Published online May 26, 2024. doi: 10.12998/wjcc.v12.i15.2597
Revised: March 20, 2024
Accepted: April 10, 2024
Published online: May 26, 2024
Processing time: 139 Days and 19.2 Hours
Pituitary gland metastasis is an unusual event, and pituitary metastasis from lung adenocarcinoma is extremely rare and associated with poor prognosis. To date, approximately 15 cases have been reported.
Here, we present the case of a 64-year-old woman with pituitary metastasis derived from lung adenocarcinoma, which was difficult to distinguish from other sellar tumors. The patient presented to the neurosurgery clinic with blurred vision and intermittent headache. During hospitalization, brain computed tomography (CT) and magnetic resonance imaging revealed a pituitary macroadenoma. Chest CT revealed irregular nodules in the basal segment of the lower lobe of the left lung, which were likely lung cancer. Positron emission tomography-CT revealed a carbohydrate metabolism tumor in the lungs and sellar region, which was considered malignant. Postoperative pathological examination of the sellar tumor revealed lung adenocarcinoma.
Excision of pituitary metastases combined with radiotherapy and chemotherapy should be a priority treatment for patients with pituitary metastasis.
Core Tip: Pituitary metastasis from lung adenocarcinoma is extremely rare, but physicians should consider it if it rapidly develops clinical symptoms or grows quickly, especially in patients with other tumors or those with a history of other systemic malignancies. Radiotherapy and chemotherapy are recommended as initial treatments. The blood supply to pituitary metastases is extremely rich; therefore, neurosurgeons must make adequate surgical preparations and plans.
- Citation: Wang Q, Liu XW, Chen KY. Pituitary metastasis from lung adenocarcinoma: A case report. World J Clin Cases 2024; 12(15): 2597-2605
- URL: https://www.wjgnet.com/2307-8960/full/v12/i15/2597.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i15.2597
Pituitary metastasis is a rare condition with poor prognosis. The occurrence rate is approximately 1% for all sellar region tumors, with a median survival of less than 1 year[1]. Patients have non-specific clinical symptoms, such as visual field deficits, cranial nerve palsy, anterior pituitary dysfunction, ophthalmoplegia, and diabetes insipidus. Computed tomo
A 64-year-old Asian woman was hospitalized for blurred vision and intermittent headache of 3 months.
Symptoms started 3 months before presentation with blurred vision and intermittent headache.
The patient had no history of hospitalization.
The patient had no significant personal or family history.
The patient’s vital signs were unremarkable. Ophthalmological examination showed that the naked vision was 0.25 in the right eye and 0.8 in the left eye.
Routine blood and urine analyses showed normal results. The endocrine examination results are presented in Table 1.
| Hormone | Level measured | Normal level |
| ACTH (pg/mL) | 17.20 | 7.2-63.3 |
| PRL (high) (ng/mL) | > 200 | 2.18-26.53 |
| GH (ng/mL) | 0.32 | 0.02-4.77 |
| TSH (μIU/mL) | 1.987 | 0.35-4.94 |
| T3 (nmol/L) | 1.69 | 0.89-2.44 |
| TT4 (low) (nmol/L) | 61.22 | 62.70-150.80 |
| FT3 (pmol/L) | 4.26 | 2.43-6.01 |
| FT4 (pmol/L) | 9.96 | 9.00-19.00 |
| Tg (ng/mL) | 9.988 | 0.20-70.00 |
| LH (low) (pmol/L) | 0.03 | 5.16-61.99 |
| FSH (low) (mIU/mL) | 1.08 | 26.72-133.41 |
| E2 (pg/mL) | < 10 | < 10-28 |
| P4 (ng/mL) | < 0.1 | < 0.1-0.2 |
| CORT (8:00) (μg/dL) | 1.0 | 6.02-18.4 |
| CORT (16:00) (μg/dL) | 1.5 | 2.68-10.5 |
| CORT (24:00) (μg/dL) | 1.1 | 2.68-10.5 |
| TES (pmol/L) | < 12.98 | 10.83-56.94 |
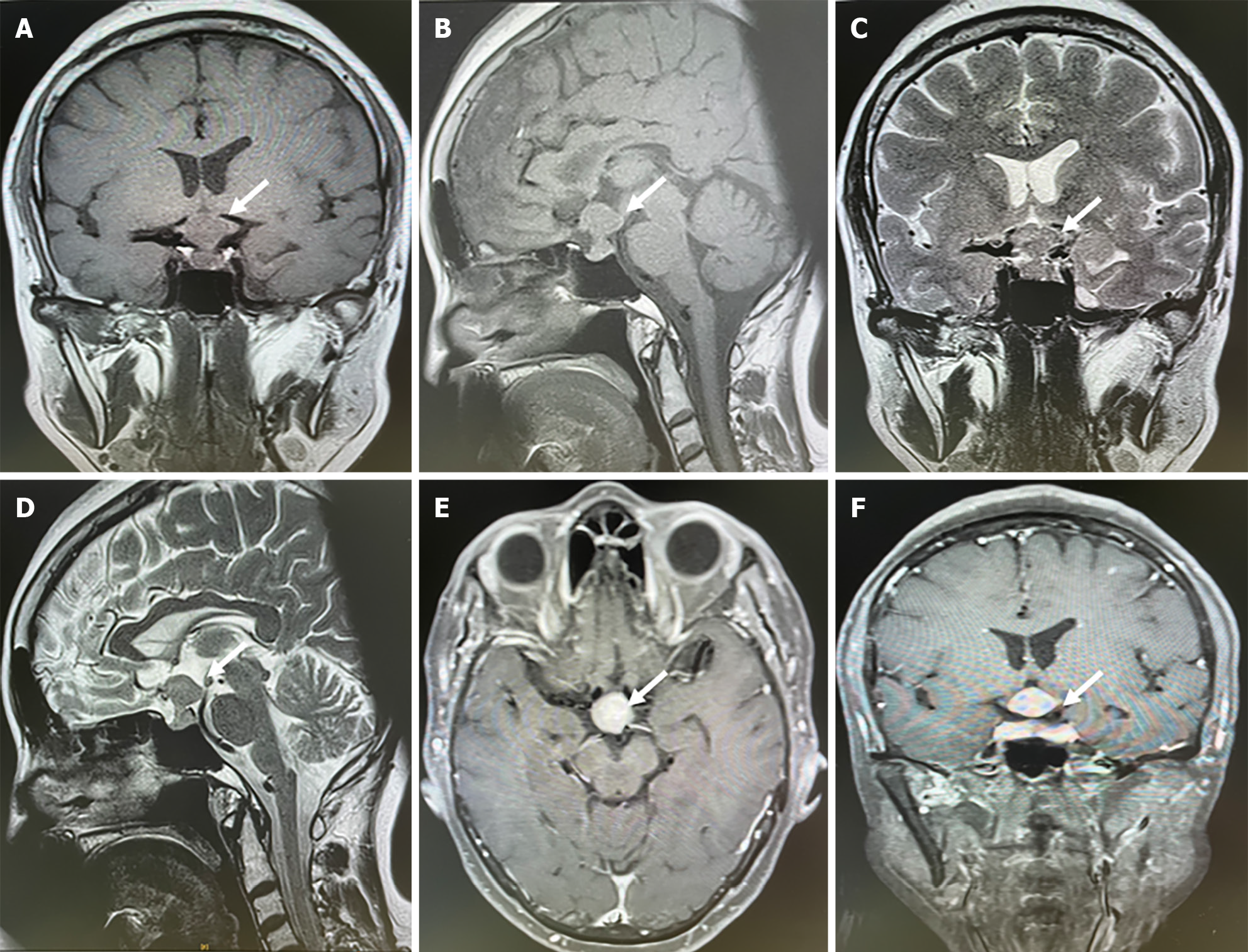
Brain CT showed that the sellar region tumor was related to the carotid artery and was considered a pituitary macroadenoma. Chest CT showed irregular nodules in the basal segment of the lower lobe of the left lung, measuring 2.0 cm × 1.7 cm, which were likely lung cancer. Brain MRI indicated sellar region tumors with isointense signals on T1- and T2-weighted images and an hourglass sign (Figure 1). The tumor was homogeneously enhanced on contrast MRI. The lesion was approximately 1.6 cm × 0.8 cm × 1.3 cm, which was considered pituitary macroadenoma. Positron emission tomography-CT revealed a carbohydrate metabolism tumor in the lungs and sellar region, which was considered malignant. Fiber bronchoscopy revealed a neoplasm in the left lung and hematoxylin and eosin (H&E) staining suggested lung adenocarcinoma.
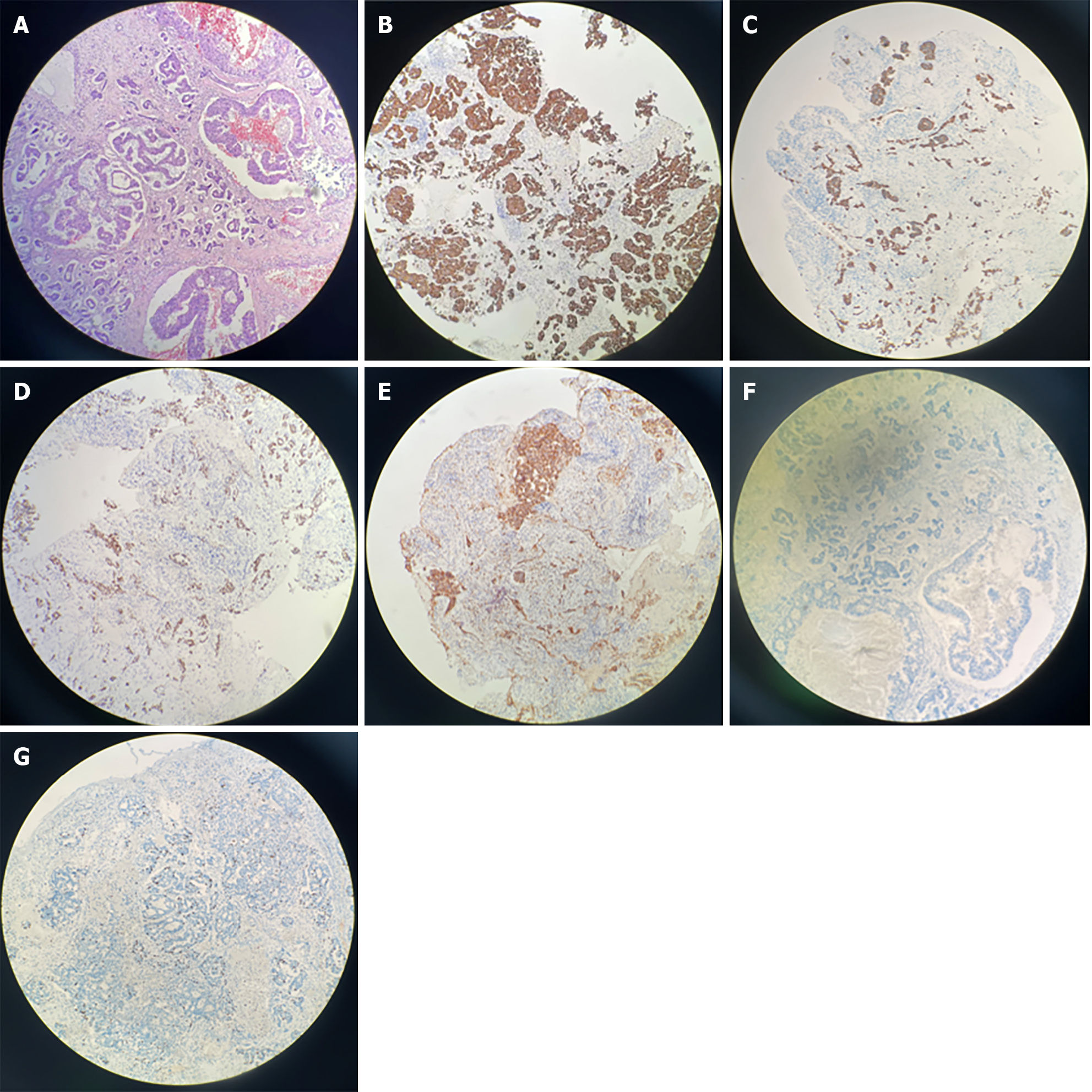
H&E staining of the sellar mass revealed a metastatic adenocarcinoma (Figure 2A). Immunohistochemistry showed positive results for CK7 (Figure 2B), CK18 (Figure 2C), TTF-1 (Figure 2D), Napsin A (+) (Figure 2E), and GATA3 (+) (Figure 2F) and negative results for CK20, CDX-2, GFAP, PAX-8, ER, and HER2. The Ki-67 index was 10%, indicating metastatic lung adenocarcinoma (Figure 2G). Next-generation sequencing confirmed somatic mutations in TSC2, POLD1, ARID1A, CTNNB1, ERBB2, and expressed PD-L1 (tumor proportion score = 1%) (Table 2).
| Gene | Expressed region | Nucleotide | Amino acid | Mutation abundance (%) |
| TSC2 | Exon 36 | c.4585C>T | p.R1529W | 5.1 |
| POLD1 | Exon19 | c.2312C>T | p.A771V | 3.8 |
| ARID1A | Exon 1 | c.1058C>T | p.A353V | 5.1 |
| ARID1A | Exon 1 | c.308C>T | p.S103L | 7.7 |
| CTNNB1 | Exon 4 | c.79G>A | p.G27R | 13.5 |
| ERBB2 | Exon 23 | c.2339C>T | p.A800V | 5.1 |
Based on the patient’s clinical symptoms and physical, imaging, and pathological examinations, the final diagnosis was pituitary metastasis.
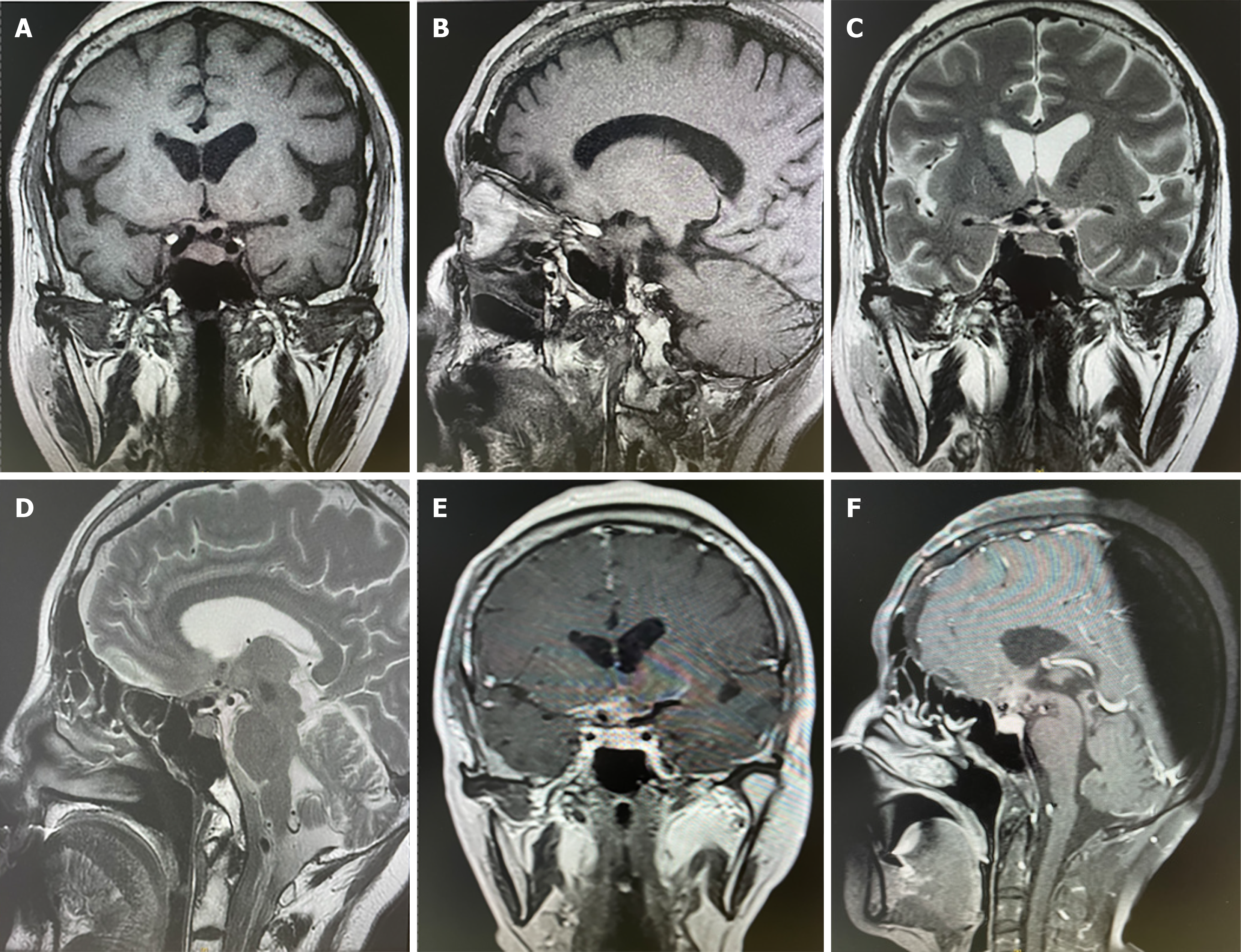
The patient was taken to the operating room for resection of the right coronary flap tumor of the sellar mass. During the operation, the tumor was gray, tough, aggressive, and rich in blood supply, infiltrating the sellar turcica, third ventricle of the cerebrum, and frontal lobe. The intraoperative bleeding volume was approximately 500 mL. Postoperatively, the patient recovered well and the vision was improved. The patient was advised to undergo immune and chemical therapies at a cancer hospital. Postoperative MRI revealed no tumor regrowth within 3 months (Figure 3).
The patient is still alive, with no recurrence noted 1 year after surgery.
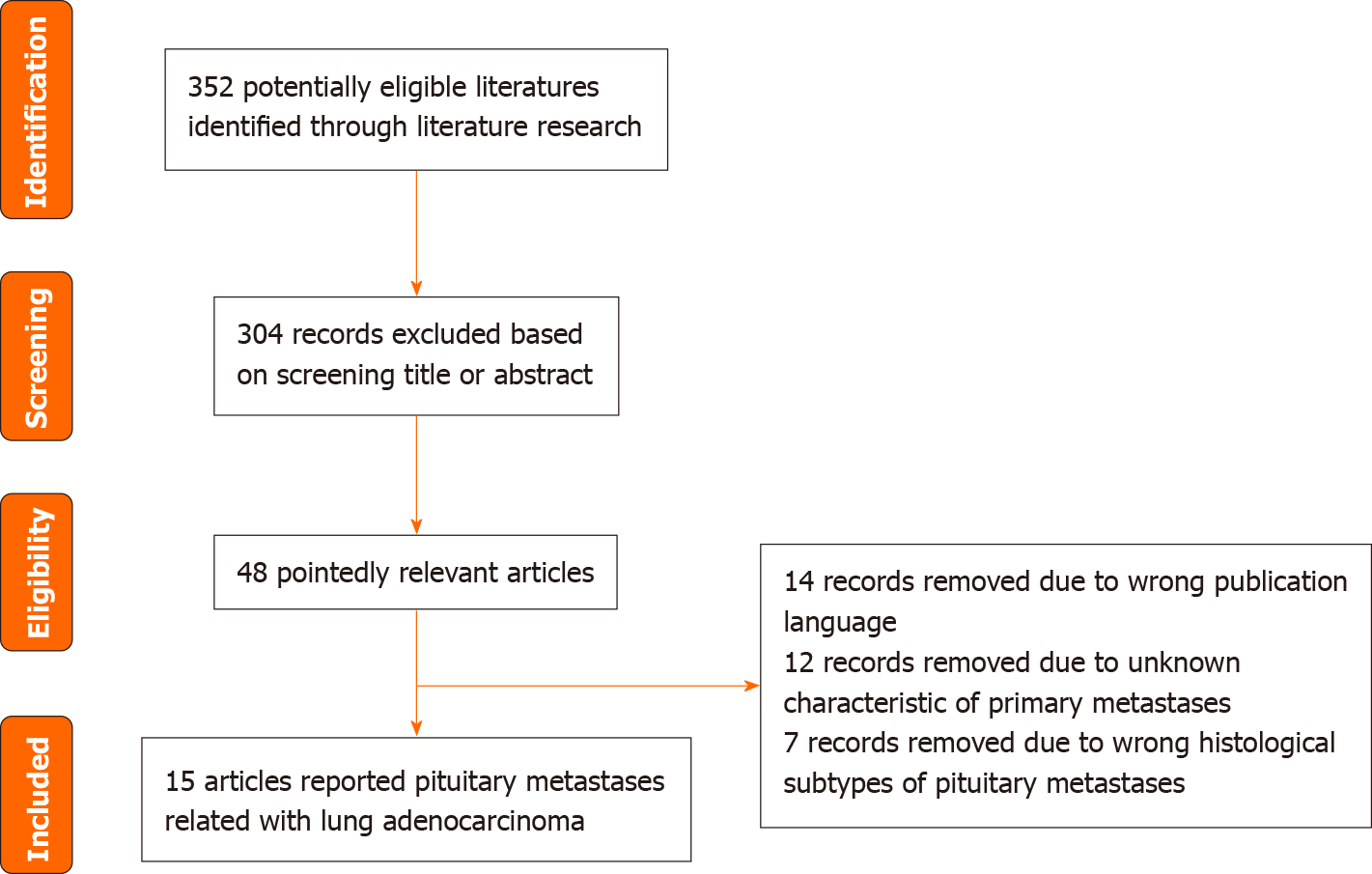
The literature was searched in PubMed till March 14, 2024. The medical subject heading search terms and strategies included pituitary metastasis and lung cancer. In total, 352 studies were screened using the PubMed database. The language was restricted to English and only published articles were included. We reviewed 15 articles that reported pituitary metastasis from lung adenocarcinoma. A flowchart of the literature selection process is shown in Figure 4. The characteristics of the included studies are presented in Table 3.
| Ref. | Year | Age (yr) | Sex | Symptom | Hormone | Treatment | Tumor Supply | Survival |
| Asim and Elashaal[13] | 2023 | 54 | F | None | ACTH (low), COTR (low), LH (low), FSH (low), TES (low), TSH (low), FT3 (low), FT4 (low) | RT, ST | ND | Alive, 3 months |
| Amaral et al[14] | 2022 | 43 | M | Headache, VFD | ACTH (low), CORT (low), FSH (low), FT4 (low), TES (low), LH (low) | ST, CT, RT, IT | R | Alive, 15 months |
| Wong et al[15] | 2022 | 53 | F | VFD | ND | ST, RT, CT | ND | Alive, 24 months |
| Han et al[16] | 2022 | 48 | F | Headache, DI | ACTH (low), Cort (low), PRL (high) | ST, CT | ND | Alive, 20 months |
| Lopes et al[17] | 2021 | 62 | F | Fatigue, Headache, Nocturia, Polydipsia, BV | FT4 (low), CORT (low), ACTH (low), FSH (low), PRL (high) | ST, CT | R | Alive, 24 months |
| Tanaka et al[9] | 2021 | 80 | F | Polyuria, Polydipsia | ADH (low) | RT, CT | ND | Alive, 7 months |
| Liu et al[3] | 2021 | 53 | M | BV, DI, VFD, Polyuria, Vomit, Fatigue | CORT (low), TSH (high), T4 (low), FSH (low), LH (low), PRL (high) | ST | R | Dead, 4 months |
| Watanabe et al[18] | 2020 | 70 | M | Anorexia | ADH (low), ACTH (low), CORT (low), FSH (low), LH (low), TSH (low) | RT, CT | ND | Dead, 5 months |
| Rajakumar et al[19] | 2020 | 49 | F | Headache, VFD | LH (low), FSH (low), CORT (low), TES (low), FT4 (low) | ST, RT, CT | NR | ND |
| Alhashem et al[11] | 2020 | 54 | M | Headache, Droop bilateral eyelid | ND | ST | NR | ND |
| Sheahan et al[5] | 2020 | 52 | F | MB | ACTH (low), CORT (low), FSH (low), TSH (low), PRL (high) | ST, CT | ND | ND |
| Yao et al[20] | 2019 | 67 | M | Headache, Vomit, ptosis | PRL (high), FSH (low), LH (low), ACTH (low), Cort (low) | ST, RT | ND | Dead, 3 months |
| Sirinvaravong et al[21] | 2019 | 72 | F | DI | PRL (high), FSH (low), LH (low), TSH (high) | ST | ND | Dead, 4 months |
| Gulati et al[12] | 2015 | 47 | F | Headache, DI | TSH (low), FSH (low) | ST | ND | ND |
| Arai et al[22] | 2010 | 61 | F | VFD | Normal | ST, RT | NR | Alive, 3 months |
Sellar tumors mostly originate from pituitary adenomas and rarely metastasize to other organs. Autopsies have revealed that pituitary metastases account for nearly 5% of all pituitary metastases in sellar tumors. In surgical sections, less than 1% of all sellar tumors are associated with pituitary metastasis[3]. Pituitary metastases always metastasize from the lungs and breasts, accounting for 39.7% and 23.7% of cases, respectively[4]. Small cell carcinomas are usually trans
The clinical symptoms and radiographic findings of pituitary metastases are nonspecific. Patients present with visual field deficits, diabetes insipidus, cranial nerve palsy, or anterior pituitary dysfunction. Pituitary metastasis is a rare disease with poor prognosis. It is difficult to diagnose, especially in patients who are not diagnosed with a primary cancer. Physicians should consider these diseases, especially in older patients presenting with new-onset deficiencies in visual and anterior pituitary hormones. Pituitary adenoma often manifests hypointense on T1-weighted images and hyperintense on T2-weighted images, similar to pituitary metastasis. This is the main reason for misdiagnosis. However, pituitary metastasis often manifests as pituitary stalk thickening, invasion of the cavernous sinus, and coexistence of brain lesions, which have been observed in pituitary adenomas. Furthermore, if patients have other tumors detected on imaging or a history of other systemic malignancies, neurosurgeons should consider pituitary metastasis.
Pituitary metastases mostly located in posterior pituitary alone or combined with anterior pituitary accounting for 84.6%. Only 15.4% of cases have been found in the anterior pituitary alone[7]. It is mainly because the location and blood supply. The posterior pituitary has larger area to contact with the dura mater compared to anterior. The posterior pituitary receives blood supply from hypophyseal artery. on the contrary, the anterior pituitary only receives venous supply through hypophyseal portal system. The patient was admitted to the hospital due to blurred vision and headache accompanied by increased prolactin hormone and decreased cortisol, suggesting that the tumor had damaged both anterior and posterior pituitary glands. During operation, the tumor was tough, aggressive, and rich of blood which was different from the common sellar region tumors, such as pituitary adenoma, craniopharyngiomas and so on. According to the operation features and fiber bronchoscope, we suspected the tumor was likely pituitary metastases from lung. After operation, H&E and immunohistochemistry all confirmed pituitary metastasis from lung adenocarcinoma.
There are currently no standard protocols for the treatment of pituitary metastasis. The treatment for pituitary metastasis includes surgery, chemotherapy, and radiotherapy (RT). The choice of treatment depends on the primary tumor, clinical symptoms, and physical conditions. Surgical eradication includes transsphenoidal surgery and cra
Pituitary metastasis from lung adenocarcinoma is extremely rare, but physicians should consider it if rapidly developing clinical symptoms or growing quickly, especially for the patients found other tumors on images or had a history of other system malignancy. RT and chemotherapy are recommended as the initial treatments. The blood supply to pituitary metastases is extremely rich, so it is necessary for neurosurgeons to make adequate operation preparations and surgery plans.
| 1. | Liu X, Wang R, Li M, Chen G. Pituitary Metastasis of Lung Neuroendocrine Carcinoma Mimicking Pituitary Adenoma:Case Report and Literature Review. Front Endocrinol (Lausanne). 2021;12:678947. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Nooreldeen R, Bach H. Current and Future Development in Lung Cancer Diagnosis. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 343] [Cited by in RCA: 518] [Article Influence: 103.6] [Reference Citation Analysis (0)] |
| 3. | Liu CY, Wang YB, Zhu HQ, You JL, Liu Z, Zhang XF. Hyperprolactinemia due to pituitary metastasis: A case report. World J Clin Cases. 2021;9:190-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 4. | Komninos J, Vlassopoulou V, Protopapa D, Korfias S, Kontogeorgos G, Sakas DE, Thalassinos NC. Tumors metastatic to the pituitary gland: case report and literature review. J Clin Endocrinol Metab. 2004;89:574-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 273] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 5. | Sheahan KH, Huffman GC, DeWitt JC, Gilbert MP. Metastatic Lung Cancer Presenting as Monocular Blindness and Panhypopituitarism Secondary to a Pituitary Metastasis. Am J Case Rep. 2020;21:e920948. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Riihimäki M, Hemminki A, Fallah M, Thomsen H, Sundquist K, Sundquist J, Hemminki K. Metastatic sites and survival in lung cancer. Lung Cancer. 2014;86:78-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 623] [Cited by in RCA: 644] [Article Influence: 53.7] [Reference Citation Analysis (0)] |
| 7. | Ng S, Fomekong F, Delabar V, Jacquesson T, Enachescu C, Raverot G, Manet R, Jouanneau E. Current status and treatment modalities in metastases to the pituitary: a systematic review. J Neurooncol. 2020;146:219-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Gilard V, Alexandru C, Proust F, Derrey S, Hannequin P, Langlois O. Pituitary metastasis: is there still a place for neurosurgical treatment? J Neurooncol. 2016;126:219-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Tanaka S, Hirabayashi T, Kimoto M, Hama M, Hachiya T, Gomi K. Gefitinib Treatment Was Unsuccessful for Central Diabetes Insipidus Due to Pituitary Metastasis of Lung Adenocarcinoma. Intern Med. 2021;60:1073-1076. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Castle-Kirszbaum M, Goldschlager T, Ho B, Wang YY, King J. Twelve cases of pituitary metastasis: a case series and review of the literature. Pituitary. 2018;21:463-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Alhashem A, Taha M, Almomen A. Pituitary metastasis of lung adenocarcinoma: Case report and literature review. Int J Surg Case Rep. 2020;67:98-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Gulati S, Kiefer C, Karim NA. Diabetes Insipidus: An Unusual Presentation of Adenocarcinoma of the Lung in a Patient with no Identifiable Lung Mass. N Am J Med Sci. 2015;7:476-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Asim SA, Elashaal AA. Metastasis of lung adenocarcinoma to the pituitary gland. Radiol Case Rep. 2023;18:3487-3491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Amaral S, Matias A, Bouça B, Manique I, Palha A, Cortez L, Cerqueira L, Forte D, Sagarribay A, Dutra E, Cristóvão M, Pontinha C, Mafra M, Silva-Nunes J. Pituitary metastasis as the first manifestation of lung carcinoma. Clin Case Rep. 2022;10:e6601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Wong PS, Rajoo S, Achmad Sankala H, Long Bidin MB. Unusual presentation of lung carcinoma with pituitary metastasis: a challenging diagnosis and sodium management dilemmas. Endocr Oncol. 2022;2:K15-K20. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Han D, Zhao K, Yang Q, Zhang L, Fei S. Secondary mutant ALK-I1171s in pituitary metastases from a patient with ALK fusion-positive advanced lung adenocarcinoma: A case report and literature review. Front Oncol. 2022;12:1016320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 17. | Lopes AM, Pereira J, Ribeiro I, Martins da Silva A, Queiroga H, Amaral C. Pituitary metastasis unveiling a lung adenocarcinoma. Endocrinol Diabetes Metab Case Rep. 2021;2021:20-0211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Watanabe M, Yasuda J, Ashida K, Matsuo Y, Nagayama A, Goto Y, Iwata S, Watanabe M, Sasaki J, Hoshino T, Nomura M. Masked Diabetes Insipidus Hidden by Severe Hyponatremia: A Case of Pituitary Metastasis of Lung Adenocarcinoma. Am J Case Rep. 2020;21:e928113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Rajakumar R, Rahmatullah IH, Rahim AA. Case Report of a Pituitary Metastasis from Lung Adenocarcinoma Masquerading as Pituitary Adenoma. J ASEAN Fed Endocr Soc. 2020;35:133-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Yao H, Rui W, Zhang Y, Liu Y, Lin S, Tang H, Zhao W, Wu Z. Prolactin-Secreting Lung Adenocarcinoma Metastatic to the Pituitary Mimicking a Prolactinoma: A Case Report. Neurosurgery. 2019;85:E773-E778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Sirinvaravong S, Vibhatavata P, Chunharojrith P, Cheunsuchon P, Sriussadaporn S. Diabetes insipidus and panhypopituitarism as a first presentation of silent adenocarcinoma of lung: a case report and literature review. BMC Endocr Disord. 2019;19:114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Arai A, Morishita A, Hanada Y, Aihara H. Solitary metastatic tumor within the optic chiasm--case report. Neurol Med Chir (Tokyo). 2010;50:158-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade C
P-Reviewer: Chien CR, Taiwan S-Editor: Zheng XM L-Editor: A P-Editor: Yu HG