Published online May 6, 2024. doi: 10.12998/wjcc.v12.i13.2231
Revised: March 9, 2024
Accepted: March 29, 2024
Published online: May 6, 2024
Processing time: 88 Days and 2.8 Hours
Esophageal cysts are relatively rare in clinical practice, with most of the literature comprising case reports. Esophageal cysts protruding into the thyroid gland are easily misdiagnosed as thyroid tumors. No such cases have been reported so far.
This article reports the case of a 31-year-old adult male diagnosed with thyroid nodules before admission. The patient underwent left thyroidectomy and isthmusectomy. During the surgery, esophageal cysts were identified in the esophageal muscle and thyroid glands. The pathology results confirmed a nodular goiter combined with esophageal cysts. Postoperatively, the patient developed a neck infection and underwent another operation and broad-spectrum antibiotic treatment for recovery.
We report the first clinical case of an esophageal cyst located within the thyroid gland that was successfully treated surgically. Esophageal cyst located within the thyroid gland cause difficulties in diagnosis. In the present study, the contents of the esophageal cysts were calcified foci, and a small amount of fluid mixture, which were easily misdiagnosed as thyroid nodules and misled the surgical methods.
Core Tip: We reported on a very special patient. The diagnosis of a nodular goiter combined with esophageal cysts was made by his symptoms, physical examination, laboratory tests and intraoperative frozen pathological examination. Esophageal cysts embedded in the thyroid gland are rare in clinical practice and can cause difficulties in diagnosis. The patient was successfully treated surgically.
- Citation: Lin HG, Liu M, Huang XY, Liu DS. Intra-thyroid esophageal duplication cyst: A case report. World J Clin Cases 2024; 12(13): 2231-2236
- URL: https://www.wjgnet.com/2307-8960/full/v12/i13/2231.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i13.2231
Esophageal cysts are defined as congenital developmental abnormalities of the esophagus. Esophageal cysts located within the thyroid gland are extremely rarely, and no relevant medical literature of such cases have been reported. This article reports the case of a 31-year-old adult male diagnosed with thyroid nodules before admission. The patient under
The patient underwent thyroid ultrasound which revealed mixed nodule in the isthmus of the thyroid for 5 years.
A 31-year-old man was admitted to the local community hospital. Thyroid color Doppler ultrasound revealed a mixed nodule in the isthmus of the thyroid gland: No abnormalities were found in the right lobe of the thyroid gland (American College of Radiology Thyroid Imaging Reporting and Data System, ACR TR 3), but a solid nodule was found in the left lobe of the thyroid gland (ACR TR 5). The physical examination and laboratory test results were normal, and the patient had no history of swallowing obstruction.
Previously in good health.
Deny bad personal history. Deny family medical history.
Physical examination was unremarkable, and sensation of swallowing obstruction was denied.
The laboratory examination showed that all blood indicators were basically normal.
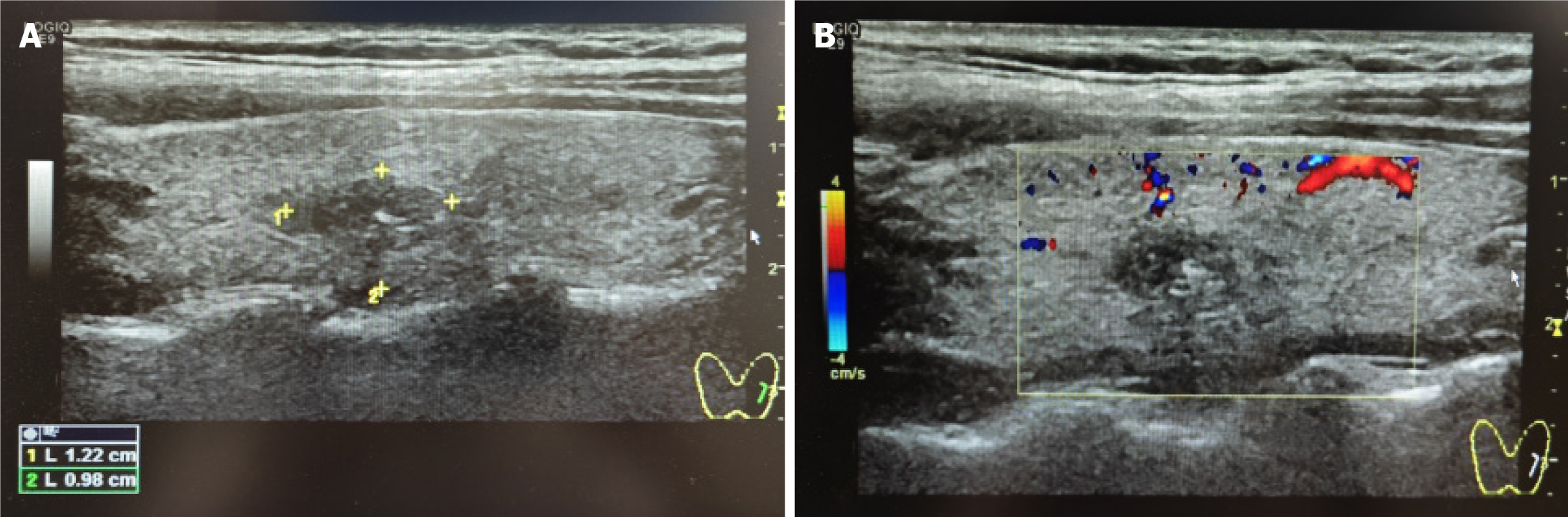
After admission, thyroid color Doppler ultrasound was performed again (Figure 1), and a nodule was located in the middle of the left lobe of the thyroid gland, classified as Thyroid Imaging Reporting and Data System (TI-RADS) 4A. The possibility of nodular goiter combined with calcification was not excluded and fine-needle aspiration (FNA) biopsy was recommended. The other thyroid nodules were classified as TI-RADS 3, considering the nodular goiter.
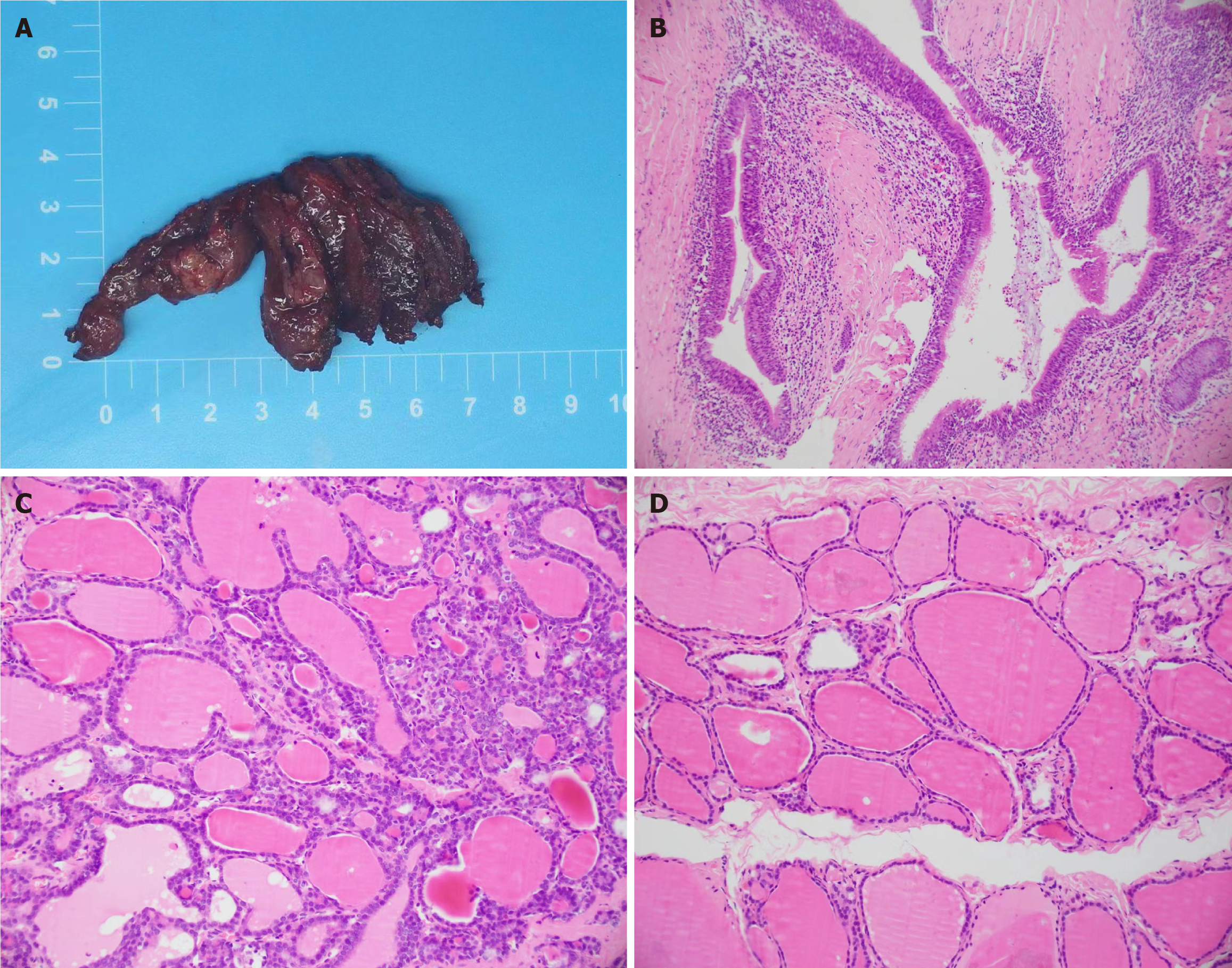
Combined with the paraffin pathology results after the first operation, the final diagnoses was esophageal cyst was embedded in the thyroid gland.
Left thyroid lobectomy and isthmusectomy were performed under general anesthesia with tracheal intubation. Intraoperative frozen pathological examination showed that the nodule in the isthmus of the thyroid gland was consistent with nodular goiter. Furthermore, thyroid tissue was found in the left lobe of the thyroid gland, and a small focus of lymphoepithelial cysts was observed.
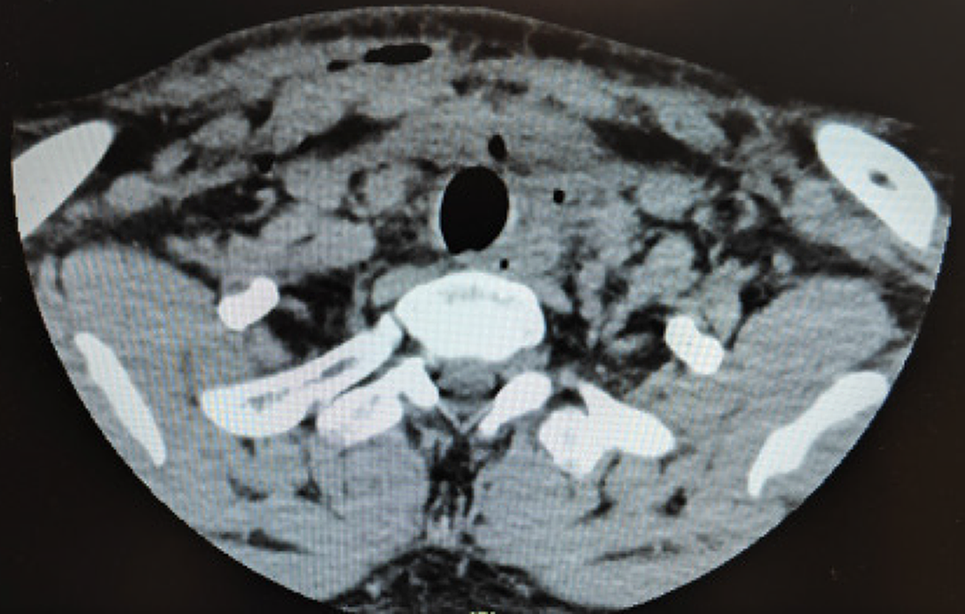
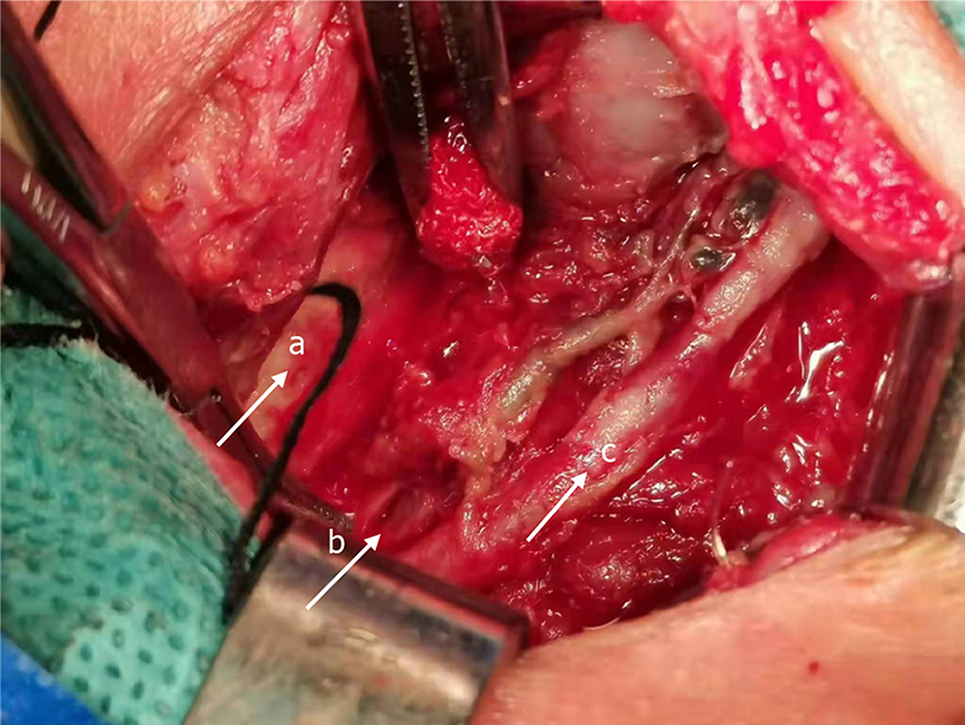
On postoperative day 3, the patient developed redness, swelling, and pain at the surgical site, accompanied by foul-smelling liquid discharge. Body temperature was 38.9 ℃ and routine blood examination showed that the white blood cell count was 10.78 × 109/L, neutrophil percentage was 77.4%, erythrocyte sedimentation rate was 54 mm/h, C-reactive protein was 59.20 mg/L, and calcitonin was 0.06 ng/L. Thyroid computed tomography (CT) revealed multiple scattered free gases in the neck, soft tissue swelling and exudation, and a small local effusion (Figure 2), while esophageal radiography showed no evident fistula signs (Figure 3). Emergency debridement for neck infections was performed in the operating room. A large amount of purulent fluid with a foul smell was observed in the surgical area. The recurrent laryngeal nerve was swollen, and a fistula with a diameter of approximately 4 mm × 5 mm was observed in the muscular layer of the anterior wall of the esophagus (Figure 4). Combined with the preoperative color Doppler ultrasound and paraffin pathology results after the first operation (Figure 5), it was considered that an esophageal cyst was embedded in the thyroid gland, which caused an esophageal fistula after thyroidectomy. The muscular layer of the fistula was sutured using a 3-0 Vicryl absorbable thread, and a drainage tube was left in place at the surgical site after repeated flushing with saline solution. After surgery, gastric tube feeding was performed, and food intake was prohibited. On day 11 after surgery, the gastric tube was removed, and the patient was initiated on a full liquid diet.
One month after surgery, the patient resumed a normal diet and did not experience any discomfort during follow-up for 2 years.
Esophageal cysts are rare in clinical practice, clear data on the true incidence of esophageal cysts are not available[1]. Congenital esophageal cysts can be classified as either duplicate, bronchogenic, gastric, or inclusion body cysts[2]. Esophageal cysts are typically asymptomatic, and 80% of cases are diagnosed in childhood. Cysts that continue to grow can cause esophageal obstruction[3]. Most esophageal cysts are located in the middle and lower parts of the esophagus, and approximately 10% of patients have esophageal cysts that communicate with the esophagus and grow along or attach to it. Surgical resection or endoscopy is the primary treatment for esophageal cysts[4].
Esophageal cysts are defined as congenital malformations of the foregut caused by the abnormal splitting of the posterior part of the embryonic foregut at 3-4 wk of gestation. Their origins may be either esophageal, bronchial, neural, gastrointestinal, and pericardial. Esophageal and bronchial cysts originate from the foregut and contain a ciliated epithelium, making them difficult to distinguish histologically.
Pathologically, the Palmer standard is usually used, which includes: (1) Attachment to the esophageal wall; (2) Presence of gastrointestinal epithelium; and (3) Presence of two layers of the muscularis propria[5].
Esophageal cysts are most commonly found in the mediastinum, and most patients have no clinical symptoms, although some patients may be diagnosed with nonspecific gastrointestinal symptoms during endoscopic examinations[6]. Treatment of asymptomatic patients with esophageal cysts remains controversial. Currently, there are no clear clinical guidelines. Close observation can be performed for small cysts without clinical symptoms; however, complete surgical resection is recommended when the cyst enlarges and compresses the adjacent organs, causing symptoms[7]. Some patients may experience acute symptoms, such as ulcers, bleeding, and infection. This may be due to the presence of gastrointestinal epithelial cells in the cyst[8].
In the present case, the esophageal cyst presented as a thyroid nodule. After surgical resection, pathological results confirmed the presence of an esophageal cyst. The cyst was closely adhered to the esophageal muscularis propria, but was not completely connected to the esophageal lumen. During the initial surgery, the ruptured esophageal muscularis propria was not sutured or repaired that resulted in a postoperative infection, which eventually required a second surgery.
Most esophageal cysts are discovered incidentally. CT and magnetic resonance imaging (MRI) can better show the morphology and relationship with the surrounding tissues. Endoscopic ultrasound (EUS) can further show whether a mass is located in the esophageal muscle layer. EUS-guided FNA (EUS-FNA) can also be used to diagnose tumors qualitatively. However, the complications of EUS-FNA in cystic masses, including infection, bleeding, and mediastinitis, are common, with the incidence reaching as high as 14%. As such, EUS-FNA should not be routinely used for the biopsy of esophageal masses without mucosal abnormalities[9]. The differences in the nature of the cyst contents can also cause difficulties in diagnosis. In the present study, the contents of the esophageal cysts were calcified foci, and a small amount of fluid mixture, which were easily misdiagnosed as thyroid nodules and misled the surgical methods.
Esophageal cysts most commonly found in the mediastinum, and most patients have no clinical symptoms.Most esophageal cysts are discovered incidentally. CT and MRI can better show the morphology and relationship with the surrounding tissues.Esophageal cysts embedded in the thyroid gland are rare in clinical practice and can cause difficulties in diagnosis.Herein, we report the first clinical case of an esophageal cyst located within the thyroid gland that was successfully treated surgically.
We thank the patient for his participation in this study. We have obtained the patient’s support and informed consent form.
| 1. | Wootton-Gorges SL, Eckel GM, Poulos ND, Kappler S, Milstein JM. Duplication of the cervical esophagus: a case report and review of the literature. Pediatr Radiol. 2002;32:533-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Martin JT, Cibull ML, Zwischenberger JB, Reda HK. Infection of an esophageal cyst following endoscopic fine-needle aspiration. Int J Surg Case Rep. 2011;2:144-146. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Eichmann D, Engler S, Oldigs HD, Schroeder H, Partsch CJ. Radiological case of the month. Denouement and discussion: congenital esophageal duplication cyst as a rare cause of neonatal progressive stridor. Arch Pediatr Adolesc Med. 2001;155:1067-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Nelms CD, White R, Matthews BD, Ballinger WE Jr, Sing RF, Heniford BT. Thoracoabdominal esophageal duplication cyst. J Am Coll Surg. 2002;194:674-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Markert DJ, Grumbach K, Haney PJ. Thoracoabdominal duplication cyst: prenatal and postnatal imaging. J Ultrasound Med. 1996;15:333-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Wiechowska-Kozłowska A, Wunsch E, Majewski M, Milkiewicz P. Esophageal duplication cysts: endosonographic findings in asymptomatic patients. World J Gastroenterol. 2012;18:1270-1272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Lee SY, Kim HY, Kim SH, Jung SE, Park KW. Thoracoscopic resection of a cervical esophageal duplication cyst in a 3-month-old infant: a case report. J Pediatr Surg. 2013;48:873-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Lee HS, Jeon HJ, Song CW, Lee SW, Choi JH, Kim CD, Ryu HS, Hyun JH, Lee SY, Kim KT. Esophageal duplication cyst complicated with intramural hematoma--case report. J Korean Med Sci. 1994;9:188-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Wiersema MJ, Vilmann P, Giovannini M, Chang KJ, Wiersema LM. Endosonography-guided fine-needle aspiration biopsy: diagnostic accuracy and complication assessment. Gastroenterology. 1997;112:1087-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 874] [Cited by in RCA: 739] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sharma D, India S-Editor: Zheng XM L-Editor: A P-Editor: Zhao S