Published online Mar 16, 2023. doi: 10.12998/wjcc.v11.i8.1808
Peer-review started: November 18, 2022
First decision: December 26, 2022
Revised: January 4, 2023
Accepted: February 16, 2023
Article in press: February 16, 2023
Published online: March 16, 2023
Processing time: 109 Days and 6.4 Hours
A giant juvenile fibroadenoma (GJF) is a rare, benign breast tumor that affects females < 18 years of age. GJFs are generally suspected based on a palpable mass. GJFs influence breast shape and mammary gland development via the pressure effect from their enormous size.
Herein we report a case involving a 14-year-old Chinese female with a GJF in the left breast. GJF is a rare, benign breast tumor that usually occurs between 9 and 18 years of age and accounts for 0.5%-4.0% of all fibroadenomas. In severe cases, breast deformation may occur. This disease is rarely reported in Chinese people and has a high clinical misdiagnosis rate due to the absence of specific imaging features. On July 25, 2022, a patient with a GJF was admitted to the First Affiliated Hospital of Dali University. The preoperative clinical examination and conventional ultrasound diagnosis needed further clarification. The mass was shown to be an atypical lobulated mass during the operation and confirmed to be a GJF based on pathologic examination.
GJF is also a rare, benign breast tumor in Chinese women. Evaluation of such masses consists of a physical examination, radiography, ultrasonography, computer tomography, and magnetic resonance imaging. GJFs are confirmed by histopathologic examination. Mastectomy is not selected when the patient benefits from a complete resection of the mass with breast reconstruction and an uneventful recovery.
Core Tip: Giant juvenile fibroadenoma (GJF) is a rare benign breast tumor below 18 years of age and can be suspected mainly through palpable masses in clinical practice. Breast ultrasonography shows left masses > 5 cm with benign features (Breast Imaging Reporting and Data System score 3) through the preferred examination for breast imaging in this GJF case. The breast mass of GJF patients in this report showed a lobulated shape and many lobular ducts. Therefore, it is necessary to differentiate GJF from phosphotyrosine binding by histopathology. Clinicians should be aware of this diagnosis for a better approach and early conservative treatment instead of blindly performing mastectomy.
- Citation: Wang J, Zhang DD, Cheng JM, Chen HY, Yang RJ. Giant juvenile fibroadenoma in a 14-year old Chinese female: A case report. World J Clin Cases 2023; 11(8): 1808-1813
- URL: https://www.wjgnet.com/2307-8960/full/v11/i8/1808.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i8.1808
A fibroadenoma (FA) is characterized by aberrant proliferation of epithelial and mesenchymal elements, and is the most common benign lesion of the breast in females < 30 years of age[1]. FAs are mostly solitary and can be unilateral or bilateral, with 10%-20% occurring in multiple fashions[1] and divided into adult- and juvenile-types[1,2]. A giant fibroadenoma (GFA) is a specific type of FA that weighs > 500 g, measures > 50 mm in diameter, or is disproportionally large compared with the rest of the breast[2]. The exact etiology of GFA is unknown[2]; however, unopposed estrogen stimulation, increased estrogen receptor sensitivity, or diminished estrogen antagonist sensitivity are thought to be the chief causative factors[1]. FAs are commonly detected incidentally during routine physical examination, ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT), and are diagnosed based on pathologic evaluation. Gene detection and artificial intelligence have been shown to have high prediction accuracy, sensitivity, and specificity in the differential diagnosis of large breast masses[3,4].
On July 25, 2022, a 14-year-old girl was hospitalized in the Department of Thyroid and Breast Surgery of the First Affiliated Hospital of Dali University (China), for evaluation of a giant left breast mass, which had been developing for nearly 6 mo without an apparent cause. Indeed, the mass had enlarged from the initial size of a mung bean to the current size of a hen’s egg.
The patient had normal menstruation in the past. She denied any family history of breast masses.
The patient had no history of any other illness.
The patient denied any history of chest disease, irradiation or estrogen supplementation. There was no family history of breast or ovarian cancer.
The physical examination revealed a 100.0 mm × 40.0 mm mass on the left breast with an unclear border, tough texture, poor mobility, and tenderness. There was no skin erythema, surgical scars, or nipple depression involving the affected breast. The right breast and both axillae were normal. In addition, there were no abnormalities on the biological examination.
There were no abnormalities on routine blood testing, blood biochemistry, blood coagulation function, or routine stool and urine testing.
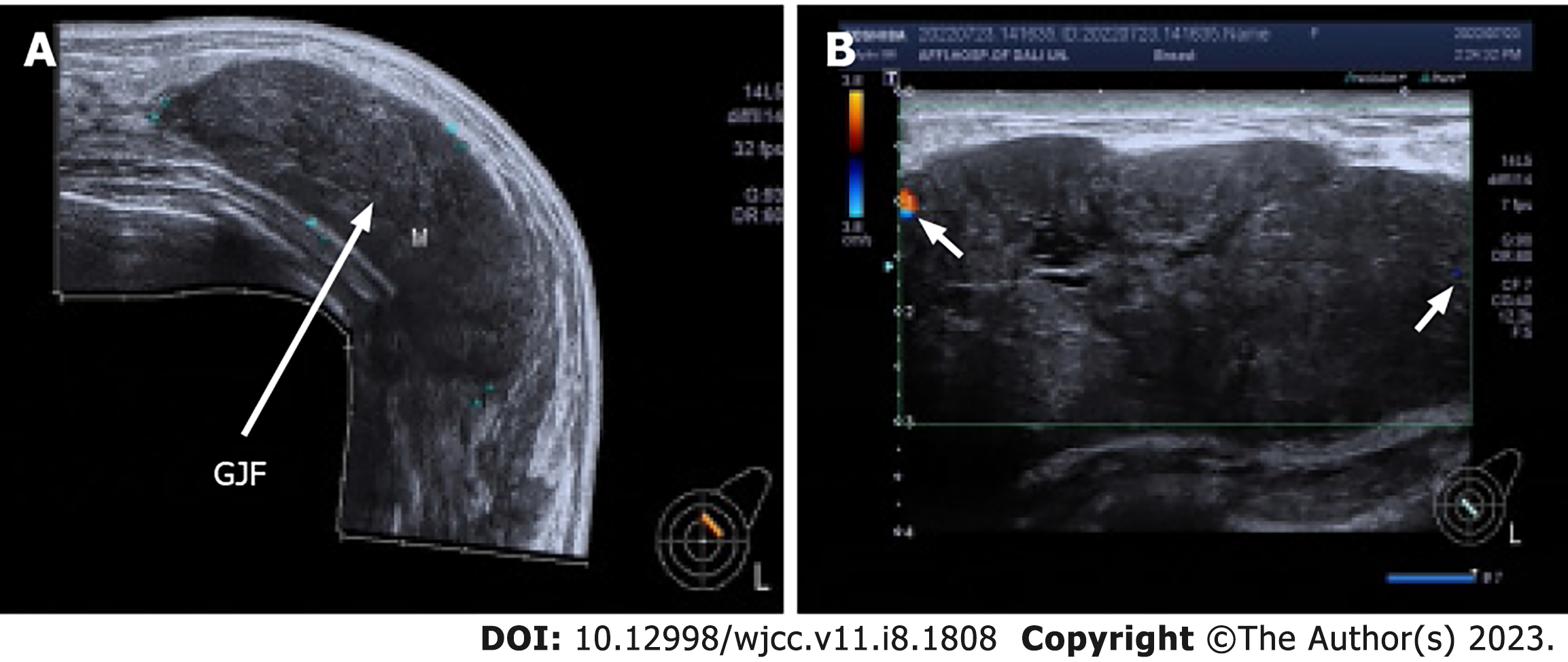
Breast ultrasonography (BUSG) (Toshiba Aplio 500© with a 7.5-MHz probe) of the patient’s left breast showed a large hypoechoic solid lesion (110.4 mm × 41.6 mm in size), which had an oval shape, clear boundaries, horizontal growth, and even distribution. A few irregular liquid dark areas were noted in the breast mass without obvious calcifications and no enlarged lymph nodes in the bilateral axillae (Figure 1A). A color Doppler examination revealed few punctate flow signals at the edge of the breast mass (Figure 1B). The lesion was classified as Breast Imaging Reporting and Data System (BI-RADS) category 3.
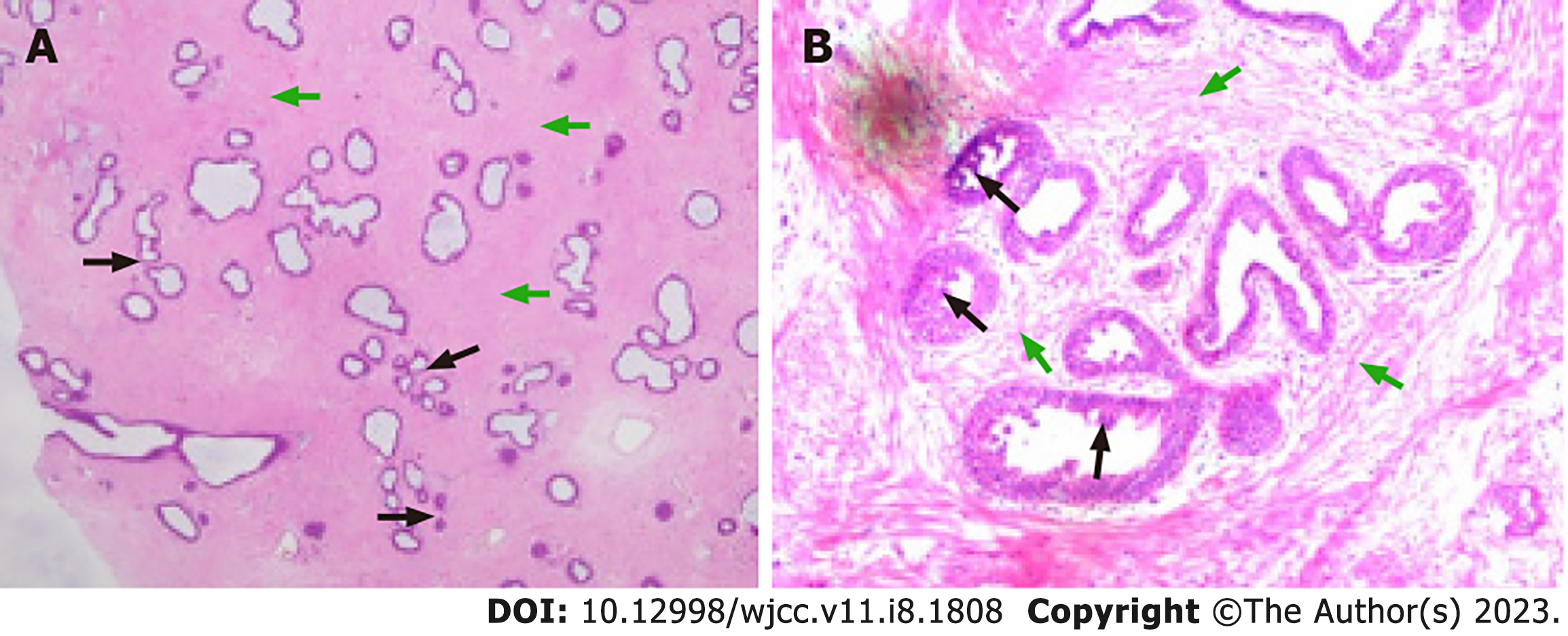
A tru-cut biopsy of frozen sections was reported as a juvenile fibroadenoma (JFA), which was characterized by small oval gland ducts and interstitial collagen fibers (Figure 2).
A GJF is mainly differentiated from phyllodes tumor of the breast (PTB). A PTB is considered a rare fibroepithelial neoplasm of the breast that can be detected in all ages; however, the median age of presentation is 45 years[5]. PTB constitutes around 1% of all FAs and 2.5% of fibroepithelial breast lumps[6]. The World Health Organization (WHO) has classified PTBs histologically as benign, borderline, and malignant[5,6]. The benign variant of a PTB is the most common and close resembles an FA, but is usually larger and recurs more frequently; the rare malignant type is aggressive[6]. The clinical symptoms of a PTB include rapidly growing breast masses; imaging features resemble GFAs or JFAs with benign features[7]. Therefore, a histopathologic examination is the best way to distinguish a GJF from a PTB.
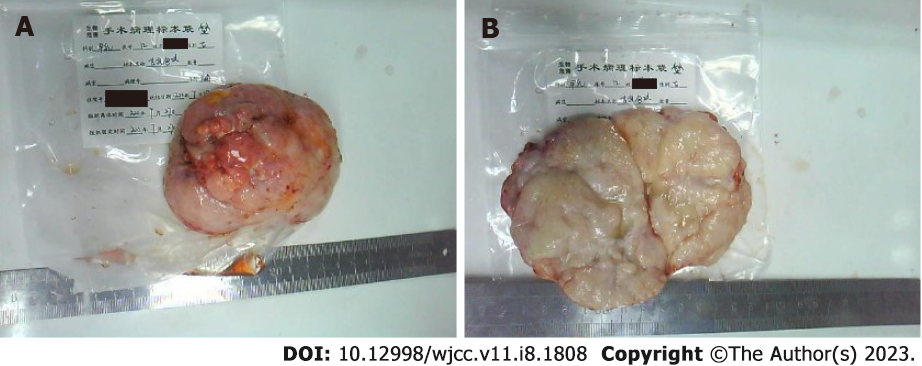
On July 27, 2022, the patient successfully underwent a simple surgical excision under general anesthesia. The excised lump was smooth, mobile, lobulated, and 100 mm × 90 mm × 50 mm in size (Figure 3). Because she benefited from a complete resection of the mass with breast reconstruction and recovered uneventfully, a mastectomy was not indicated.
The breast development of the patient was restored to normal. Three months after surgery, her routine outpatient follow-up BUSG evaluation was normal.
FAs are the most common benign tumors in adolescent women. FAs commonly present in late adolescence and comprise 91% of all histologically-evaluated solid breast masses among patients < 19 years of age based on a radiologic study[8]. Among women with FAs, only 15% have 2-4 masses in one breast, and only 11% have bilateral masses[9]. According to the size and histologic features, adolescent breast masses usually include six types: Simple, complex, multiple, giant, juvenile FAs, and phosphotyrosine binding[7,10,11]. While simple FAs of the breast are the most common lesion, giant juvenile fibroadenomas (GJFs) are a very rare variant with an incidence of 0.5%-2.0%, representing 7%-8% of all FA subtypes, and the most common cause of unilateral gigantomastia in young female patients[7]. In fact, GFAs in patients between 10 and 18 years of age are defined as JFAs, eventually becoming GFAs due to rapid growth[12].
Fibroepithelial breast tumors are biphasic neoplasms formed by an organoid pattern of ductal structures with a striking stromal appearance composed of extensive vascular proliferation, including common FAs and rare phyllodes tumors[13,14]. The FA stroma is usually of low cellularity, with myxoid, fibroblastic, or hyalinized appearances, displaying an interlacing fascicular arrangement of fibroblasts and myofibroblasts with a peri-canalicular pattern[8]. The epithelial proliferation may disclose gynecomastia features with fine filigree-like narrow micropapillary epithelial protrusions[8]. Phyllodes tumors, neoplasms with the potential for recurrence, show an exaggerated intracanalicular growth pattern with broad stromal fronded architecture and stromal hypercellularity[13]. Although the breast mass of the patient in this report had a lobulated shape and a large number of lobular ducts, the histopathologic report was not a phyllodes tumor, thus more longitudinal follow-up is required.
Imaging plays an important role in diagnosing and differentiating GJFs, and a histopathologic exam is used to define the diagnosis further. In a retrospective analysis of 52 articles (n = 153 patients), most patients (86%) presented with a single breast mass[15]. Imaging modalities included BUSG in 72.5% of the patients and mammography (MMG) in 26.1% of the patients[15]. A tissue diagnosis was obtained using a core-needle biopsy in 18.3% of the patients, fine-needle aspiration (FNA) in 25.5% of the patients, and excisional biopsy in 11.1% of the patients[15]. BUSG and MMG are two basic techniques for routine imaging in diagnosing breast diseases, such as FAs, phyllodes tumors, hamartomas, cysts, hematomas, abscesses, and carcinomas, which are difficult to distinguish clinically based on interview, clinical manifestations, and physical examination. The accuracy of MMG is reduced because of the high density of glandular tissue in adolescent breasts[16], thus MMG is not recommended[7]. If it is not feasible to establish the diagnosis of a JFA clinically, further studies are necessary (BUSG and FNA)[16]. BUSG is the main diagnostic examination in children and adolescents associated with a breast MRI[7]. The 7.5-MHz probe used in this study is commonly recommended in classic textbooks. Sonographic imaging of the breasts with a 7.5-MHz probe achieved a sensitivity of 83% and an net present value of 84%. The same concept applies to Doppler scanning[17]. A high-frequency (20-30 MHz) probe was used in a targeted manner to image breasts in prospective studies. High-quality scans were obtained with optimal spatial resolution and anatomic detail[17]. The typical appearance of a GJF on BUSG is the presence of well-circumscribed round or oval-shaped masses, sometimes lobulated, with a parallel orientation, fairly uniform hypoechoic or anechoic areas with low-level internal echoes, and sometimes with a posterior acoustic enhancement[7]. A GJF on Doppler evaluation can be avascular or show some central vascularity[7]. The diagnosis and treatment of GJFs are heterogeneous. The most common diagnostic modalities include a core needle or excisional biopsy, and the mainstay of treatment is complete excision with an emphasis on preserving the developing breast parenchyma and nipple-areolar complex[15]. Women with BI-RADS category 3 or less breast lesions have a low risk of malignancy, in which case an FNA would reduce the excisional biopsy rate[18]. In the treatment of our patient, although the mass was removed directly without an FNA, it was confirmed by BUSG and verified by pathologic evaluation.
GJFs are benign tumors that can influence breast shape and mammary gland development through a pressure effect due to the enormous size of the mass. GJFs usually require surgical resection of the mass to offer a complete cure and acceptable cosmetic results. In this case report, the breast ultrasound provided a preoperative diagnostic basis for surgical treatment, while the postoperative histopathologic diagnosis avoided an unnecessary mastectomy.
We thank all clinicians who provided pictures and laboratory results.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corvino A, Italy; Jamali R, Iran S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Zeeshan S, Shaikh K, Tariq MU, Vohra LM. Giant Juvenile Fibroadenoma of the breast in a 13-year-old Pakistani girl with excellent cosmetic outcome after subareolar enucleation - A case report. Int J Surg Case Rep. 2021;79:450-454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 2. | Islam S, Saroop S, Bheem V, Naraynsingh V. Largest giant juvenile fibroadenoma of the breast. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Yin Lee JP, Thomas AJ, Lum SK, Shamsudin NH, Hii LW, Mai CW, Wong SF, Leong CO. Gene expression profiling of giant fibroadenomas of the breast. Surg Oncol. 2021;37:101536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Niu S, Huang J, Li J, Liu X, Wang D, Wang Y, Shen H, Qi M, Xiao Y, Guan M, Li D, Liu F, Wang X, Xiong Y, Gao S, Yu P, Zhu J. Differential diagnosis between small breast phyllodes tumors and fibroadenomas using artificial intelligence and ultrasound data. Quant Imaging Med Surg. 2021;11:2052-2061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Rayzah M. Phyllodes Tumors of the Breast: A Literature Review. Cureus. 2020;12:e10288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Alipour S, Eskandari A. Phyllodes Tumor of the Breast in Pregnancy and Lactation. Adv Exp Med Biol. 2020;1252:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 7. | Belkouchi L, El Haddad S, Mrani Alaoui N, Allali N, Chat L. Child gigantomastia revealing juvenile giant fibroadenomas. BJR Case Rep. 2022;8:20210181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Tan PH. Fibroepithelial lesions revisited: implications for diagnosis and management. Mod Pathol. 2021;34:15-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 9. | Im CJ, Miller A, Balassanian R, Mukhtar RA. Early onset, multiple, bilateral fibroadenomas of the breast: a case report. BMC Womens Health. 2021;21:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Jayasinghe Y, Simmons PS. Fibroadenomas in adolescence. Curr Opin Obstet Gynecol. 2009;21:402-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Panda SK, Patro B, Mishra J, Dora RK, Subudhi BS. Multiple fibroadenomas in bilateral breasts of a 46-year-old Indian woman - A case report. Int J Surg Case Rep. 2014;5:262-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Basara Akin I, Balci P. Fibroadenomas: a multidisciplinary review of the variants. Clin Imaging. 2021;71:83-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Lerwill MF, Lee AHS, Tan PH. Fibroepithelial tumours of the breast-a review. Virchows Arch. 2022;480:45-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Hanna W, AL-Maghrabi J, Malik A. Aggressive giant fibroepithelial lesion with unusual vascular stroma--a case report. Mod Pathol. 2003;16:823-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 15. | Sosin M, Pulcrano M, Feldman ED, Patel KM, Nahabedian MY, Weissler JM, Rodriguez ED. Giant juvenile fibroadenoma: a systematic review with diagnostic and treatment recommendations. Gland Surg. 2015;4:312-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 16. | Mareti E, Vatopoulou A, Spyropoulou GA, Papanastasiou A, Pratilas GC, Liberis A, Hatzipantelis E, Dinas K. Breast Disorders in Adolescence: A Review of the Literature. Breast Care (Basel). 2021;16:149-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 17. | Corvino A, Varelli C, Catalano F, Cocco G, Delli Pizzi A, Boccatonda A, Corvino F, Basile L, Catalano O. Use of High-Frequency Transducers in Breast Sonography. J Pers Med. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 18. | Chen Z, Salibay C, Elatre W, Naritoku WY, Ma Y, Martin SE, Wang T. Performance of breast fine needle aspiration as an initial diagnostic tool: A large academic hospital experience. Cytopathology. 2022;33:707-715. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |