Published online May 26, 2024. doi: 10.12998/wjcc.v12.i15.2482
Revised: April 8, 2024
Accepted: April 19, 2024
Published online: May 26, 2024
Processing time: 80 Days and 0.4 Hours
Lymphedema is a prevalent complication affecting patients with breast cancer, greatly impacting their quality of life. This editorial describes diagnostic methods and therapeutic interventions for managing lymphedema in patients with breast cancer. Diagnosis relies on clinical evaluation and objective measures, including arm circumference and volumetric assessments, along with lymphoscintigraphy and ultrasonic measurements. Treatment primarily involves complex decon
Core Tip: This editorial describes the diagnosis and management of lymphedema in patients with breast cancer. Lymphedema, a common complication of breast cancer treatment, greatly impacts patients' quality of life and psychological well-being. Diagnosis relies on clinical evaluation and objective measures, including arm circumference and volumetric assessments, as well as lymphoscintigraphy and ultrasonic measurements. Treatment involves complex decongestive physical therapy comprising manual lymphatic drainage, compression therapy, exercise, and skin care. Early diagnosis and proper treatment are essential for effective management of lymphedema in patients with breast cancer.
- Citation: Choi JE, Chang MC. Management of lymphedema is really a matter in patients with breast cancer. World J Clin Cases 2024; 12(15): 2482-2486
- URL: https://www.wjgnet.com/2307-8960/full/v12/i15/2482.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i15.2482
Lymphedema is an abnormal accumulation of protein-rich fluid in interstitial spaces due to a compromised lymphatic system[1]. In patients with breast cancer, lymphedema commonly occurs in the arm on the operated side because of regional lymph node involvement of the tumor, surgical removal of the lymph nodes for tumor treatment, and radiation therapy[2]. The incidence of this condition following breast cancer treatment has been reported at 5%-60%; such differences in incidence may be attributed to differences in diagnostic criteria, measurement methods, and follow-up periods[3]. The condition is considered as incurable and is a major factor decreasing the quality of life of patients with breast cancer[4]. In addition to cosmetic problems, physical discomfort, and functional impairment, lymphedema causes various psychological problems, such as depression, anxiety, and social avoidance[4]. Moreover, patients often experience inflammation from lymphangitis or cellulitis[5,6]. Stagnant proteins in tissues affected by lymphedema serve as a good medium for bacterial growth, increasing the likelihood of an infection[6]. Therefore, prevention, early diagnosis, and proper treatment of lymphedema are crucial.
In this editorial, we comment on a paper by Mubarak et al[7] published in a recent issue of World Journal of Clinical Cases. The authors described that the presence of tumor deposits in patients with breast cancer indicates a poor prognosis and recommended that clinicians should carefully investigate the presence of tumor deposits. We describe the diagnosis and management of lymphedema, another important issue in patients with breast cancer.
Although there is no gold standard test for diagnosing lymphedema, common complaints from patients include feeling heavy, tightness, and/or pain. The objective method most commonly used in clinical practice is measurement of both the left and right arm circumferences at the same position, where a difference of > 2 cm between arms is used to diagnose moderate lymphedema[2,8]. A difference of ≤ 2 cm is considered to indicate mild lymphedema[2]. Volumetric methods can also be used, including the water replacement method, which defines lymphedema as a difference of ≥ 200 mL in volume between the two arms[9]. These assessments should be performed preoperatively and within 1 mo postoperatively; once lymphedema has been identified, weekly assessment should be considered[10]. Upon the completion of treatment, follow-up should be performed every 2-3 mo for 1-2 years[10]. Although medical history assessment and clinical examinations may be sufficient for diagnosis, lymphoscintigraphy can be performed to examine the functional status of the lymphatic system and predict treatment outcomes and prognosis[11]. Moreover, ultrasonic measurement of the thickness of the skin and subcutaneous fat layers as well as changes in echogenicity may also help in diagnosis and severity determination[12].
Complex decongestive physical therapy, which is primarily used to treat lymphedema, consists of four components: Manual lymphatic drainage, compression therapy, exercise therapy, and skin care[13,14]. This therapy typically involves 2-6 wk of intensive therapy followed by several months of management[13,14]. The effects of properly administered complex decongestive physical therapy and appropriate management of lymphedema can last from several months to as long as 2 years or more[13,14]. In addition, prophylactic administration of this therapy after breast cancer surgery has been reported to reduce the incidence of lymphedema[15].
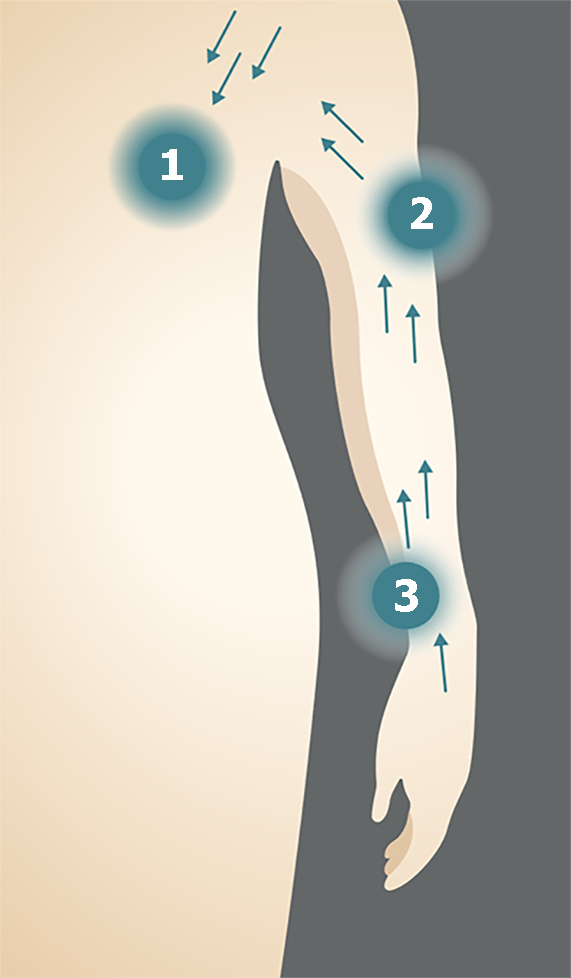
Herein, we discuss individual therapies comprising complex decongestive physical therapy. Manual lymphatic drainage is a highly specialized massage technique designed to increase the movement of lymphatic fluid (Figure 1)[16]. Slow and rhythmical massage is used to drain congested lymphatic fluid from the non-functioning lymphotome to areas that remain functional; the lymphatic fluid is then removed through the remaining lymph nodes. This massage technique is performed in a proximal-to-distal direction[17] with very superficial and light pressure of approximately 30-45 mmHg[18].
Compression therapy involves application of external force, which increases the tissue pressure and facilitates lymphatic and venous circulation to promote lymphatic duct functions[19]. Moreover, it can facilitate the distribution of protein components in fibrotic arm tissues. As compression therapy, a compression bandage (Figure 2A) or compression stocking (Figure 2B) can be applied and should be worn during exercise and activities of daily living[20]. When applying the compression bandage method, a short-stretch, non-elastic bandage is used to increase the working pressure[21]. The patient is also instructed to wear a compression stocking to reduce swelling and maintain an appropriate arm shape and protect the skin, while applying compensatory pressure on the skin that has been stretched and lacks elasticity after the swelling has been reduced[22]. In addition, wearing a compression stocking can enhance the flow of lymphatic fluid, which reduces protein buildup and improves venous circulation[22].
Exercises include upper extremity range of motion exercises, stretching, and resistive exercises for muscle streng
Finally, thorough skin care should be administered to patients with lymphedema[26]. Measures should be taken to prevent and maintain proper hygiene to minimize bacterial infection and lymphedema.
Patients should avoid saunas and tub baths, as they can increase the risk of lymphedema, and should avoid exposure to extreme cold or heat[27]. As dieting can help reduce lymphedema volume, a reduced dietary calorie intake and low-fat diet are recommended to some patients[28].
As drug therapy, flavonoids can be used[29] to enhance lymphangiomotion and reduce capillary permeability. If there are findings of secondary infection, appropriate antibiotics should be administered immediately[30]. Diuretics are not effective in the long term, as they can exacerbate edema by increasing protein accumulation in the interstitial space.
Surgical treatment is another option for patients with lymphedema that is not controlled by conservative treatment. Microsurgical lymphovenous anastomoses, debulking, and liposuction can be performed to remove excess fluid or tissue and relieve symptoms[31]. However, surgical procedures can lead to complications such as delayed wound healing, infection, and recurrence, and, therefore, should be carefully selected.
Lymphedema commonly occurs in patients with breast cancer, which can affect not only the quality of life but also physical function and has a negative psychological impact. Therefore, lymphedema should be actively controlled through early diagnosis and proper treatment. Despite the high need for treatment, effective treatments for lymphedema are lacking for patients with breast cancer. Clinicians should acquire sufficient knowledge on the diagnostic and treatment methods and actively provide appropriate medical services to these patients.
| 1. | Manrique OJ, Bustos SS, Ciudad P, Adabi K, Chen WF, Forte AJ, Cheville AL, Jakub JW, McLaughlin SA, Chen HC. Overview of Lymphedema for Physicians and Other Clinicians: A Review of Fundamental Concepts. Mayo Clin Proc. 2022;97:1920-1935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 2. | Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zamba GKD, Scott-Conner C. Lymphedema following breast cancer: The importance of surgical methods and obesity. Front Womens Health. 2018;3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Rebegea L, Firescu D, Dumitru M, Anghel R. The incidence and risk factors for occurrence of arm lymphedema after treatment of breast cancer. Chirurgia (Bucur). 2015;110:33-37. [PubMed] |
| 4. | Taghian NR, Miller CL, Jammallo LS, O'Toole J, Skolny MN. Lymphedema following breast cancer treatment and impact on quality of life: a review. Crit Rev Oncol Hematol. 2014;92:227-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 231] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 5. | Hosseinzadeh A, Ebrahimi K, Shahriarirad R, Dalfardi F. Lower limb lymphedema and cellulitis as a complication of COVID-19 vaccine: A case report. Clin Case Rep. 2022;10:e6317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Park SI, Yang EJ, Kim DK, Jeong HJ, Kim GC, Sim YJ. Prevalence and Epidemiological Factors Involved in Cellulitis in Korean Patients With Lymphedema. Ann Rehabil Med. 2016;40:326-333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Mubarak M, Rashid R, Shakeel S. Tumor deposits in axillary adipose tissue in patients with breast cancer: Do they matter? World J Clin Cases. 2024;12:1045-1049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Sleigh BC, Manna B. Lymphedema. 2023 Apr 19. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 9. | Armer JM. The problem of post-breast cancer lymphedema: impact and measurement issues. Cancer Invest. 2005;23:76-83. [PubMed] |
| 10. | Cornish BH, Chapman M, Hirst C, Mirolo B, Bunce IH, Ward LC, Thomas BJ. Early diagnosis of lymphedema using multiple frequency bioimpedance. Lymphology. 2001;34:2-11. [PubMed] |
| 11. | Forte AJ, Boczar D, Huayllani MT, Lu X, Ciudad P. Lymphoscintigraphy for Evaluation of Lymphedema Treatment: A Systematic Review. Cureus. 2019;11:e6363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | de Rezende LF, Piloni JPM, Kempa VL, Silva JFR, Vilas Boas VF, Carvalho RL, Marx ÂG. Ultrasonography as an instrument to evaluate lymphedema secondary to breast cancer: systematic review. J Vasc Bras. 2023;22:e20220144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Bergmann A, Baiocchi JMT, de Andrade MFC. Conservative treatment of lymphedema: the state of the art. J Vasc Bras. 2021;20:e20200091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Tatar KK, Turhan B. The effects of complex decongestive therapy on pain and functionality in individuals with breast cancer who developed adhesive capsulitis due to lymphedema: an evaluation by an isokinetic computerized system. Korean J Pain. 2022;35:280-290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Torres Lacomba M, Yuste Sánchez MJ, Zapico Goñi A, Prieto Merino D, Mayoral del Moral O, Cerezo Téllez E, Minayo Mogollón E. Effectiveness of early physiotherapy to prevent lymphoedema after surgery for breast cancer: randomised, single blinded, clinical trial. BMJ. 2010;340:b5396. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 232] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 16. | Liang M, Chen Q, Peng K, Deng L, He L, Hou Y, Zhang Y, Guo J, Mei Z, Li L. Manual lymphatic drainage for lymphedema in patients after breast cancer surgery: A systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99:e23192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 17. | Liu J, Chen D, Yin X. Effect of manual lymphatic drainage combined with vacuum sealing drainage on axillary web syndrome caused by breast cancer surgery. Int Wound J. 2023;20:183-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Sanal-Toprak C, Ozsoy-Unubol T, Bahar-Ozdemir Y, Akyuz G. The efficacy of intermittent pneumatic compression as a substitute for manual lymphatic drainage in complete decongestive therapy in the treatment of breast cancer related lymphedema. Lymphology. 2019;52:82-91. [PubMed] |
| 19. | Hobday A. Use of compression therapy in patients with lymphoedema. Nurs Stand. 2016;30:50-58; quiz 60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Rabe E, Földi E, Gerlach H, Jünger M, Lulay G, Miller A, Protz K, Reich-Schupke S, Schwarz T, Stücker M, Valesky E, Pannier F. Medical compression therapy of the extremities with medical compression stockings (MCS), phlebological compression bandages (PCB), and medical adaptive compression systems (MAC) : S2k guideline of the German Phlebology Society (DGP) in cooperation with the following professional associations: DDG, DGA, DGG, GDL, DGL, BVP. Hautarzt. 2021;72:37-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Rucigaj TP, Huljev D. [The role of short-stretch bandage in therapy of lymphedema]. Acta Med Croatica. 2012;66 Suppl 1:49-51. [PubMed] |
| 22. | de Godoy JM, de Godoy LMP, de Godoy HJP, Guerreiro Godoy MF. Nonelastic Compression Stockings for the Reduction of Lymphedema and the Maintenance of the Results for 2-3 years. Indian J Community Med. 2021;46:329-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 23. | Baklaci M, Eyigör S, Tanıgör G, Özgür İnbat M, Çalışkan Kabayel S. Assessment of Muscle Strength and Volume Changes in Patients with Breast Cancer-Related Lymphedema. Oncol Res Treat. 2020;43:584-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Kilbreath SL, Refshauge KM, Beith JM, Ward LC, Lee M, Simpson JM, Hansen R. Upper limb progressive resistance training and stretching exercises following surgery for early breast cancer: a randomized controlled trial. Breast Cancer Res Treat. 2012;133:667-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 25. | Barufi S, Pereira de Godoy HJ, Pereira de Godoy JM, Guerreiro Godoy MF. Exercising and Compression Mechanism in the Treatment of Lymphedema. Cureus. 2021;13:e16121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Fife CE, Farrow W, Hebert AA, Armer NC, Stewart BR, Cormier JN, Armer JM. Skin and Wound Care in Lymphedema Patients: A Taxonomy, Primer, and Literature Review. Adv Skin Wound Care. 2017;30:305-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Cemal Y, Pusic A, Mehrara BJ. Preventative measures for lymphedema: separating fact from fiction. J Am Coll Surg. 2011;213:543-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 111] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 28. | Bonetti G, Dhuli K, Michelini S, Ricci M, Cestari M, Bertelli M. Dietary supplements in lymphedema. J Prev Med Hyg. 2022;63:E200-E205. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Pecking AP, Février B, Wargon C, Pillion G. Efficacy of Daflon 500 mg in the treatment of lymphedema (secondary to conventional therapy of breast cancer). Angiology. 1997;48:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Senger JB, Kadle RL, Skoracki RJ. Current Concepts in the Management of Primary Lymphedema. Medicina (Kaunas). 2023;59:894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 31. | Schaverien MV, Coroneos CJ. Surgical Treatment of Lymphedema. Plast Reconstr Surg. 2019;144:738-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 130] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country of origin: South Korea
Peer-review report’s classification
Scientific Quality: Grade B, Grade B, Grade C
Novelty: Grade B, Grade B, Grade C
Creativity or Innovation: Grade B, Grade B, Grade C
Scientific Significance: Grade A, Grade B, Grade B
P-Reviewer: Ma C, China; Tari DU, Italy S-Editor: Che XX L-Editor: Wang TQ P-Editor: Li X