Published online Apr 6, 2024. doi: 10.12998/wjcc.v12.i10.1804
Peer-review started: November 14, 2023
First decision: January 23, 2024
Revised: February 5, 2024
Accepted: March 8, 2024
Article in press: March 8, 2024
Published online: April 6, 2024
Processing time: 139 Days and 18.9 Hours
Although percutaneous vertebral augmentation (PVA) is a commonly used pro
A 74-year-old man suffered from low back pain after taking a fall about 3 wk ago. According to physical examination, imaging and laboratory findings, diagnoses of T12 VCF, CKD-MBD, and chronic kidney disease stage 5 were established. He then received percutaneous vertebroplasty at T12 vertebra. Fourteen weeks later, he presented with T12 and L1 vertebral refractures caused by lumbar sprain. Once again, he was given PVA which was optimized for the refractured vertebrae. Al
It is necessary that patients with CKD-MBD who have received PVA are aware of the adverse effects of CKD-MBD. It may increase the risk of vertebral refracture. Furthermore, the PVA surgical technique needs to be optimized according to the condition of the patient. The medium- and long-term effects of PVA remain un
Core Tip: This is a rare case wherein the cemented vertebra and the adjacent vertebra refractured simultaneously in a chronic kidney disease-mineral and bone disorder (CKD-MBD) patient after percutaneous vertebral augmentation (PVA). He was given PVA once more, which was optimized for the refractured vertebrae. While, the medium- and long-term effects were not satisfactory. It is necessary that patients with CKD-MBD who have received PVA are aware of the adverse effects of CKD-MBD.
- Citation: Zhang TD, Cao S, Ren HY, Li YM, Yuan YM. Cemented vertebra and adjacent vertebra refractured in a chronic kidney disease-mineral and bone disorder patient: A case report. World J Clin Cases 2024; 12(10): 1804-1809
- URL: https://www.wjgnet.com/2307-8960/full/v12/i10/1804.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i10.1804
Percutaneous vertebral augmentation (PVA), including percutaneous vertebroplasty (PVP) and percutaneous kypho
The patient was a 74-year-old man who experienced persistent low back pain after taking a fall about 3 wk ago.
The patient took a fall 3 wk ago, and then, he suffered from persistent and drastic lower back pain, and he was barely able to stand and walk.
The patient was diagnosed as having CKD stage 5 in 2006, and since then, he has undergone hemodialysis three times a week and was prescribed oral calcium (1000 mg/d) and calcitriol (0.5 μg/d). The causative disease of CKD was not clear. He was diagnosed with urothelium carcinoma in 2012 and received surgical treatment.
The patient and his family had no history of fragility fracture, and he had no history of chronic low back pain.
Tenderness was found at the thoracolumbar vertebrae, but there were no neurological signs or symptoms. His body mass index was 16.7 kg/m2.
Laboratory examination (Table 1) revealed bone metabolism abnormalities in the patient.
| Serum calcium (mmol/L) | Serum phosphorus (mmol/L) | Parathyroid hormone (pg/mL) | Vitamin D (ng/mL) | Alkaline phosphatase (U/L) | |
| 1st admission | 2.45 | 2.74 | 562.2 | 9.25 | 53 |
| 2nd admission | 2.16 | 1.71 | 557.4 | 8.57 | 60 |
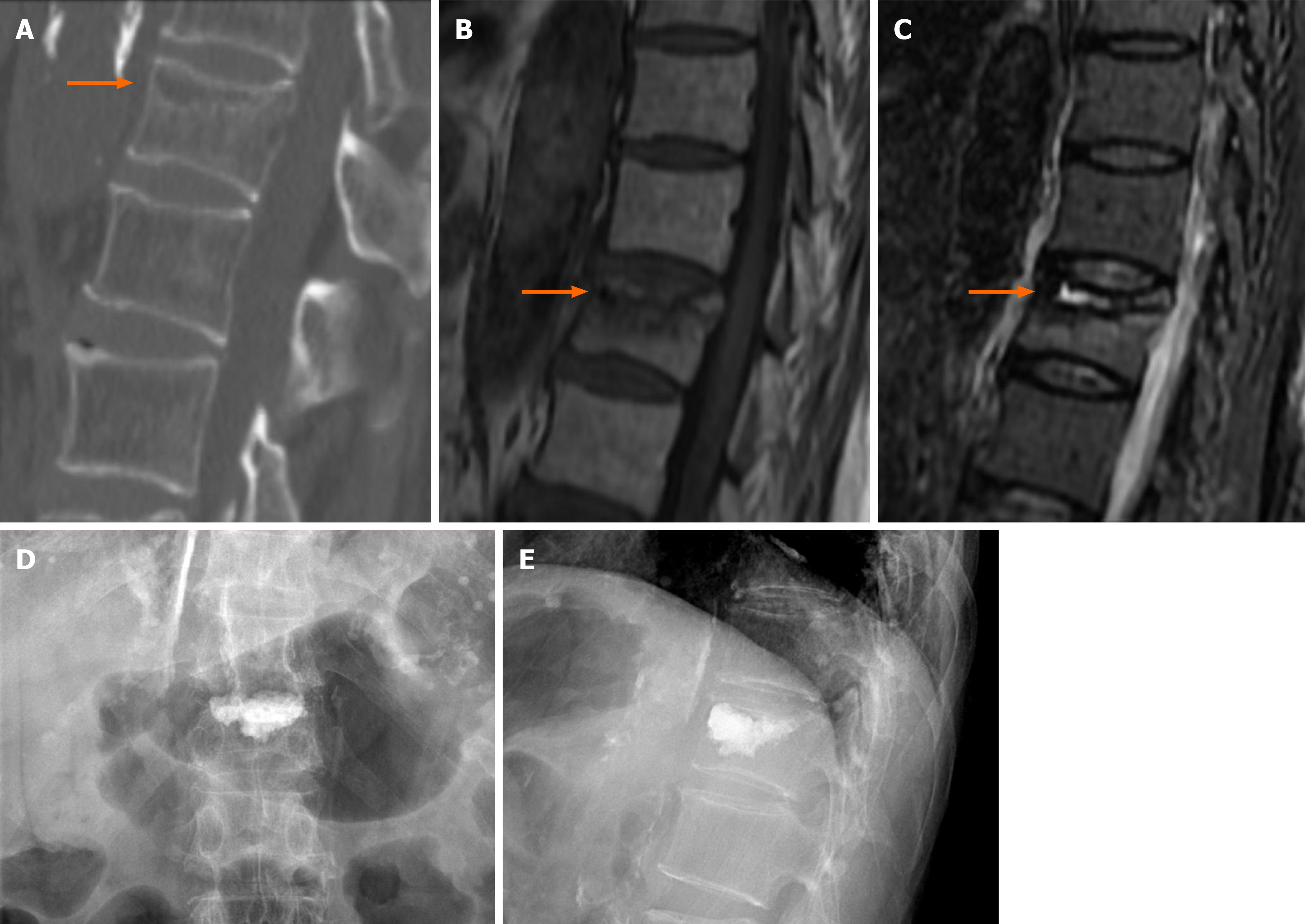
The computed tomography (CT) and magnetic resonance imaging revealed T12 VCF (Figure 1A-C). The L1-L4 bone mineral density (BMD) was 0.922 (T score: -1.3), and the femoral neck BMD was 0.579 (T score: -3.1).
According to the history, physical examination, laboratory and imaging examinations, he was diagnosed as having T12 VCF, CKD-MBD, and CKD stage 5. The secondary causes like hyperparathyroidism, osteomalacia, and malignant tumors were excluded.
He underwent hemodialysis and was prescribed oral medicine as usual. After full preoperative testing and preparation, the patient received T12 PVP (left pedicle approach, cement injection: 3 mL). Typically, the standard procedures of PVP and PKP are the surgical treatment for VCF in patients with CKD-MBD. However, in this case, to fill the intravertebral cleft (IVC; Figure 1, orange arrow) with cement, we penetrated the cleft as precisely as possible during the operation. Postoperatively, the X-ray (Figure 1D and E) revealed that the IVC was filled with the cement without any leakage.
The pain was alleviated significantly on the first postoperative day: The visual analog scale (VAS) score had decreased from 9 to 2, the Oswestry disability index (ODI) score had decreased from 72.5 to 47.5, and he was discharged 3 d later.
During 14th week postoperatively, low back pain occurred again after a lumbar sprain, but he showed no neurological signs or symptoms. CT and bone scan showed T12 and L1 VCFs (Figure 2A-C, thin arrow), the IVC around the injected cement (Figure 2, orange arrow), and the rupture of the posterior vertebral wall (Figure 2, white arrow). The results of the laboratory examination were similar to the previous findings (Table 1). This time, he was diagnosed as having L1 VCF, T12 cemented vertebral refracture, CKD-MBD, and CKD stage 5. After clinical assessment and discussion, we decided to operate again with a further optimized and improved method.
L1 PKP (left pedicle approach, cement injection: 4 mL) was performed as usual, whereas the T12 vertebra was punc
At 1-month follow-up, the VAS score was 2 and ODI was 27.5. The patient complained of chronic low back pain at the 3-month telephonic follow-up, and his VAS score and ODI were found to be 5 and 47.5, respectively. However, owing to loss of follow-up, his imaging examination scheduled to be done at 3-month follow-up could not be performed.
Cemented vertebral refracture rarely co-occurs with the adjacent vertebral refracture after PVA in patients with CKD-MBD. The incidence rate of cemented vertebral refracture is reportedly 0.56%–12.5%[4], and its risk factors include age, low BMD, the IVC, high anterior vertebral height restoration, high Cobb angle restoration, and low cement dose in the previous operation[5]. Furthermore, the rate of adjacent vertebral refracture is reportedly 9.9%–16.2%[6-9], and its risk factors include intradiscal cement leakage[6], low BMD, female[10], exceeded cement injection[10], preoperative segmen
In this case, low BMD and low cement dose in the previous operation may be the factors related to the dual refracture. The minimum volume of cement recommended in the thoracolumbar vertebra is 4–6 mL[11]; however, only 3 mL of the cement was injected in the first operation. In our patient, abnormalities in bone turnover and mineralization caused by CKD-MBD led to low BMD, and we believe this was the most predominant factor resulting in T12 and L1 vertebra re
In the T12 vertebra, IVCs were found both times he was admitted to the hospital. For the first visit at the 3rd week after injury, the abnormality in mineralization and the fracture nonunion caused the formation of the IVC, and its imaging findings were typical[13,14]. At the time of refracture, the IVC formed around the cement again because of abnormal bone mineralization. A large IVC reduced or nullified the strengthening effect of the cement, and the cement even made the vertebra more unstable, thus leading to a fracture even after a minor traumatic injury.
For the L1 vertebra, the low BMD and biomechanical changes of the adjacent vertebra[15] together resulted in the refracture. Thus, the refractures of the vertebrae in this case were both related to the abnormal bone mineralization and low BMD caused by CKD-MBD.
The distribution of cement and filling with cement in the IVC may reportedly influence the clinical outcome[16,17]. In the first operation, we did our best to ensure that the IVC was full of cement and there was sufficient cement distribution. According to the CT findings (Figure 2A and B) acquired after the refracture, although the IVC was completely filled with the cement, the cement was not distributed well. Meanwhile, a larger IVC formed in T12 vertebra, which was accom
The findings of Mo et al[18] and Li et al[19] establish that cement distribution is associated with the degree of post
Taken together, we consider the following factors to have contributed to the refractures: low BMD, abnormal bone turnover, and abnormal bone mineralization caused by CKD-MBD. These led to the formation of IVCs and may explain why the efficacy was not satisfactory at the last follow-up. The limitation of the case was that bone turnover markers were not tested at the time of admission.
For the PVA treatment in patients with CKD-MBD, it is necessary to be aware of the adverse effects of CKD-MBD. It may increase the risk of vertebral refracture. PVA surgical technique needed to be optimized according to the condition of the patient. The medium- and long-term treatment effects of PVA may still be uncertain in patients with CKD-MBD.
| 1. | Vilaca T, Salam S, Schini M, Harnan S, Sutton A, Poku E, Allen IE, Cummings SR, Eastell R. Risks of Hip and Nonvertebral Fractures in Patients With CKD G3a-G5D: A Systematic Review and Meta-analysis. Am J Kidney Dis. 2020;76:521-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 2. | West SL, Lok CE, Jamal SA. Fracture Risk Assessment in Chronic Kidney Disease, Prospective Testing Under Real World Environments (FRACTURE): a prospective study. BMC Nephrol. 2010;11:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Chen H, Yang H, Jia P, Bao L, Tang H. Effectiveness of kyphoplasty in the treatment of osteoporotic vertebral compression fracture patients with chronic kidney disease. J Orthop Sci. 2016;21:571-578. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Li YX, Guo DQ, Zhang SC, Liang D, Yuan K, Mo GY, Li DX, Guo HZ, Tang Y, Luo PJ. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42:2131-2139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 87] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 5. | Zhu S, Su Q, Zhang Y, Sun Z, Yin P, Hai Y. Risk factors of cemented vertebral refracture after percutaneous vertebral augmentation: a systematic review and meta-analysis. Neuroradiology. 2020;62:1353-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Ko BS, Cho KJ, Park JW. Early Adjacent Vertebral Fractures after Balloon Kyphoplasty for Osteoporotic Vertebral Compression Fractures. Asian Spine J. 2019;13:210-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Yang W, Yang J, Liang M. Percutaneous Vertebroplasty Does Not Increase the Incidence of New Fractures in Adjacent and Nonadjacent Vertebral Bodies. Clin Spine Surg. 2019;32:E99-E106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Spross C, Aghayev E, Kocher R, Röder C, Forster T, Kuelling FA. Incidence and risk factors for early adjacent vertebral fractures after balloon kyphoplasty for osteoporotic fractures: analysis of the SWISSspine registry. Eur Spine J. 2014;23:1332-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003;226:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 430] [Cited by in RCA: 407] [Article Influence: 17.7] [Reference Citation Analysis (1)] |
| 10. | Hu L, Sun H, Wang H, Cai J, Tao Y, Feng X, Wang Y. Cement injection and postoperative vertebral fractures during vertebroplasty. J Orthop Surg Res. 2019;14:228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Martinčič D, Brojan M, Kosel F, Štern D, Vrtovec T, Antolič V, Vengust R. Minimum cement volume for vertebroplasty. Int Orthop. 2015;39:727-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Chen B, Fan S, Zhao F. Percutaneous balloon kyphoplasty of osteoporotic vertebral compression fractures with intravertebral cleft. Indian J Orthop. 2014;48:53-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Qi H, Qi J, Sun Y, Gao J, Sun J, Wang G. Bone microarchitecture and metabolism in elderly male patients with signs of intravertebral cleft on MRI. Eur Radiol. 2022;32:3931-3943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Wang C, Zhang X, Liu J, Shan Z, Li S, Zhao F. Percutaneous kyphoplasty: Risk Factors for Recollapse of Cemented Vertebrae. World Neurosurg. 2019;130:e307-e315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Boger A, Heini P, Windolf M, Schneider E. Adjacent vertebral failure after vertebroplasty: a biomechanical study of low-modulus PMMA cement. Eur Spine J. 2007;16:2118-2125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 108] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 16. | Lv NN, Hou MZ, Zhou ZZ, Feng XX, Liu HJ, Shan FR, Li EH, Guan BY, He SJ, Liu MM. Does the Relationship Between Bone Cement and the Intravertebral Cleft of Kummell Disease Affect the Efficacy of PKP? World Neurosurg. 2022;160:e430-e435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Yu W, Xiao X, Zhang J, Li Z, Wang X, Tang F, Jiang X, Zhong Y. Cement Distribution Patterns in Osteoporotic Vertebral Compression Fractures with Intravertebral Cleft: Effect on Therapeutic Efficacy. World Neurosurg. 2019;123:e408-e415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Mo L, Wu Z, Liang D, Y L, Cai Z, Huang J, Lin S, Cui J, Zhang S, Yang Z, Yao Z, Jiang X. Influence of bone cement distribution on outcomes following percutaneous vertebroplasty: a retrospective matched-cohort study. J Int Med Res. 2021;49:3000605211022287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Li Q, Long X, Wang Y, Guan T, Fang X, Guo D, Lv J, Hu X, Jiang X, Cai L. Clinical observation of two bone cement distribution modes after percutaneous vertebroplasty for osteoporotic vertebral compression fractures. BMC Musculoskelet Disord. 2021;22:577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Ohashi N, Japan; Sanyal D, India S-Editor: Gong ZM L-Editor: A P-Editor: Xu ZH