Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.1939
Peer-review started: December 6, 2022
First decision: December 26, 2022
Revised: January 18, 2023
Accepted: February 27, 2023
Article in press: February 27, 2023
Published online: March 26, 2023
Processing time: 100 Days and 16.8 Hours
Situs inversus (SI) is a rare congenital condition characterized by a mirror-image transposition of the major visceral organs. Since the 1990s, more than one hundred SI patients have been reported to have successfully undergone laparoscopic cholecystectomy. In these cases, the major problem is to overcome is the left-right condition for right-handed surgeons. Laparoscopic common bile duct exploration (LCBDE), an alternative to treat patients with bile duct stones, has shown equivalent efficacy and is less likely to cause pancreatitis than endoscopic retrograde cholangiopancreatography. Recent updated meta-analyses revealed that a shorter postoperative hospital stay, fewer procedural interventions, cost-effectiveness, a higher stone clearance rate, and fewer perioperative complications are additional advantages of LCBDE. However, the technique is technically demanding, even for skilled laparoscopic surgeons. Conducting LCBDE in patients with difficult situations, such as SI, is more complex than usual. We herein review published SI patients with choledocholithiasis treated by LCBDE, including our own experience, and this paper focuses on the technical aspects.
Core Tip: Laparoscopic common bile duct exploration (LCBDE) is an alternative option to treat choledocholithiasis. Compared to endoscopic retrograde cholangiopancreatography, it has been demonstrated that LCBDE has resulted in shorter hospital stays, fewer procedures, and greater cost-effectiveness in recent studies. Nevertheless, LCBDE is a technically demanding procedure. It is even more challenging in difficult circumstances such as situs inversus (SI). Herein, we present an analysis of published SI patients with choledocholithiasis treated by LCBDE and our own case, and this paper focuses on the technical aspects.
- Citation: Chiu BY, Chuang SH, Chuang SC, Kuo KK. Laparoscopic common bile duct exploration to treat choledocholithiasis in situs inversus patients: A technical review. World J Clin Cases 2023; 11(9): 1939-1950
- URL: https://www.wjgnet.com/2307-8960/full/v11/i9/1939.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i9.1939
For more than two decades, laparoscopic common bile duct exploration (LCBDE) and endoscopic retrograde cholangiopancreatography (ERCP) with stone removal have been widely accepted techniques for managing common bile duct (CBD) stones[1-3]. As LCBDE is a technically demanding procedure, ERCP has gradually become mainstream in clinical practice. In 2018, an updated network meta-analysis including 13 trials and 1757 patients revealed that laparoscopic cholecystectomy (LC) plus LCBDE had better outcomes than LC plus ERCP in terms of not only length of hospital stay but also stone clearance rate and perioperative complications[4]. Other studies exhibited inconsistent results[3,5,6]. The trend in favor of ERCP resulted in decreased familiarity with LCBDE by surgeons. The complex steps and delicate tools used in LCBDE also make it challenging to perform.
Situs inversus (SI) is a rare condition causing left-right positioning of thoracic and abdominal organs[7]. Clinically, SI by itself is asymptomatic; however, when it is associated with CBD stones, the diagnosis can be challenging due to the reversed anatomical location[8]. This is also true for LC and LCBDE. As LC in SI has been studied in two meta-analyses[9,10], LCBDE in SI is limited to a small number of case reports. This review is aimed at assessing published SI patients treated by LCBDE and shares our own experience in the technical aspects.
A search for all articles regarding CBD exploration in patients with SI was conducted in The Cochrane Library, PubMed, Embase, and Web of Science without language restriction until October 5, 2022. The keywords used were “Situs inversus” plus “laparoscopic bile duct exploration”, “choledocholithotripsy”, “choledocholithotomy”, “choledocholithiasis”, and “bile duct stone”. All relevant studies reporting one or more cases of CBD stone exploration in SI that were found as full texts, structured abstracts or conference reports were included. Studies that described procedures conducted in open surgery or other than CBD exploration were excluded. Duplications of the same patient reported in different studies were also excluded. A total of 12 records were identified by the literature search. In accordance with the study exclusion criteria, two articles were excluded for reporting the same patient[11,12], and the other two articles were excluded for open surgery[13,14]. Finally, eight case reports were included in this review[8,15-21]. The detailed information is presented in Tables 1-3.
| Ref. | Year | Age | Sex | Medical history | Presentation | Diagnostic tools for CBD stone | Preoperative intervention |
| Kang et al[21] | 2004 | 64 | F | Atrial fibrillation | Jaundice, abnormal liver function | Echo, CT, MRCP | Nil |
| Tai et al[20] | 2004 | NA | F | Arrhythmia with pacemaker implantation | NA | NA | ERCP |
| Weber-Sánchez et al[15] | 2011 | 60 | M | NA | Jaundice, cholecystitis | NA | NA |
| Han et al[16] | 2012 | 71 | F | NA | NA | CT | ERCP |
| Liu et al[8] | 2017 | 51 | F | Nil | Cholecystitis, abnormal liver function | CT, MRCP | Nil |
| Senthilnathan et al[17] | 2017 | 76 | F | Gallbladder stone s/p open cholecystectomy | NA | NA | ERCP |
| Takalkar et al[19] | 2018 | 50 | F | NA | Jaundice, abnormal liver function, cholecystitis | Echo, MRCP | ERCP + ERBD |
| Simkhada et al[18] | 2021 | 63 | F | HTN, hypothyroidism, CKD | NA | MRCP | ERCP |
| Our case | 2022 | 79 | F | HTN, hyperlipidemia, DM, CKD, ectopic pregnancy | Jaundice, abnormal liver function, cholecystitis | CT | Nil |
| Ref. | Year | IOC | Incision number | Style | Position | Surgeon site | Working hand | Choledochoscopy | CBDE route | Approach technique |
| Kang et al[21] | 2004 | N | 4 | MirA | NA | Right side | Left | Yes | Choledochotomy with T-tube closure | Choledochoscopy |
| Tai et al[20] | 2004 | N | 4a | NA | NA | NA | NA | NA | NA | NA |
| Weber-Sánchez et al[15] | 2011 | N | 4a | NA | NA | NA | NA | NA | NA | NA |
| Han et al[16] | 2012 | N | 4 | MirCon | NA | NA | NA | Yes | Choledochotomy | Choledochoscopy |
| Liu et al[8] | 2017 | N | 4a | NA | NA | NA | NA | NA | NA | NA |
| Senthilnathan et al[17] | 2017 | Y | 4 | MirCon | Supine, split legs | Between legs | NA | No | Choledochotomy with CDDb | Balloon and saline sweep |
| Takalkar et al[19] | 2018 | N | 4 | MirA | NA | NA | NA | No | Choledochotomy with CDDc | NA |
| Simkhada et al[18] | 2021 | N | 4 | MirA | Lithotomy | Right side | Left | Yes | Choledochotomy with primary closure | Endo-forceps |
| Our case | 2022 | Y | 1 | SP | Reverse Trendelenburg | Right side | Right | No | Transcystic approach | Basket in catheter |
| Ref. | Year | OP time (min) | Conversion | PLOS (d) | Complication | Mortality | Follow-up (mo) |
| Kang et al[21] | 2004 | 240 | No | NA | NA | Nil | Nil |
| Tai et al[20] | 2004 | NA | No | NA | Nil | Nil | Nil |
| Weber-Sánchez et al[15] | 2011 | NA | No | NA | NA | Nil | Nil |
| Han et al[16] | 2012 | 129 | No | NA | Nil | Nil | Nil |
| Liu et al[8] | 2017 | NA | No | 5 | Nil | Nil | Nil |
| Senthilnathan et al[17] | 2017 | NA | No | 7 | Nil | Nil | Nil |
| Takalkar et al[19] | 2018 | NA | No | NA | NA | Nil | Nil |
| Simkhada et al[18] | 2021 | NA | No | NA | NA | Nil | Nil |
| Our case | 2022 | 152 | No | 3 | Nil | Nil | 24.5 |
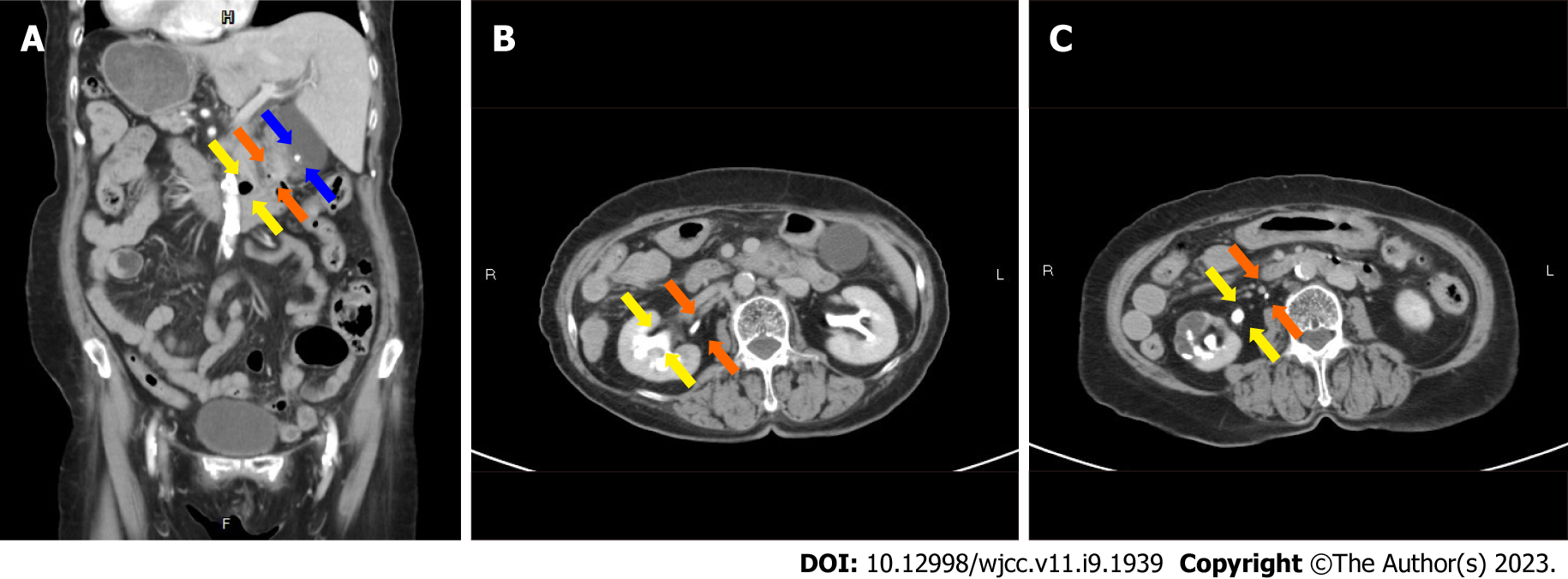
A 79-year-old female with SI had underlying hypertension, type II diabetes mellitus, dyslipidemia, and an operation history of ectopic pregnancy 50 years prior. This time, she suffered from postprandial epigastric pain accompanied by a jaundice episode 5 d before her medical seeking. At the emergency room, physical examination was unremarkable. Laboratory values showed white blood cell 7,200/mm (normal range: 4000–10000), C-reactive protein 33.31 mg/dL (0–8), total bilirubin 1.17 mg/dL (1.0–2.0), direct bilirubin 0.5 mg/dL (0.2–1), alanine transaminase 39 IU/L (10–40), aspartate aminotransferase 89 IU/L (10–42), and alkaline phosphatase 147 IU/L (28–94). Abdominal computed tomography (CT) showed cholelithiasis and choledocholithiasis in the distal CBD (Figure 1A and B). Other anomalies included distal CBD draining into the duodenal 3rd portion, duplication of the right ureter, and right hydroureteronephrosis (Figure 1A and C). Under the impression of acute calculous cholecystitis and choledocholithiasis with obstructive jaundice and liver function impairment, she was admitted for single-incision LC and LCBDE. The detailed surgical procedure is discussed below, and the patient’s postoperative recovery was uneventful. She was discharged on the 3rd postoperative day. No complications occurred after a 24.5-mo follow-up.
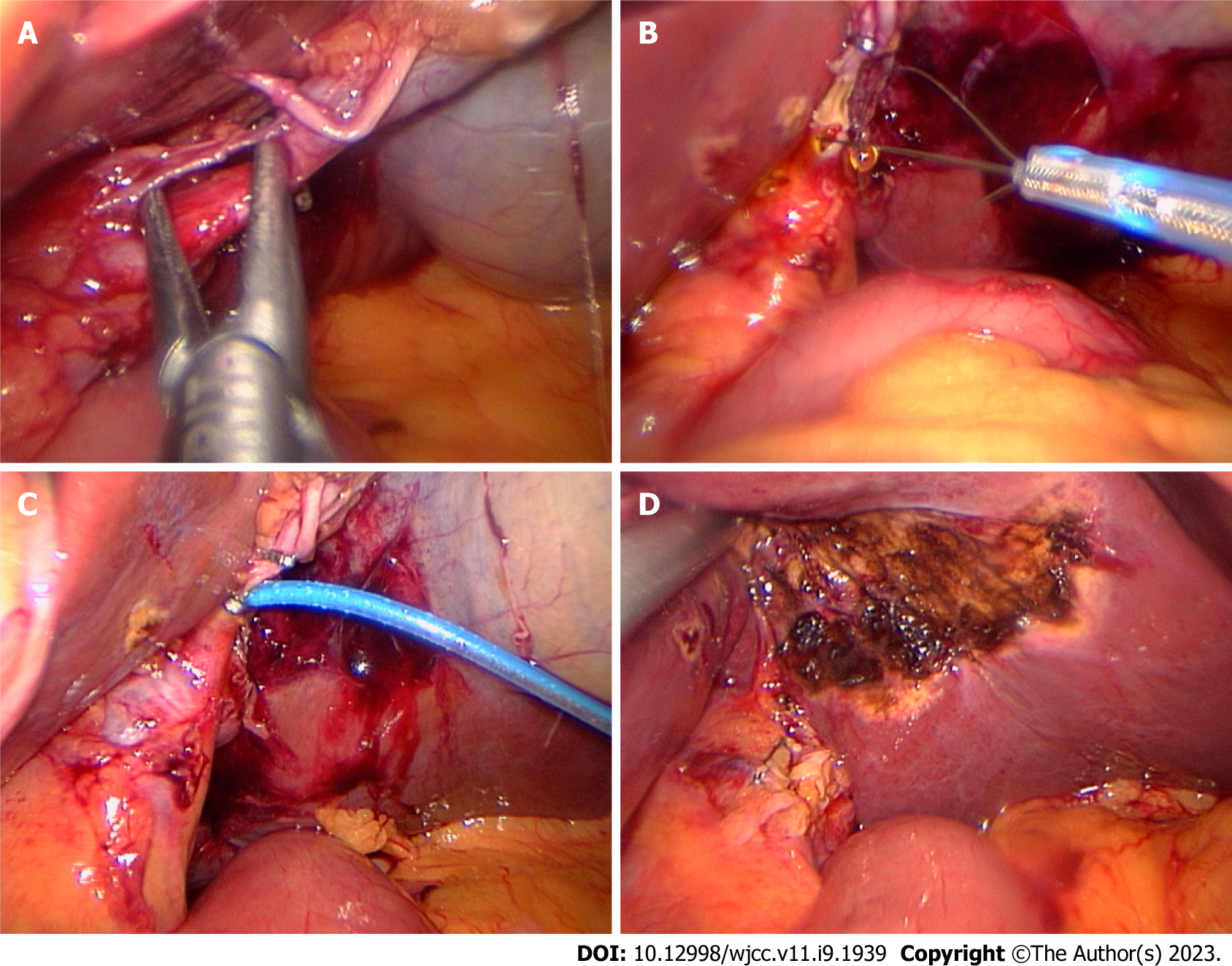
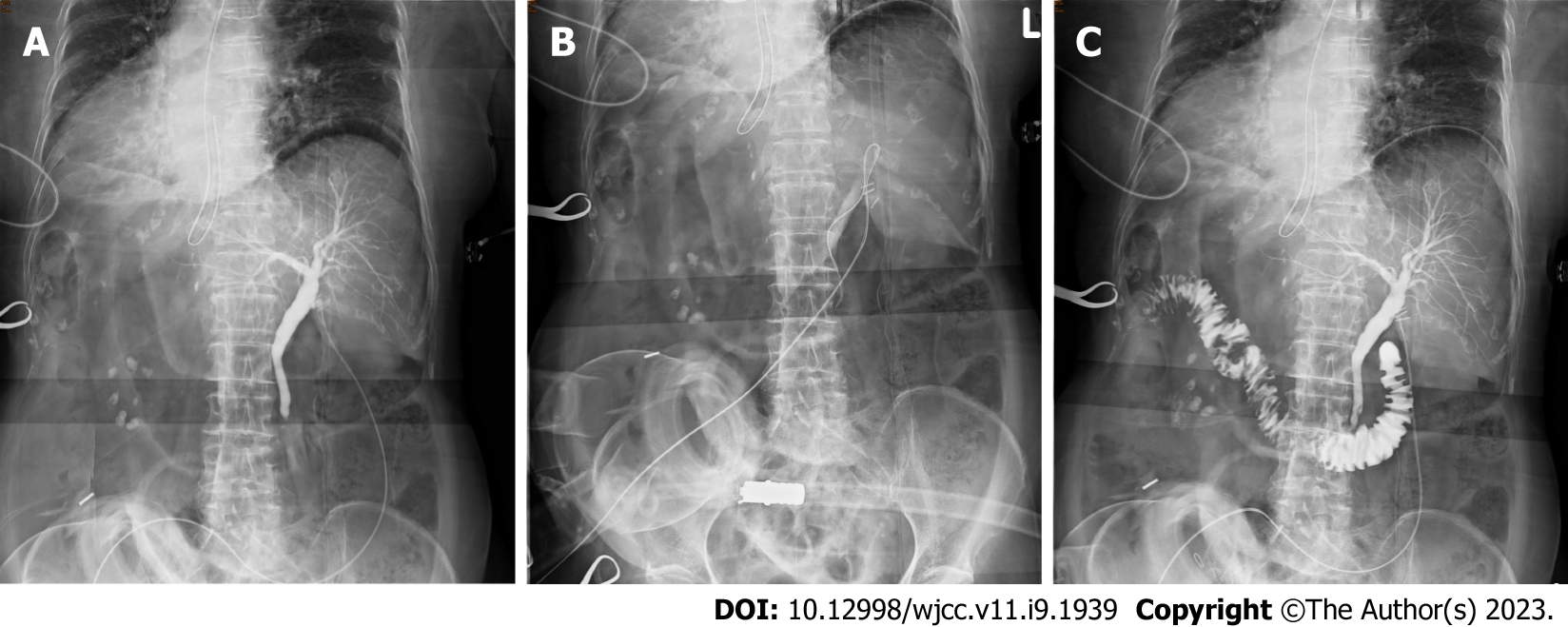
The single-incision LCBDE (SILCBDE) technique has been described in detail previously[22,23]. The patient was given general anesthesia and placed in the reverse Trendelenburg position. The surgeon and the assistant stood on the right side of the patient owing to the mirror positioning of the intraabdominal organs. The surgery began with the insertion of a commercial multichannel port through a 2 cm left paraumbilical incision. A 5-mm atraumatic grasper was inserted through the left 5-mm port to retract the gallbladder to the 2 o’clock direction. A 5-mm 50-cm-long 30-degree laparoscope was passed through the lower 12-mm port to provide visualization. The working ports were served by the upper 12-mm and right 5-mm ports. After dissecting Calot’s triangle (Figure 2A) and securing the proximal cystic duct, a small incision was made into the cystic duct, and a 5 French feeding tube was passed into the nondilated cystic duct (Figure 2B and C). We conducted a diagnostic intraoperative cholangiogram (IOC), and distal CBD stones were confirmed (Figure 3A). Then, we used a modified technique named "basket-in-catheter"(BIC)[24]: The Dormia basket was inserted into a six French feeding tube and then went forward to the predestined distance. After entering the distal CBD, the basket was opened to trap the stone (Figures 2B and 3B). After stone clearance, completion IOC was performed to confirm that there were no retained stones (Figure 3C). Finally, the cystic duct was closed, and the gallbladder was detached from the liver bed (Figure 2D) with a closed suction drain left in the subhepatic space. The surgery took 152 min with an estimated blood loss of 5 ml. The details of the operation are shown in the Video.
SI is a rare defect of situs orientation. As SI fails to generate normal left-right asymmetry, it results in a spectrum of laterality disturbances[25]. The most common of these is immotile cilia syndrome, known as Kartagener syndrome[26-28]. Ivemark’s syndrome, cardiac malformation and biliary atresia are also found in patients with SI[29-31]. In our case, duplication of the right ureter and abnormal insertion of the distal CBD into the 3rd portion of the duodenum were found on CT (Figures 1 and 3C). Although their association with SI remains unclear[32,33], we should always pay attention to SI patients to identify possible anomalies in preoperative surveys.
A total of 9 case reports including our case, was comprised of eight women and one man with ages ranging from 50 to 79 years of age, as detailed in Table 1. Systemic disease was reported in four patients[18,20,21], and one of them was equipped with a pacemaker[20]. One patient had an ectopic pregnancy history. Also, one patient had undergone LC before, but residual gallbladder and CBD stones were found six months later[17]. The presentation in four of these patients was jaundice[15,19,21], while four patients developed cholecystitis[8,15,19]. Additional high-resolution imaging was used to assess the abdominal anatomy in six patients: Two patients underwent abdominal CT only[16], magnetic resonance cholangiopancreatography (MRCP) was used in two cases[18,19], and two patients underwent both CT and MRCP[8,21].
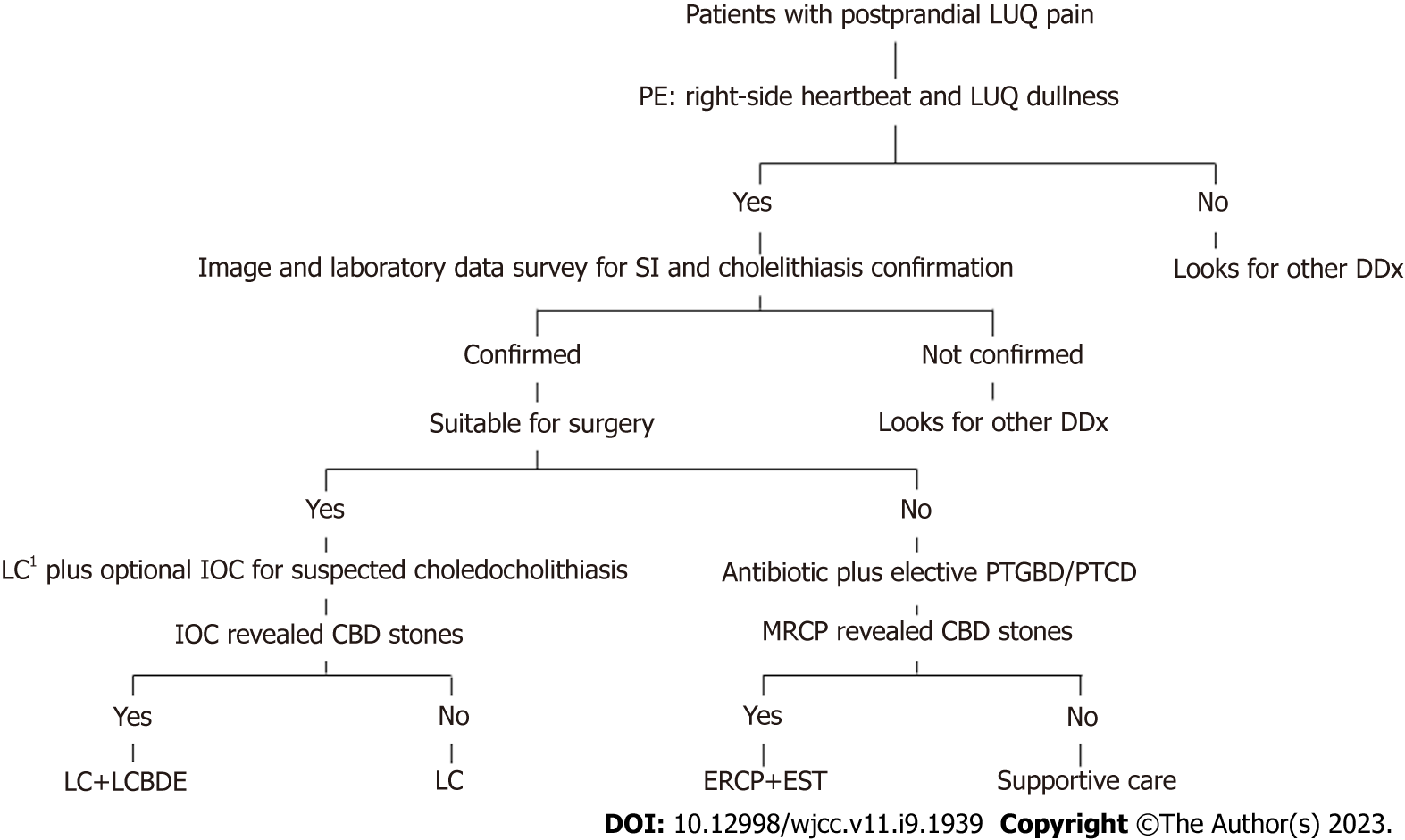
Due to the left-right presentation of SI, a timely diagnosis of acute abdominal diseases in SI patients is difficult for emergency physicians[34,35]. Liu et al[8] reported a 15-d delay diagnosis of acute cholangitis[8]. For patients with postprandial left upper abdominal pain, physical examination is needed to reveal a heartbeat in the right hemithorax and hepatic dullness in the left upper abdomen so that cholelithiasis associated with SI can be considered in addition to acute myocardial infarction or a peptic ulcer. In patients with uncertain features, a careful physical examination with radiological investigations plays a significant role in SI diagnosis[36,37]. Here, we propose a practical algorithm for the diagnosis and management of cholelithiasis and choledocholithiasis in SI patients (Figure 4).
Patients with SI also pose significant challenges to endoscopists and surgeons[38-42]. ERCP is one of the most challenging procedures in SI patients. Given the reversed anatomy, a 180-degree clockwise rotation in the duodenum is often required[43-47]. Furthermore, cannulation to the bile duct is difficult because of the lack of visualization and the ectopic location of the ampulla of Vater in SI patients[7]. In 2022, Ding et al[48] published a case series containing 14 patients with SI undergoing ERCP. The rate of successful cannulation was 85.7% (12/14), while difficult cannulation occurred in 71.4% (10/14) of those patients[48]. Although the literature review until 2021 revealed a 100% cannulation success of 41 patients[48], one of five cases reported in 2022 failed[49-52]. Plus there were 5 failed cases in our literature review, and the overall success rate was 87.7%. Compared to ERCP, LCBDE provides full intraperitoneal visualization. In the five case reports of our literature review, all the patients had successful LCBDE after failed ERCP, and the former might be a better option to treat choledocholithiasis in SI patients.
In addition to our case, the operative time was only shown in two more patients: 240 min[21] and 129 min[16]. Postoperative hospital stay was also recorded in two other patients as five days[8] and seven days[17]. While we spent 152 min to complete the SILCBDE, the postoperative hospital stay was only three days. Of these patients, no conversion, complication, or mortality was recorded. The detailed operative results are presented in Table 3.
Conducting laparoscopic surgery in SI patients is also difficult owing to the transposed organs[53-55]. The first consideration is trocar positioning. There are essentially two types of laparoscopic port placements in SI patients: The “American mirror technique” and the “French mirror technique”[9,10]. Surgeons can choose either of them depending on their discretion. In most of the case reports in our review, the “American mirror technique” was used, while some authors ambiguously described it as a “conventional technique” that could be the “American mirror technique” or “French mirror technique”. The handedness of the surgeons is the second problem[56,57]. Surgeons use their left hand for dissection via the epigastric port and use the right hand for the midclavicular port. As most surgeons are right-handed, using the left hand will not be precise and may pose danger. In using the right hand, however, the surgeon will have to cross the patient’s body to perform the dissection[10]. To address this dilemma, a systemic review showed that left-handed surgeons yielded shorter intervention times than right-handed surgeons during LC of SI patients[9]. However, there were only seven left-handed surgeons in 121 cases in this study. While most surgical procedures are designed for right-handed surgeons, it is not uncommon for left-handed surgeons to use their right hand as the working hand in daily practice[58,59]. Using a nondominant hand might not have much impact on the surgical outcome.
In our literature review of LCBDE in SI patients (Table 2), although some of the patients ambiguously described their operative technique as "conventional"[8,15,20], most of them reported a four-port technique with the American mirror style[18,19,21]. Our patient is the only case treated by SILCBDE.
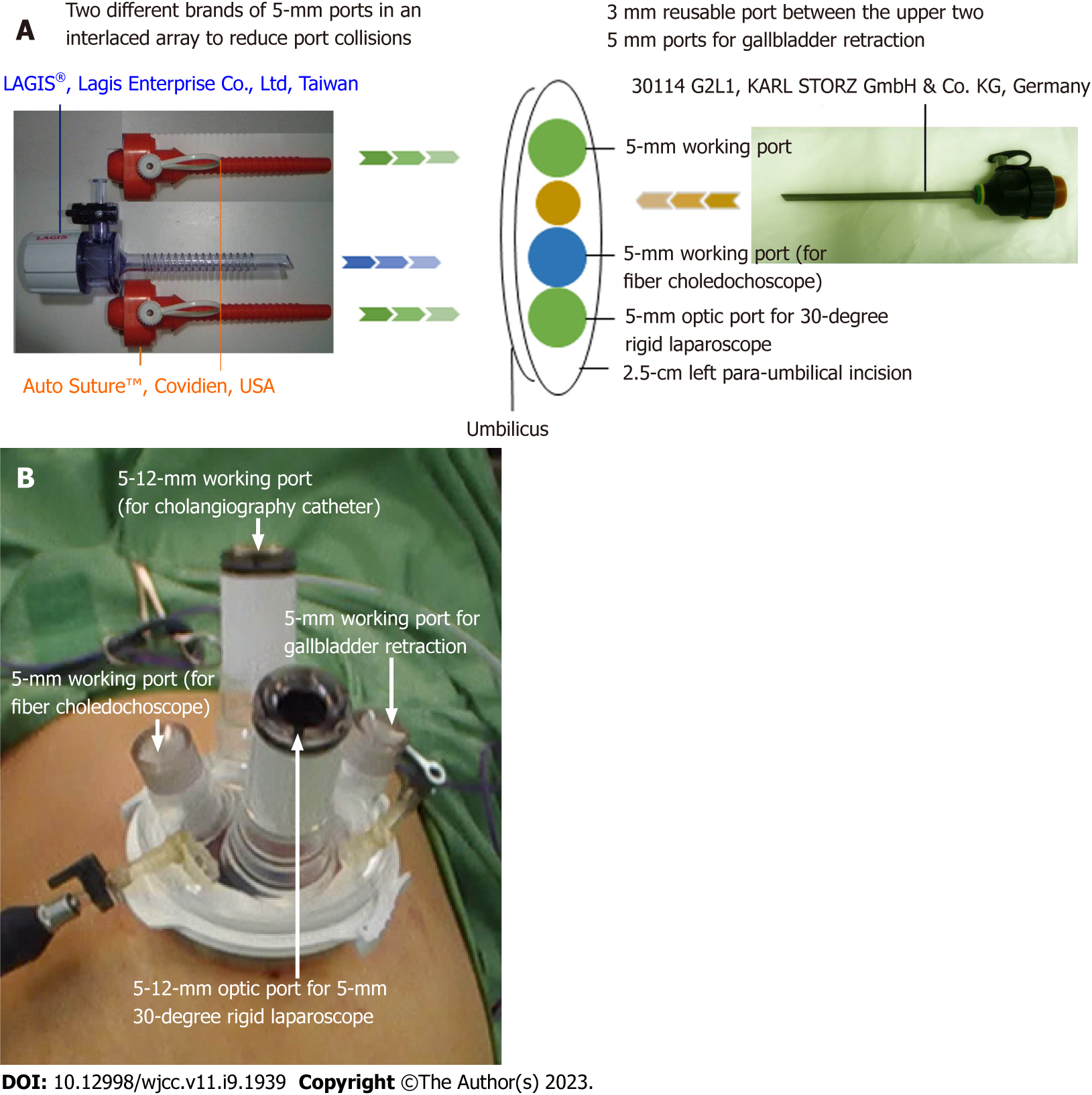
Compared with the difficulty in LCBDE for SI patients, SILCBDE seems to have some advantages. We developed this novel technique in July 2012, and it soon became our standard of care for choledocholithiasis, including difficult situations such as Mirizzi syndrome Csendes type II-IV[22,23,60]. In addition to a 5-mm 50-cm-long 30-degree laparoscope and a 5-mm flexible fiber choledochosope set, only conventional straight laparoscopic instruments were needed. Either the single-incision multiple-port longitudinal-array technique[61] or a commercial multichannel port could be used at the surgeon’s discretion (Figure 5). This procedure is indicated for every patient with choledocholithiasis who can tolerate regular laparoscopic surgery. While SILCBDE is selected for SI patients, the mirror position of trocars is unnecessary because only one single port was used. The handedness problem is invalid, as dissection can be performed by the right hand, and the left hand can be used for gallbladder traction[62-65]. It has little adverse effect in our technique as well, while gallbladder traction is usually carried out by the assistant[22,23,66]. Additionally, SILCBDE decreases incisional trauma and postoperative pain, speeds recovery and provides favorable cosmesis. The only modification needed is the positions of operators and assistants, which should be moved from the patient’s left side to the right side. Since our surgeon is an experienced surgeon who has performed more than 100 SILCBDEs[22], the risk of major complications is minimal. Our patient also attained the shortest postoperative stay in this review.
Another issue in SI undergoing LCBDE is the approach route. The laparoscopic approach for CBD stones can be categorized into transcystic exploration and choledochotomy[67]. The location, number, and size of the CBD stones along with the anatomy of the cystic duct and the CBD influence the choice between these two techniques[68]. For example, small distal stones (≤ 6 mm diameter) are more suitable for the transcystic approach; choledochotomy can be considered if the CBD is larger than 7 mm or intrahepatic duct stones exist[67]. In our literature review, choledochoscopy was used in three patients to conduct bile duct exploration[16,18,21]. Five patients underwent choledochotomy that closed by one T-tube drainage[21], one patient had primary closure[18], two patients had choledochoduodenostomies[17,19], and the remaining one patient had an unmentioned repair[16]. The only transcystic approach was applied in our case. Balloon and saline sweeping was used in one case[17], and we used a basket in a catheter to remove the bile duct stone (Table 2).
Although many studies have reported that transcystic approaches have shorter postoperative hospital stays and fewer bile leaks than choledochotomies[69-72], in most of the cases in our review, the latter was used. Senthilnathan et al[17] mentioned that a residual gallbladder containing small calculi was found six months after LC in an SI patient[17]. CBD stones were also exhibited at the same time, which might have migrated from the cystic duct. In this situation, a transcystic approach might be a better option to detect and remove retained cystic duct stones that could be missed by choledochotomy. Our patient is the only case in which a transcystic approach was applied in this review. We showed that SILCBDE with a transcytic approach can be performed successfully in an SI patient. In addition, we used a modified technique named BIC[24]. As choledochoscopy is a delicate device and could be under repair at times, BIC can be performed easily by using a small feeding tube and a stone basket. In our experience, it could achieve stone clearance in nearly half of simple CBD stone cases (data unpublished). With these novel techniques, an SI patient with choledocholithiasis can experience the least invasive LCBDE approach. In our case, SILCBDE via a transcystic approach using a modified BIC technique took 152 min to complete, similar to other cases in this review. After a 24.5-mo follow-up, no late complications or stone recurrence were identified.
There are several limitations to our study that must be acknowledged. First, due to the rarity of such cases, the number of included cases is very limited. The conclusion might be considered expert opinions, relatively low-quality evidence. Second, cases included in our review were published between 2004 and 2022. Bias could occur because of the advances in techniques and instruments used, which results in consistent cohort heterogeneity. Finally, missing data were encountered in most of the patients, and therefore, some important issues were difficult to address. For example, information on the postoperative length of hospital stay and complications was only available for three (33.3%) and five (55.6%) patients, respectively.
Both ERCP and LCBDE are valid options to treat choledocholithiasis by experienced endoscopists and surgeons. Although there are no related comparative studies, LCBDE seems to be superior to ERCP for SI patients in terms of better intraperitoneal visualization and a lower failure rate. In SI patients, some difficulties of conventional multiport laparoscopic surgical techniques could be overcome by SILCBDE. The transcystic approach and a modified BIC technique are also feasible and safe with many benefits, as we described in our report.
| 1. | European Association for the Study of the Liver (EASL). EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016;65:146-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 372] [Article Influence: 37.2] [Reference Citation Analysis (2)] |
| 2. | Park CH. The Management of Common Bile Duct Stones. Korean J Gastroenterol. 2018;71:260-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Zhang J, Ling X. Risk factors and management of primary choledocholithiasis: a systematic review. ANZ J Surg. 2021;91:530-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Pan L, Chen M, Ji L, Zheng L, Yan P, Fang J, Zhang B, Cai X. The Safety and Efficacy of Laparoscopic Common Bile Duct Exploration Combined with Cholecystectomy for the Management of Cholecysto-choledocholithiasis: An Up-to-date Meta-analysis. Ann Surg. 2018;268:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 123] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 5. | Parra-Membrives P, Martínez-Baena D, Lorente-Herce J, Jiménez-Riera G. Comparative Study of Three Bile Duct Closure Methods Following Laparoscopic Common Bile Duct Exploration for Choledocholithiasis. J Laparoendosc Adv Surg Tech A. 2018;28:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Morton A, Cralley A, Brooke-Sanchez M, Pieracci FM. Laparoscopic common bile duct exploration by acute care surgeons saves time and money compared to ERCP. Am J Surg. 2022;224:116-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 7. | Eitler K, Bibok A, Telkes G. Situs Inversus Totalis: A Clinical Review. Int J Gen Med. 2022;15:2437-2449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 120] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 8. | Liu Y, Wu L, Chen Y, Li D, Jiang J, Zhong W, Cao Y. Delayed diagnosis of abdominal pain in patient with situs inversus totalis in emergency department: A case report. Medicine (Baltimore). 2017;96:e9028. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 9. | Enciu O, Toma EA, Tulin A, Georgescu DE, Miron A. Look beyond the Mirror: Laparoscopic Cholecystectomy in Situs Inversus Totalis-A Systematic Review and Meta-Analysis (and Report of New Technique). Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Chaouch MA, Jerraya H, Dougaz MW, Nouira R, Dziri C. A Systematic Review of Laparoscopic Cholecystectomy in Situs Inversus. J Invest Surg. 2021;34:324-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Wong J, Tang CN, Chau CH, Luk YW, Li MK. Laparoscopic cholecystectomy and exploration of common bile duct in a patient with situs inversus. Surg Endosc. 2001;15:218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 12. | Tang CN, Tsui KK, Ha JP, Siu WT, Li MK. Laparoscopic exploration of the common bile duct: 10-year experience of 174 patients from a single centre. Hong Kong Med J. 2006;12:191-196. [PubMed] |
| 13. | Emmanuel J, Sriram N, Muthukaruppan R. Endoscopic retrograde cholangiopancreatography in a patient with complete situs inversus viscerum: A case report and literature review. DEN Open. 2022;2:e17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 14. | Alzahrani HA, Yamani NM. Gallbladder agenesis with a primary choledochal stone in a patient with situs inversus totalis. Am J Case Rep. 2014;15:185-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Weber-Sánchez A, Bravo-Torreblanca C, Garteiz-Martínez D, Carbó-Romano R, Vega-Rivera F, Hernández R. Case report: laparoscopic cholecystectomy and common bile duct exploration in a 60 year-old patient with situs inversus. Rev Gastroenterol Mex. 2011;76:255-259. [PubMed] |
| 16. | Han SJ, Chun KS, Song IS. Laparoscopic cbd exploration in patient with situs inversus totalis. HPB. 2012;14:328. [DOI] [Full Text] |
| 17. | Senthilnathan P, Parthasarathi R, Rajapandian S, Praveen Raj P, Vijai A, Nalankilli VP, Srivatsan G, Sabnis S, Palanivelu C. Laparoscopic CBD exploration with choledochoduodenostomy for bileduct stones in a patient with situs inversus totalis. Surgical Endoscopy and Other Interventional Techniques. 2017;31:S95. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Simkhada S, Malla B, Shrestha R. Laparoscopic Cholecystectomy and Common Bile Duct Exploration in Situs Inversus Patients. Kathmandu Univ Med J (KUMJ). 2021;19:271-274. [PubMed] |
| 19. | Takalkar YP, Koranne MS, Vashist KS, Khedekar PG, Garale MN, Rege SA, Dalvi AN. Laparoscopic cholecystectomy with choledochoduodenostomy in a patient with situs inversus totalis. J Minim Access Surg. 2018;14:241-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Tai CK, Tang CN, Ha JP, Chau CH, Siu WT, Li MK. Laparoscopic exploration of common bile duct in difficult choledocholithiasis. Surg Endosc. 2004;18:910-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Kang SB, Han HS. Laparoscopic exploration of the common bile duct in a patient with situs inversus totalis. J Laparoendosc Adv Surg Tech A. 2004;14:103-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Chuang SH, Hung MC, Huang SW, Chou DA, Wu HS. Single-incision laparoscopic common bile duct exploration in 101 consecutive patients: choledochotomy, transcystic, and transfistulous approaches. Surg Endosc. 2018;32:485-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Chuang SH, Chen PH, Chang CM, Tsai YF, Lin CS. Single-incision laparoscopic common bile duct exploration with conventional instruments: an innovative technique and a comparative study. J Gastrointest Surg. 2014;18:737-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Qandeel H, Zino S, Hanif Z, Nassar MK, Nassar AH. Basket-in-catheter access for transcystic laparoscopic bile duct exploration: technique and results. Surg Endosc. 2016;30:1958-1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Soofi M, Alpert MA, Barbadora J, Mukerji B, Mukerji V. Human Laterality Disorders: Pathogenesis, Clinical Manifestations, Diagnosis, and Management. Am J Med Sci. 2021;362:233-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Zurcher K, Kawashima A. Kartagener's Syndrome. N Engl J Med. 2021;384:e45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Wallmeier J, Nielsen KG, Kuehni CE, Lucas JS, Leigh MW, Zariwala MA, Omran H. Motile ciliopathies. Nat Rev Dis Primers. 2020;6:77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 260] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 28. | Lucas JS, Davis SD, Omran H, Shoemark A. Primary ciliary dyskinesia in the genomics age. Lancet Respir Med. 2020;8:202-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 224] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 29. | Chen W, Guo Z, Qian L, Wang L. Comorbidities in situs inversus totalis: A hospital-based study. Birth Defects Res. 2020;112:418-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 30. | Masiwal P, Chenthil KS, Priyadarsini B, Gnanaprakasam J, Srihari I. Ivemark Syndrome. J Assoc Physicians India. 2016;64:73-75. [PubMed] |
| 31. | Nair R, Muthukuru SR. Dextrocardia. 2022 Sep 19. In: StatPearls [Internet]. StatPearls Publishing. 2022 Jan. [PubMed] |
| 32. | Munshi FI, Polotti CF, Elsamra SE. Robot-Assisted Radical Cystectomy with Intracorporeal Ileal Conduit in a Patient with Situs Inversus Totalis. J Endourol Case Rep. 2020;6:135-138. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 33. | Miheţiu AF, Bratu DG, Popescu OM, Juravle C, Dumitrean IE, Chicea R. A rare case of situs inversus totalis associated with sigmoid diverticulitis and appendicular agenesis. Embryological, clinical considerations and literature review. Rom J Morphol Embryol. 2021;62:861-867. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 34. | Di Buono G, Maienza E, Buscemi S, Randisi B, Romano G, Agrusa A. Acute appendicitis in a patient with situs viscerum inversus totalis: Role of laparoscopic approach. A case report and brief literature review. Int J Surg Case Rep. 2020;77S:S29-S33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Herrera Ortiz AF, Lacouture JC, Sandoval Medina D, Gómez Meléndez LJ, Uscategui R. Acute Cholecystitis in a Patient With Situs Inversus Totalis: An Unexpected Finding. Cureus. 2021;13:e15799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Evola G, Ferrara F, Di Fede GF, Patanè M, Sarvà S, Piazza L. Left-sided acute appendicitis in a patient with situs viscerum inversus totalis: A case report. Int J Surg Case Rep. 2022;90:106658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 37. | Umar UA, Alremeithi AN, Qayyum H. Incidental diagnosis of situs inversus totalis: a perspective from an emergency department attendance. BMJ Case Rep. 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 38. | Abbey E, Yang F, Qi L, Wu JJ, Tong L, Zhen Z. Situs inversus totalis patients with gastric cancer: Robotic surgery the standard of treatment? Int J Surg Case Rep. 2021;81:105818. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 39. | Kasai S, Hino H, Shiomi A, Kagawa H, Manabe S, Yamaoka Y, Kato S, Hanaoka M, Kinugasa Y. Robotic-assisted surgery for rectal cancer with situs inversus totalis: A case report. Asian J Endosc Surg. 2021;14:803-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 40. | Li X, Liu Z, Kong R, Zhang C, Ge S. Robot-assisted beating-heart surgery for atrial septal defect repair in a case of situs inversus totalis with dextrocardia. Int J Med Robot. 2021;17:e2304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 41. | Yeom SS, Kim KH, Lee SY, Kim CH, Kim HR, Kim YJ. Reduced-Port Laparoscopic Surgery for Patients With Proximal Transverse Colon Cancer With Situs Inversus Totalis: A Case Report. Ann Coloproctol. 2018;34:322-325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 42. | Jomaa S, Deeb H, Alshaar D, Alahmar FO. Surgical challenges during open pancreaticoduodenectomy in a patient with situs inversus totalis: A rare case report and literature review. Ann Med Surg (Lond). 2022;82:104610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 43. | Hu L, Chai Y, Yang X, Wu Z, Sun H, Wang Z. Duodenoscope combined with laparoscopy in treatment of biliary stones for a patient with situs inversus totalis: A case report. Medicine (Baltimore). 2019;98:e14272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 44. | de la Serna-Higuera C, Perez-Miranda M, Flores-Cruz G, Gil-Simón P, Caro-Patón A. Endoscopic retrograde cholangiopancreatography in situs inversus partialis. Endoscopy. 2010;42 Suppl 2:E98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 45. | Yoshida A, Minaga K, Takeda O, Hanno H, Takayanagi S, Dozaiku T, Kudo M. Successful biliary cannulation using a novel rotatable sphincterotome in a patient with situs inversus totalis. Endoscopy. 2020;52:E333-E334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 46. | Tanisaka Y, Ryozawa S, Sudo K, Fujita A, Mizuide M, Nonaka K, Tashima T. Successful endoscopic retrograde cholangiopancreatography using pancreatic guidewire placement for biliary cannulation in a patient with situs inversus and Billroth-I gastrectomy (with video). JGH Open. 2019;3:540-541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 47. | Shimoda F, Satoh A, Asonuma S, Umemura K, Shimosegawa T. Successful removal of multiple bile duct stones using a papillary large balloon dilation in a very elderly woman with situs inversus totalis. Clin J Gastroenterol. 2021;14:309-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 48. | Ding B, Wang J, Wei X, Du Y, Xia L, Sun C, Han K, Yang X, Guo X, Pan Y, Wang X. Efficacy and safety of ERCP in patients with situs inversus totalis: multicenter case series and literature review. BMC Gastroenterol. 2022;22:497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 49. | Gao YK, Liu SH, Xie SA, Wen HP, Cao LQ. Successful endoscopic drainage of malignant obstructive jaundice in patients with situs inversus totalis: Two cases report. Int J Surg Case Rep. 2022;93:106873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 50. | Naser J, Sarmini MT, Vozzo C, Saleh MA, Chahal P. ERCP and EUS technique in situs inversus totalis: preparing for a left-sided plot twist. VideoGIE. 2022;7:367-370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 51. | Oh CH. Successful endoscopic retrograde cholangiopancreatography and bilateral stenting in a patient with situs inversus totalis. Dig Liver Dis. 2022;54:136-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 52. | Valdivielso Cortázar E, Porto Fuentes Ó, González Peñas L, Couto Wörner I, Souto Ruzo J, González Conde B, Estévez Prieto E, Alonso Aguirre P. ERCP and situs inversus. Rev Esp Enferm Dig. 2022;114:176-177. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 53. | Atwez A, Keilani Z. Laparoscopic Roux-en-Y gastric bypass in a patient with situs inversus totalis: Case report, technical tips and review of the literature. Int J Surg Case Rep. 2018;45:56-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 54. | Sagawa H, Ito S, Hayakawa S, Ueno S, Okubo T, Tanaka T, Ogawa R, Takahashi H, Matsuo Y, Mitsui A, Kimura M, Takiguchi S. Robotic distal gastrectomy for gastric cancer in a patient with situs inversus totalis and a vascular anomaly. Int Cancer Conf J. 2022;11:253-260. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 55. | Zavalza JF, Molina GA, Paipilla OA, Gil M, Rosales K. Situs inversus and bariatric surgery: A challenge for the surgical team. Ann Med Surg (Lond). 2021;72:102972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 56. | Patle NM, Tantia O, Sasmal PK, Khanna S, Sen B. Laparoscopic cholecystectomy in situs inversus-our experience of 6 cases. Indian J Surg. 2010;72:391-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 57. | García-Núñez LM, Soto-Ortega LE, Payró-Hernández LE, Cabello-Pasini R. Laparoscopic cholecystectomy in situs inversus: the disadvantage of being right-handed. Rev Gastroenterol Mex. 2008;73:149-152. [PubMed] |
| 58. | Tchantchaleishvili V, Myers PO. Left-handedness--a handicap for training in surgery? J Surg Educ. 2010;67:233-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 59. | Prasad NK, Kvasnovsky C, Wise ES, Kavic SM. The Right Way to Teach Left-Handed Residents: Strategies for Training by Right Handers. J Surg Educ. 2018;75:271-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 60. | Chuang SH, Kuo KK, Chuang SC, Wang SN, Chang WT, Su WL, Huang JW, Wu PH, Chan HM, Kuok CH. Single-incision versus four-incision laparoscopic transfistulous bile duct exploration for Mirizzi syndrome type II. Surg Endosc. 2022;36:8672-8683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Chuang SH, Yang WJ, Chang CM, Lin CS, Yeh MC. Is routine single-incision laparoscopic cholecystectomy feasible? Am J Surg. 2015;210:315-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 62. | Khiangte E, Newme I, Patowary K, Phukan P. Single-port laparoscopic cholecystectomy in situs inversus totalis using the E.K. glove port. J Minim Access Surg. 2013;9:180-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 63. | Deguchi Y, Mitamura K, Omotaka S, Eguchi J, Sakuma D, Sato M, Nomura N, Ito T, Grimes KL, Inoue H. Single-incision cholecystectomy in a patient with situs inversus totalis presenting with cholelithiasis: A case report. Asian J Endosc Surg. 2015;8:347-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 64. | Jhobta RS, Gupta A, Negi B, Negi K. Single-incision laparoscopic cholecystectomy using conventional instruments in situs inversus totalis. BMJ Case Rep. 2018;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 65. | Jang EJ, Roh YH. Single Port Laparoscopic Cholecystectomy in a Patient with Situs Inversus Totalis: A Case Report. J Minim Invasive Surg. 2019;22:81-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 66. | Chuang SH, Lin CS. Single-incision laparoscopic surgery for biliary tract disease. World J Gastroenterol. 2016;22:736-747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (5)] |
| 67. | Gupta N. Role of laparoscopic common bile duct exploration in the management of choledocholithiasis. World J Gastrointest Surg. 2016;8:376-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 68. | Zerey M, Haggerty S, Richardson W, Santos B, Fanelli R, Brunt LM, Stefanidis D. Laparoscopic common bile duct exploration. Surg Endosc. 2018;32:2603-2612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 69. | Navaratne L, Martinez Isla A. Transductal versus transcystic laparoscopic common bile duct exploration: an institutional review of over four hundred cases. Surg Endosc. 2021;35:437-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 70. | Bekheit M, Smith R, Ramsay G, Soggiu F, Ghazanfar M, Ahmed I. Meta-analysis of laparoscopic transcystic versus transcholedochal common bile duct exploration for choledocholithiasis. BJS Open. 2019;3:242-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 71. | Feng Q, Huang Y, Wang K, Yuan R, Xiong X, Wu L. Laparoscopic Transcystic Common Bile Duct Exploration: Advantages over Laparoscopic Choledochotomy. PLoS One. 2016;11:e0162885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 72. | Guan H, Jiang G, Mao X. Primary duct closure combined with transcystic drainage versus T-tube drainage after laparoscopic choledochotomy. ANZ J Surg. 2019;89:885-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Atqiaee K, Iran; Miao G, China S-Editor: Li L L-Editor: A P-Editor: Li L