medical information management and quality control endeavors.
A total of 768 discharged medical records from the medical records management room of Meishan People’s Hospital from January 2020 to January 2023 were randomly selected as the research objects. All medical records in this work were managed using a computer network system instead of paper medical records. According to whether the PDCA cycle management method was implemented, 232 medical records from January to December 2020 were not implemented with the PDCA cycle management method, so the traditional medical record coding method was used to set them as the controls; A total of 536 medical records from January 2021 to December 2022 were treated with PDCA cycle coding method, and were set as the observation group. According to the medical records, there were 182 male and 50 female patients in the controls, aged from 18 to 70 years old (45.21 ± 4.01), and the course of disease was 7-40 d (23.82 ± 2.35). There were 384 male and 152 female patients in the observation group. The average age was 42.35 ± 3.98 years old, ranging from 18-70, and the course of disease was 25.33 ± 2.61 d, ranging from 6-42 d. By comparison, there was no visible difference in general clinical data between two groups (P > 0.05). The study had obtained informed consent from patients and signed an informed consent form, and had been approved by the Medical Ethics Committee of Meishan People’s Hospital (Approval Number: MPP-23-602).
All patients’ medical records were managed utilizing a computer networked system, comprising an electronic medical record management system (EMR) and an online ICD-10 coding tool. The EMR serves as a comprehensive information management platform tailored for recording, storing, and overseeing patients’ medical records. Leveraging the EMR, medical institutions can achieve the digitization of medical records, thereby expediting access, sharing, and updating processes. The online ICD-10 coding tool represents an application expressly designed to aid coders in enhancing the accuracy and efficiency of their coding endeavors. To ensure sample homogeneity, the management system for all patient medical records in this study was an electronic medical record system procured from Beijing Tongchuang Tiancheng Technology Co., LTD. The online ICD-10 coding tool utilized is the IMO Problem Terminology provided by Intelligent Medical Objects company.
Controls: the control group underwent treatment using the traditional medical record coding method. This process involved several steps: (1) Documentation: Physicians and nurses documented patients’ clinical information, encompassing medical history, physical examination findings, laboratory results, medical imaging findings, surgical reports, and other pertinent medical documents, which were stored as electronic medical records; (2) Data extraction: Medical record coders extracted essential information such as diagnostic outcomes, symptoms, and procedural details from patient documents and records, converting them into a representation system compliant with ICD-10 coding standards; (3) Coding process: Based on symptoms and disease names from diagnostic outcomes, the corresponding ICD-10 codes were retrieved via the electronic medical record system and subsequently inputted into the relevant section of the medical record homepage; and (4) Quality control: Upon completion of medical record coding, internal audits and quality control measures were implemented to ensure coding accuracy and consistency. These included routine coder audits to assess the quality of their work.
Observation group: The observation group underwent treatment utilizing the PDCA cycle management model for medical record coding. The specific management approach of the PDCA cycle model is depicted in Figure 1.
Step 1: Planning stage: Initially, the current scenario was scrutinized. A total of 232 medical records spanning January to December 2019 were amassed to assess the precision of ICD-10 coding. Findings revealed 102 inaccurately coded cases, yielding an error rate of 43.96%, well below the state-mandated threshold of 95%. Through deliberation and analysis, it became apparent that key factors impeding coding accuracy included non-standard medical record documentation, an inadequate medical records management system, deficient implementation of audit and quality control measures, limited coder knowledge base, lack of timely updates, and deficient coding awareness among coders. Subsequently, goal-setting and planning ensued: Accounting for coder proficiency and the progressive nature of knowledge acquisition, a predetermined target accuracy rate exceeding 90% was established. Informed by the analysis of influencing factors, improvement strategies were devised: (1) Enhancing medical record documentation standards; (2) Refining the medical records management system: Enacting medical records management policies and instituting a review committee; (3) Intensifying audit and quality control measures, encompassing bolstered internal and external reviews and the establishment of quality control benchmarks; (4) Enhancing coder knowledge and skills through ongoing education, resource sharing, and incentivizing certification attainment: coders were encouraged to pursue medical coding certification to enhance their professional proficiency; and (5) Fostering coding awareness through training initiatives and instituting incentive mechanisms.
Step 2: Implementation stage: Initially, a dedicated team for enhancing ICD-10 coding management was constituted. The core team comprised a professional coding expert, a physician specializing in the relevant department, a medical quality and compliance specialist, and a medical record management expert. Subsequently, the planned improvement measures were executed as follows: (1) Enhancing medical record documentation standards: Physicians and nurses underwent training to adhere to standardized medical record writing practices, with a review process established for timely corrections; (2) Refining the medical records management system: Departmental responsibilities were delineated, accompanied by the establishment of a medical record quality review committee tasked with overseeing system implementation; (3) Intensifying audit and quality control measures: Routine internal audits were conducted, supplemented by the introduction of external review entities, and the clarification of quality control standards and guidelines; (4) Enhancing coder knowledge and skills: Continuous education and training initiatives were provided for coders, alongside the establishment of a resource-sharing platform enabling access to the latest coding guidelines and materials. Coders were incentivized to pursue medical coding certification to augment their professionalism; and (5) Fostering coding awareness: Training sessions emphasizing the ethics and significance of coding were conducted, while positive coding accuracy performance was incentivized through rewards or recognition schemes. The efficacy of the aforementioned coding-related training was assessed to gauge training effectiveness.
Step 3: Inspection stage: Regular assessments (monthly) were conducted to automatically verify the consistency of ICD-10 codes with corresponding disease and surgical descriptions via computerized checks. Non-conforming items were identified, tallied, and subsequently verified and rectified by the respective coders. Actual error rates and accuracy metrics were calculated accordingly. Comparative analysis of pre- and post-improvement data was performed to assess the efficacy of the improvement measures. Internal audits were conducted to scrutinize coder work and processes, ensuring adherence to established standards.
Step 4: Action phase: Based on the findings of the inspection phase, further action was undertaken. If the data indicated potential for enhanced coding accuracy, workflow refinements, additional training provisions, or system rectifications were implemented. Moreover, a culture of continuous improvement was fostered, entailing ongoing monitoring of coding accuracy, refinement of workflows, and adaptability to evolving circumstances, thereby facilitating sustained enhancements in coding accuracy over time.
The accuracy rate of disease and surgery coding, coding time (comprising medical records review and verification), and the rate of quality improvement were documented at 1, 3, 6, 12, 18, and 24 months post-implementation of the PDCA cycle management method within the observation group. A comparative analysis of disease and surgery coding accuracy, efficiency, and quality improvement rates between the observation group and controls was conducted.
Through questionnaire surveys or interviews, feedback was collected from coders in both the control and observation groups regarding the two medical record management models (Table 1). Additionally, patient satisfaction with medical record photocopying was assessed by directly querying patients regarding their level of satisfaction, with response options ranging from very dissatisfied to very satisfied. This evaluation aimed to gauge both coder and patient satisfaction levels. Subsequently, the acceptance and practical feasibility of the new model were analyzed.
| Items | Specific questions |
| Productivity | How productive are you when using the medical record management model? |
| Are you satisfied with the improved work efficiency of the medical record management model? | |
| Accuracy | Are you satisfied with the coding accuracy of the medical record management model? |
| Are you satisfied with the accuracy of coding improved by the medical record management model? | |
| Workload | Are you satisfied with the relief of your workload by the medical record management model? |
| Summary | Overall, are you satisfied with the results of your medical record coding? |
SPSS 19.0 statistical software was used for data collation and analysis. The count data were expressed as [n (%)], and chi-square test was performed. P < 0.05 was used to indicate significant differences.
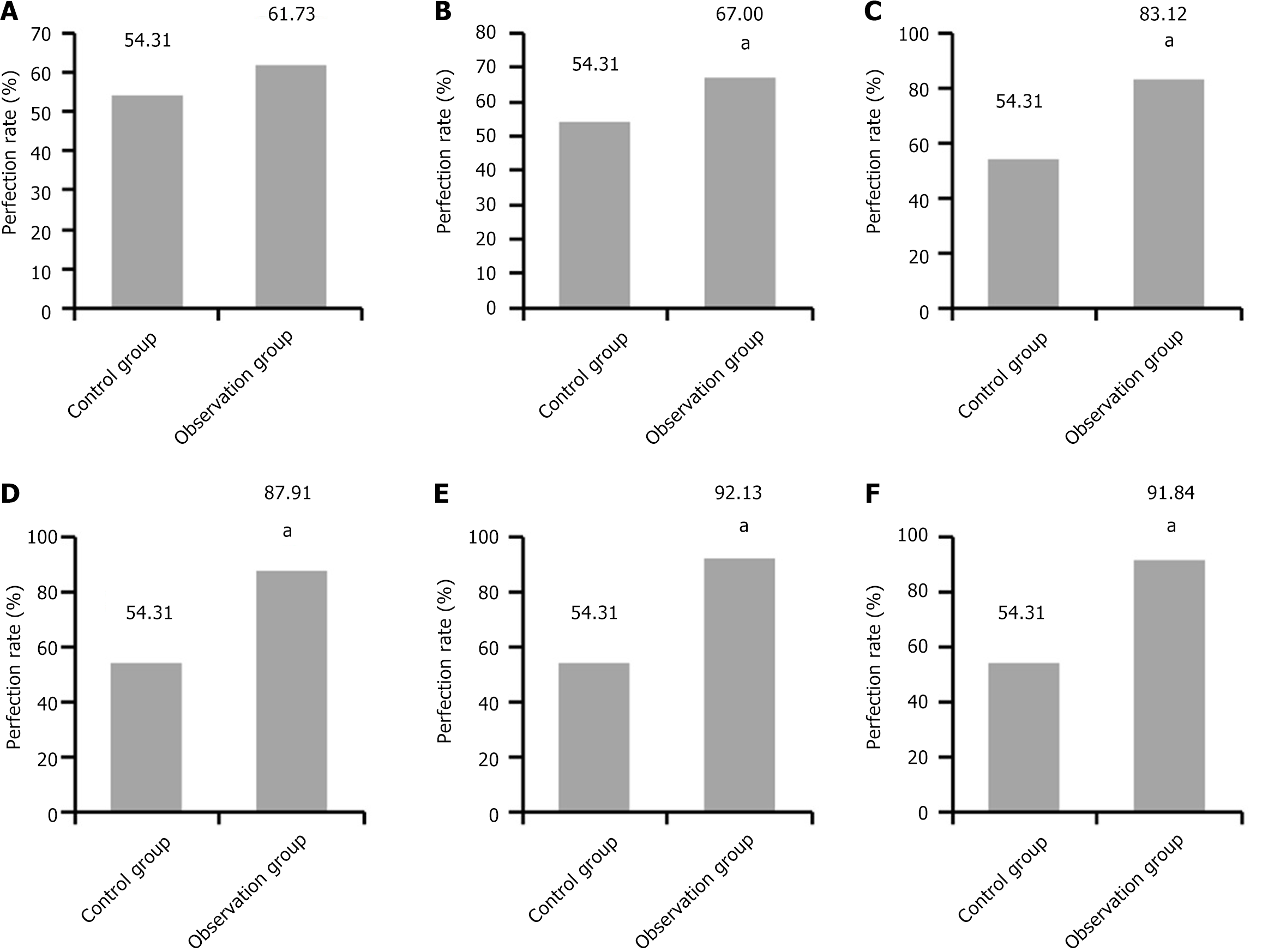
It was noted that among the 232 medical records in the control group, 130 were accurately coded, yielding an accuracy rate of 56.03%. The observation group exhibited the following trends: One month post-implementation of the PDCA cycle management method, 81 medical records were assessed, with 51 coded accurately, resulting in an accuracy rate of 62.96%; at 3 months, 100 medical records were evaluated, with 69 accurately coded, achieving a rate of 69%; by 6 months, 77 samples were reviewed, of which 65 were accurately coded, reflecting an accuracy rate of 84.42%. After 12 months, 91 samples were examined, with 82 accurately coded, yielding a rate of 90.11%. At the 18-month mark, 89 samples were analyzed, and 83 were accurately coded, reaching an accuracy rate of 93.26%. Lastly, after 24 months, 98 samples were collected, and 92 were accurately coded, resulting in an accuracy rate of 93.88%. The observation group demonstrated a progressive increase in coding accuracy over time, surpassing that of the control group. Significant disparities in accuracy were observed between the two groups at all time points, except for the initial one-month period post-implementation (P < 0.05; Figure 2).
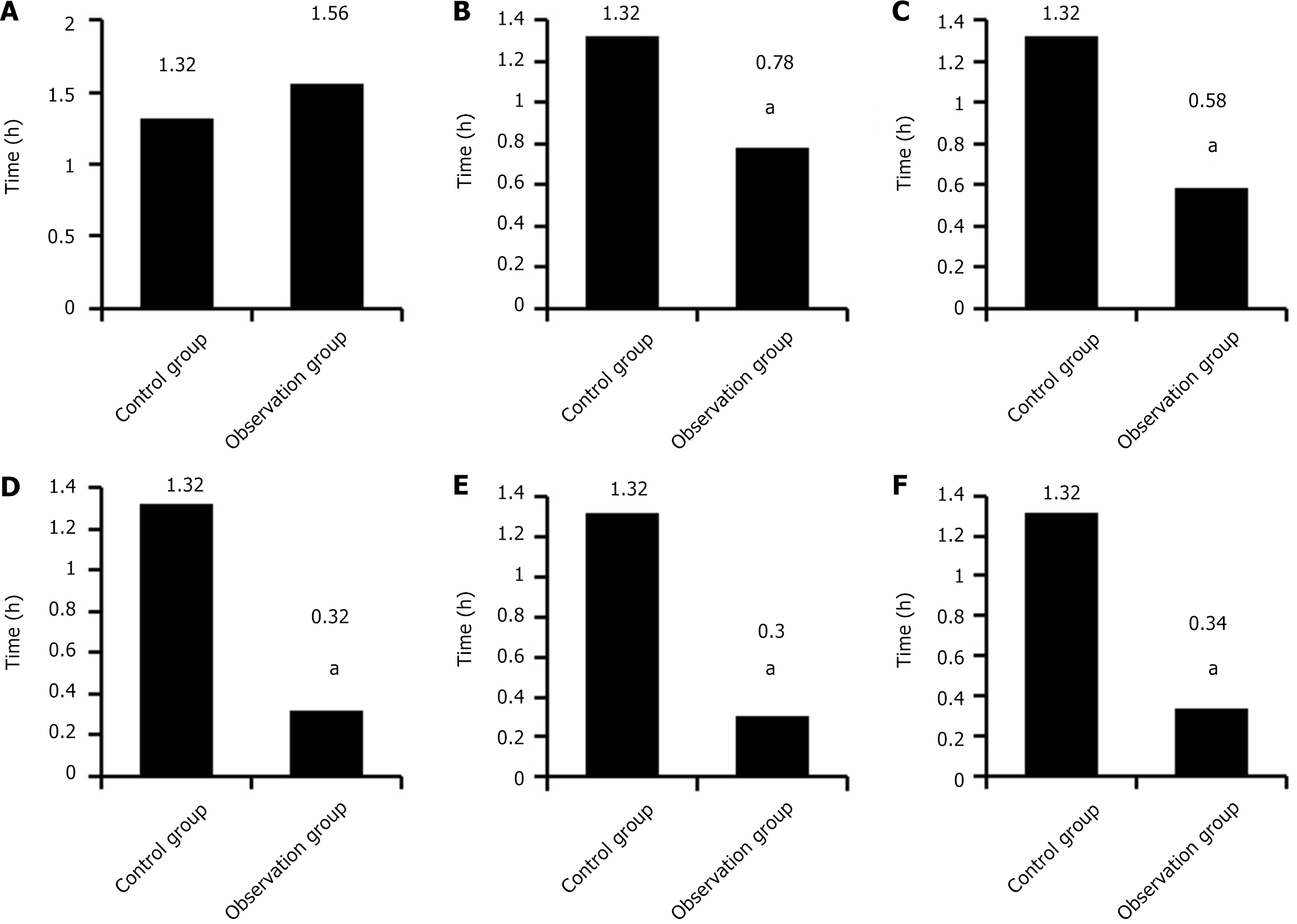
The average coding time of 232 medical records in the controls was 1.32 ± 0.72 h. One month after the implementation of PDCA cycle management method, the coding time of medical records in the observation group was 1.56 ± 0.66 h; 3 months later, 0.78 ± 0.35 h; 6 months later, 0.58 ± 0.12 h; 12 months later, 0.32 ± 0.14 h; after 18 months, 0.30 ± 0.10 h; after 24 months, 0.34 ± 0.11 h. Through observation, the coding time of the observation group was higher as against the controls in the first month, without obvious differences (P > 0.05), and the coding time of the 3, 6, 12, 18, and 24 months was markedly lower in the observation group (P < 0.05; Figure 3).
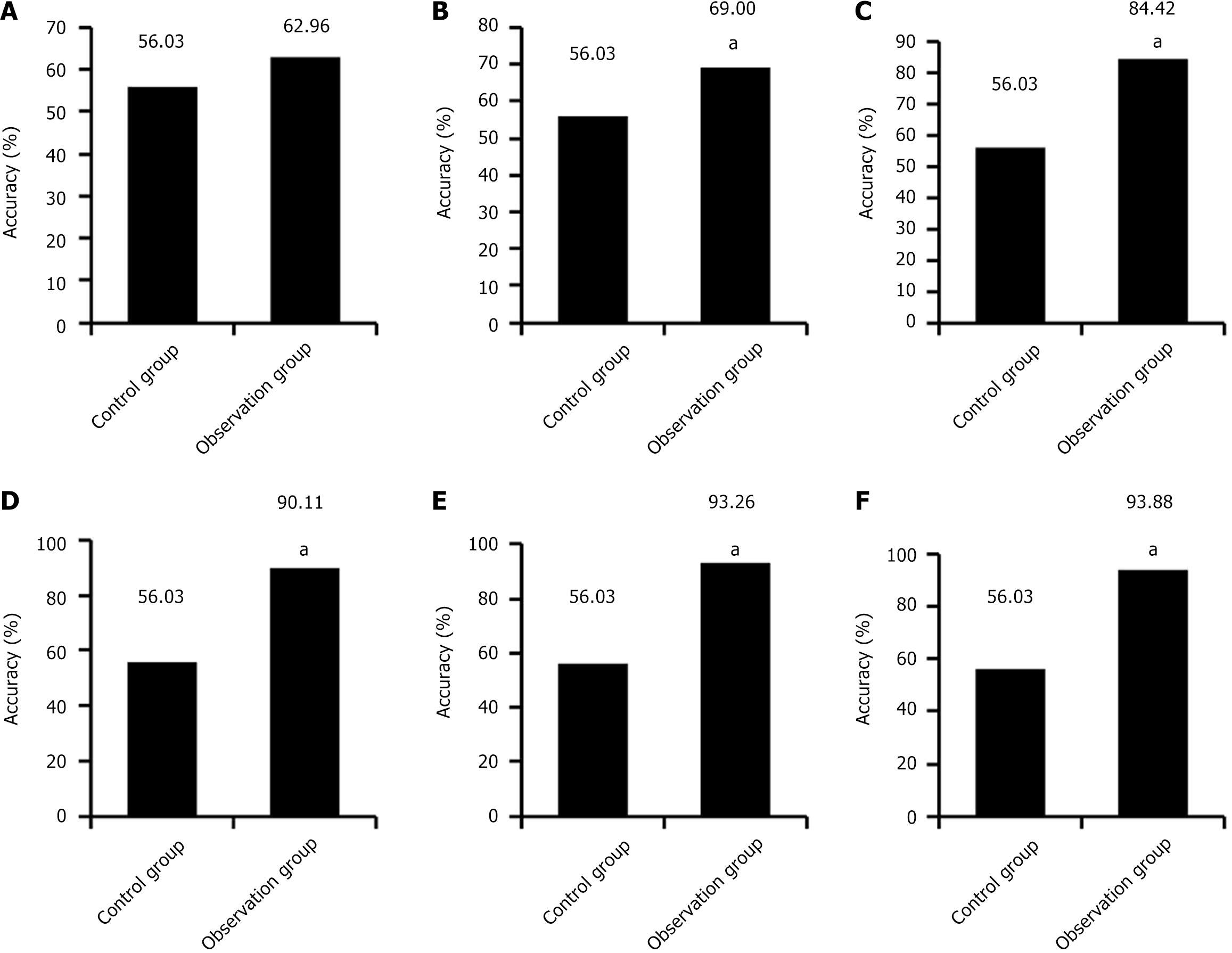
In the controls, 126 out of 232 medical records were perfect, and the perfect rate of medical records was 70.69%. The specific situation of the observation group was as follows: one month after the implementation of PDCA cycle management method, 81 medical records were collected, of which 50 were perfect, and the perfect rate of medical records was 61.73%; 3 months later, 100 medical records were collected, 67 of them were perfect, and the perfect rate of medical records was 67%. Six months later, 77 medical records were collected, and 64 of them had complete medical records, with a complete rate of 83.12%. Following 12 months, 91 cases were collected, and 80 cases had complete medical records, with a complete rate of 87.91%. Eighteen months later, 89 cases were collected, and 82 cases had complete medical records, with a complete rate of 92.13%. Following 24 months, 98 cases were collected, 90 cases had complete medical records, and the complete rate of medical records was 91.84%. Through observation, the medical record completion rate of the observation group was on a gradual upward trend, which was higher as against the controls, and except for 1 month of implementation, the medical record completion rate at other time points was markedly different from that of the controls (P < 0.05; Figure 4).
Table 2 shows the statistics of coder and patient satisfaction survey results. As far as coders were concerned, 124 out of 232 control cases were satisfied with the coding, and the satisfaction rate was 53.45%. 430 of 536 cases in the observation group were satisfied with the coding, with a satisfaction rate of 80.22%. In terms of patients, 120 out of 232 copies of the controls were satisfied, with a satisfaction rate of 51.72%. Among the 536 copies of medical records in the observation group, 455 copies were satisfied by patients, with a satisfaction rate of 84.89%. After comparison, the satisfaction of coders and patients in the observation group was markedly higher as against the controls (P < 0.05).
ICD coding serves as an international standard and sophisticated discipline utilized for classifying and coding diverse health conditions and medical diagnoses, constituting one of the paramount indicators within the medical domain[25]. Precision in coding is indispensable for ensuring the fidelity of patients’ medical records and data, particularly in instances of medical disputes[26]. Consequently, medical institutions must undertake a series of measures to uphold the accuracy and consistency of coding, thereby enhancing the quality of medical records.
Clinical studies have revealed that the accuracy of medical record coding is influenced by several factors, including the training of medical personnel, the quality of clinical documentation, adherence to medical policies and guidelines, review and quality control practices, and the utilization of computer-aided coding systems[27,28]. Presently, the integration of computer networks into medical record management has yielded notable outcomes, positively impacting the efficiency, quality, and accessibility of healthcare systems. Nevertheless, various extraneous factors continue to impact the accuracy of medical record coding. To further enhance coding accuracy, the PDCA cycle management model is introduced to iteratively refine and optimize the medical record management process. Results from this study indicated that the observation group exhibited more pronounced advantages over the controls across multiple dimensions.
The observation group consistently exhibited significantly higher coding accuracy and lower coding times compared to the controls at 3, 6, 12, 18, and 24 months (P < 0.05). These findings underscore the substantial efficacy of the PDCA cycle management model in enhancing both the accuracy and efficiency of coding processes, thereby mitigating the risks of misdiagnosis and missed diagnoses, and ultimately augmenting the quality and efficacy of the healthcare system. The PDCA cycle management mode embodies a continuous improvement process, capable of iterative refinement with each cycle yielding greater enhancements. It emphasizes data-driven decision-making, fosters a culture of continual improvement, and advocates for a transparent approach to problem-solving[29]. Consequently, the model facilitates organizational adaptability, quality enhancement, waste reduction, and efficiency augmentation[30]. These outcomes hold significant implications for healthcare coding practices and quality management endeavors. This work found that the case completion rate of 3/6/12/18/24 months after the implementation of PDCA management model in the observation group gradually increased, and were higher relative to the controls (P < 0.05). This implies that medical records managed under the PDCA management mode exhibit greater completeness and adherence to standards, thereby expectedly enhancing the quality of medical records and reducing omissions and errors. This bears significant implications for medical record management and patient care. Concurrently, studies have corroborated the pronounced advantages of the PDCA method in enhancing the quality of pathology management and nursing outcomes. As the accuracy, efficiency, and integrity of medical record coding improve, the satisfaction levels of both coders and patients also rise. This underscores that the utilization of the PDCA management method not only enhances internal workflow efficiency and accuracy but also augments interaction and satisfaction with patients. Such enhancements are pivotal for improving healthcare services and enhancing the overall patient experience.
In conclusion, this study underscores the potential benefits of integrating computer networks with the PDCA cycle management model in the realm of ICD-10 coding of medical records. These advantages encompass enhanced accuracy, time savings, increased medical record completion rates, and improved satisfaction levels. The findings suggest that the amalgamation of computer networks with the PDCA management model holds considerable promise for healthcare institutions seeking to optimize their coding processes and deliver higher quality healthcare services. Future research endeavors could delve deeper into the implementation specifics and long-term impacts of the PDCA method to gain a comprehensive understanding of its potential value.
| 1. | Kumar A, Sinha N, Bhardwaj A, Goel S. Clinical risk assessment of chronic kidney disease patients using genetic programming. Comput Methods Biomech Biomed Engin. 2022;25:887-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Chang C, Liao SC, Shao SC. Positive Predictive Values of Anaphylaxis Diagnosis in Claims Data: A Multi-Institutional Study in Taiwan. J Med Syst. 2023;47:97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 3. | Michalopoulos G, Mikula AL, Kerezoudis P, Biedermann AJ, Parney IF, Van Gompel JJ, Bydon M. Unplanned returns to the operating room: a quality improvement methodology for the comparison of institutional outcomes to national benchmarks. J Neurosurg. 2024;1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Mukherjee A, Shammas N, Xu L, Cannavale KL, Gilfillan AD, Szamreta EA, Monberg M, Hodeib M, Chao CR. Impact of the Coronavirus Disease 2019 pandemic on neoadjuvant chemotherapy use in patients diagnosed with epithelial type ovarian cancer. Front Oncol. 2024;14:1290719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Paleczny S, Osagie N, Sethi J. Validity and reliability International Classification of Diseases-10 codes for all forms of injury: A systematic review. PLoS One. 2024;19:e0298411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 6. | Kumar A, Hammond N, Grattan S, Finfer S, Delaney A. Accuracy of International Classification of Disease Coding Methods to Estimate Sepsis Epidemiology: A Scoping Review. J Intensive Care Med. 2024;39:3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 7. | Zarei J, Golpira R, Hashemi N, Azadmanjir Z, Meidani Z, Vahedi A, Bakhshandeh H, Fakharian E, Sheikhtaheri A. Comparison of the accuracy of inpatient morbidity coding with ICD-11 and ICD-10. Health Inf Manag. 2023;18333583231185355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 8. | Johnson JA, Williams DJ, Feinstein JA, Grijalva CG, Zhu Y, Dickinson E, Stassun JC, Sekmen M, Tanguturi YC, Gay JC, Antoon JW. Positive Predictive Value of ICD-10 Codes to Identify Acute Suicidal and Self Harm Behaviors. Hosp Pediatr. 2023;13:e207-e210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Yang X, Li YM, Wang Q, Li R, Zhang P. Machine learning model based on RCA-PDCA nursing methods and differentiating factors to predict hypotension during cesarean section surgery. Comput Biol Med. 2024;174:108395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Nogueira CS, Silva-Fernandes IJL, de Albuquerque CGP, Oliveira FFB, Wong DVT, Silva PGB, Bitencourt FDS, Lima MVA. How to structure an oncogenetics service for the public health system: Report of the implementation of the first service in Northeastern Brazil. Cancer Genet. 2021;250-251:6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Ma X, Wang Z. Computer security technology in E-commerce platform business model construction. Heliyon. 2024;10:e28571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Shyamala Bharathi P, Shalini C. Advanced hybrid attention-based deep learning network with heuristic algorithm for adaptive CT and PET image fusion in lung cancer detection. Med Eng Phys. 2024;126:104138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Liu H, Tang T. MAPK signaling pathway-based glioma subtypes, machine-learning risk model, and key hub proteins identification. Sci Rep. 2023;13:19055. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 62] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 14. | Jolly AK, Selvarajah D, Micallef J, Torres A, Button D. Adapting the Gamified Educational Networking Online Learning Management System to Test a Decentralized Simulation-Based Education Model to Instruct Paramedics-in-Training on the Emergency Intraosseous Access and Infusion Skill. Cureus. 2024;16:e55493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 15. | Keremoğlu E, Weidmann NB, Gamero-Garrido A, Carisimo E, Dainotti A, Snoeren AC. Network topology facilitates internet traffic control in autocracies. PNAS Nexus. 2024;3:pgae069. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Zhang L, Ge L. A clustering-based differential privacy protection algorithm for weighted social networks. Math Biosci Eng. 2024;21:3755-3773. [PubMed] [DOI] [Full Text] |
| 17. | May JT, Myers J, Noonan D, McConnell E, Cary MP. A call to action to improve the completeness of older adult sexual and gender minority data in electronic health records. J Am Med Inform Assoc. 2023;30:1725-1729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Belfrage S, Helgesson G, Lynøe N. Trust and digital privacy in healthcare: a cross-sectional descriptive study of trust and attitudes towards uses of electronic health data among the general public in Sweden. BMC Med Ethics. 2022;23:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 19. | Lu MN, Zhang BL, Dai QH, Fu XH. Application of the Plan-Do-Check-Act Cycle in Shortening the Decision to Delivery Interval Time. Risk Manag Healthc Policy. 2022;15:1315-1323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 20. | Kong X, Zhu X, Zhang Y, Wu J. The application of plan, do, check, act (PDCA) quality management in reducing nosocomial infections in endoscopy rooms: It does work. Int J Clin Pract. 2021;75:e14351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Gao Y, Chen X, Kang L. The effect of Plan-Do-Check-Act cycle nursing management of gynecological surgery: a systematic review and meta-analysis. Ann Palliat Med. 2021;10:8072-8081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Goenka A, Mundkur S, Sujir Nayak S, Shetty A, Thomas J, Mymbilly Balakrishnan J, Chandra Sekaran V, Dsouza B. Improving the emergency services using quality improvement project and Donabedian model in a quaternary teaching hospital in South India. BMJ Open Qual. 2024;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 23. | Jeong E, Su Y, Li L, Chen Y. Discovering clinical drug-drug interactions with known pharmacokinetics mechanisms using spontaneous reporting systems and electronic health records. J Biomed Inform. 2024;153:104639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Zhong X, Wu X, Xie X, Zhou Q, Xu R, Wang J, He L, He Y, Qiu X. A descriptive study on clinical department managers' cognition of the Plan-Do-Check-Act cycle and factors influencing their cognition. BMC Med Educ. 2023;23:294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 25. | Passanisi S, D’Angelo G, Marseglia L, De Cola C, Granese R, Conti G, Betta P, Cutrupi MC, Fede C, Chimenz R, Salpietro C, Gitto E. Renal anomalies in newborns with vacterel association: case series and literature review. J Biol Regul Homeost Agents. 2019;33:53-58. [PubMed] |
| 26. | Adame-Miranda SJ, Granados-Guzmán G, Silva-Mares DA, Acevedo-Fernández JJ, Waksman-Minsky N, Salazar-Aranda R. Evaluation of antihyperglycemic activity of plants in northeast mexico. Cell Mol Biol (Noisy-le-grand). 2021;67:212-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Yu Y, Qiu T, Duan J, Wang J. Multigranularity Label Prediction Model for Automatic International Classification of Diseases Coding in Clinical Text. J Comput Biol. 2023;30:900-911. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Guo Y, Al-Garadi MA, Book WM, Ivey LC, Rodriguez FH 3rd, Raskind-Hood CL, Robichaux C, Sarker A. Supervised Text Classification System Detects Fontan Patients in Electronic Records With Higher Accuracy Than ICD Codes. J Am Heart Assoc. 2023;12:e030046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 29. | Lv L, Sun Y, Yang B, Xin C, Zhang M. Impact of Pharmacist-Led PDCA Cycle in Reducing Prescription Abandonment: An Action Research from China. Patient Prefer Adherence. 2023;17:2145-2152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 30. | Hsu TW, Huang CH, Chuang LJ, Lee HC, Wong CS. Continuous quality improvement: reducing informed consent form signing errors. BMC Med Ethics. 2023;24:59. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/