Published online Mar 16, 2023. doi: 10.12998/wjcc.v11.i8.1794
Peer-review started: November 1, 2022
First decision: December 19, 2022
Revised: January 7, 2023
Accepted: February 15, 2023
Article in press: February 15, 2023
Published online: March 16, 2023
Processing time: 125 Days and 19.8 Hours
Testicular pain caused by lumbar disease is uncommon in the clinic. Here we reported a case of discogenic low back pain with testicular pain that was successfully cured.
A 23-year-old male patient presented to our department with chronic low back pain. Based on his clinical symptoms, signs and imaging, he was diagnosed with discogenic low back pain. Since conservative treatment for more than half a year did not significantly improve his low back pain, we decided to treat it with intradiscal methylene blue injection. During the course of surgery, we again identified the low back pain as originating from the degenerated lumbar disc by analgesic discography. Interestingly, the patient’s low back pain disappeared along with the testicular pain that had been present for more than 3 mo. After the operation, the patient’s low back pain improved, and the testicular pain did not reappear.
Intradiscal methylene blue injection is a convenient and effective surgical intervention for the treatment of discogenic low back pain. Lumbar disc degeneration may also be a possible clinical cause of testicular pain. Methylene blue injection in the diseased disc improved the low back pain, and the accom
Core Tip: Herein, we present a case of a patient who was cured of testicular pain after treatment of discogenic low back pain. Lumbar disc degeneration may be a possible etiology of testicular pain.
- Citation: Yan XJ, Wu B, He X, Tian ZK, Peng BG. Testicular pain originating from lumbar disc degeneration: A case report. World J Clin Cases 2023; 11(8): 1794-1798
- URL: https://www.wjgnet.com/2307-8960/full/v11/i8/1794.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i8.1794
Chronic testicular pain is a common symptom in urology[1]. Clinicians have found numerous causes that can evoke testicular pain, including infections, tumors, varicocele and referred pain. However, many patients still suffer from testicular pain of unknown pathogenesis that cannot be effectively treated[2]. Lumbar disc degeneration has been proven to be a major source of low back pain, and some researchers have proposed that lumbar disc herniation could also lead to testicular pain[3]. Nevertheless, there has been no high-quality study on testicular pain caused by lumbar disc degeneration. The relationship between lumbar disc degeneration and testicular pain or the pathogenesis of discogenic testicular pain remains elusive. In this paper, we reported a young male whose testicular pain was cured after treating discogenic low back pain and analyzed the possible pathogenesis of testicular pain induced by lumbar disc degeneration.
A 23-year-old man had a 1-year history of severe low back pain, which seriously affected his quality of life.
Prior to presenting at our department, the patient had been on nonsteroidal anti-inflammatory drugs and physical therapy for more than 8 mo. However, the low back pain did not improve and instead continued to worsen.
The patient had also suffered from bilateral testicular pain for more than 3 mo. After detailed physical examination and related ultrasonography, the urologists hypothesized that the testicular pain was not caused by a urinary system disease. No other illnesses were documented, and the patient had no relevant traumatic history.
It was unremarkable.
The pressure pain of L4/5 intervertebral space was positive. No abnormal sensory or motor function of either lower extremity. The scrotum was normal, and the testicles were in the scrotum without enlargement. The right testis was slightly tender. Visual analogue scale (VAS) score of low back pain was 8 and the testicular pain was 7.
It was unremarkable.
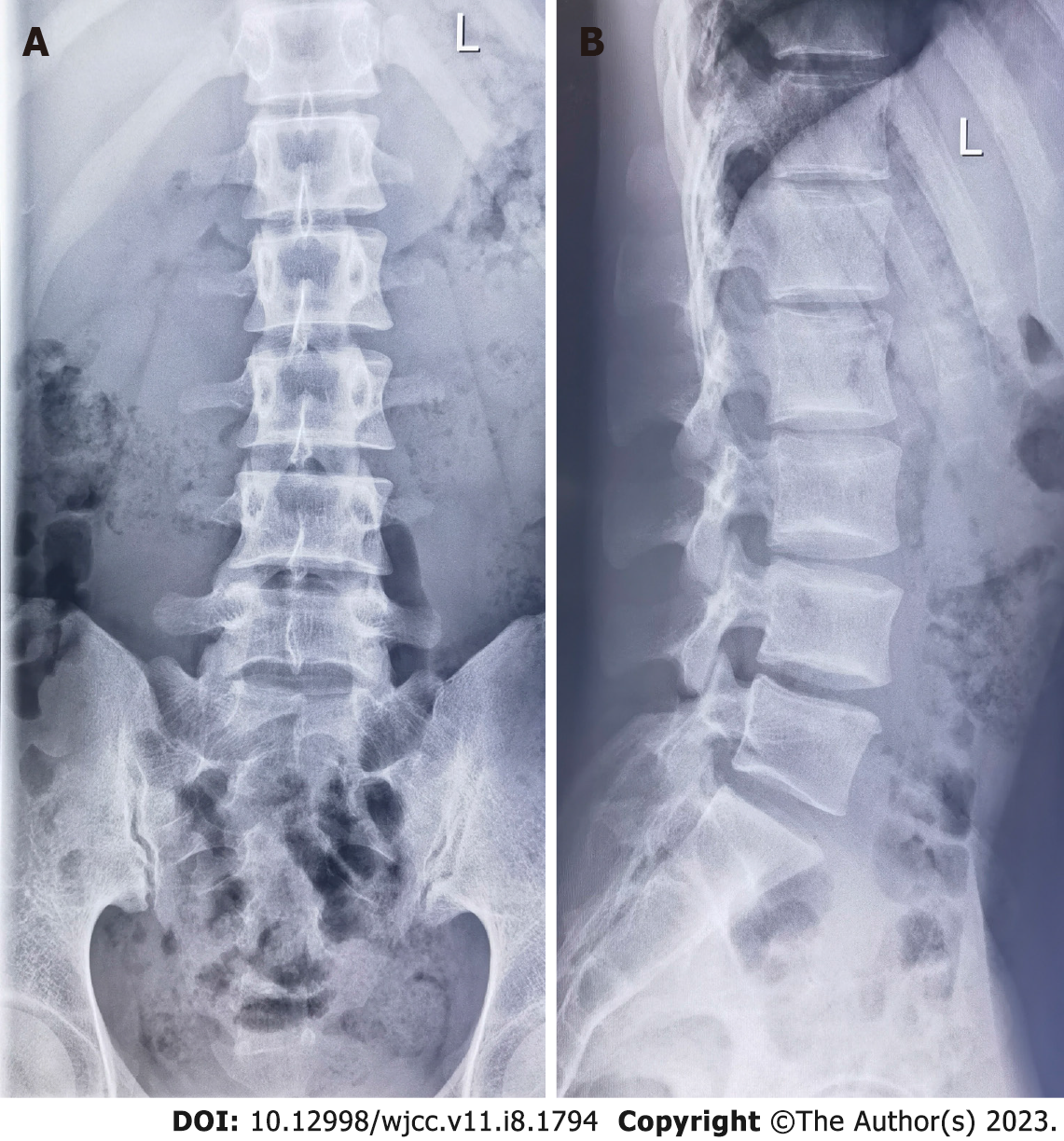
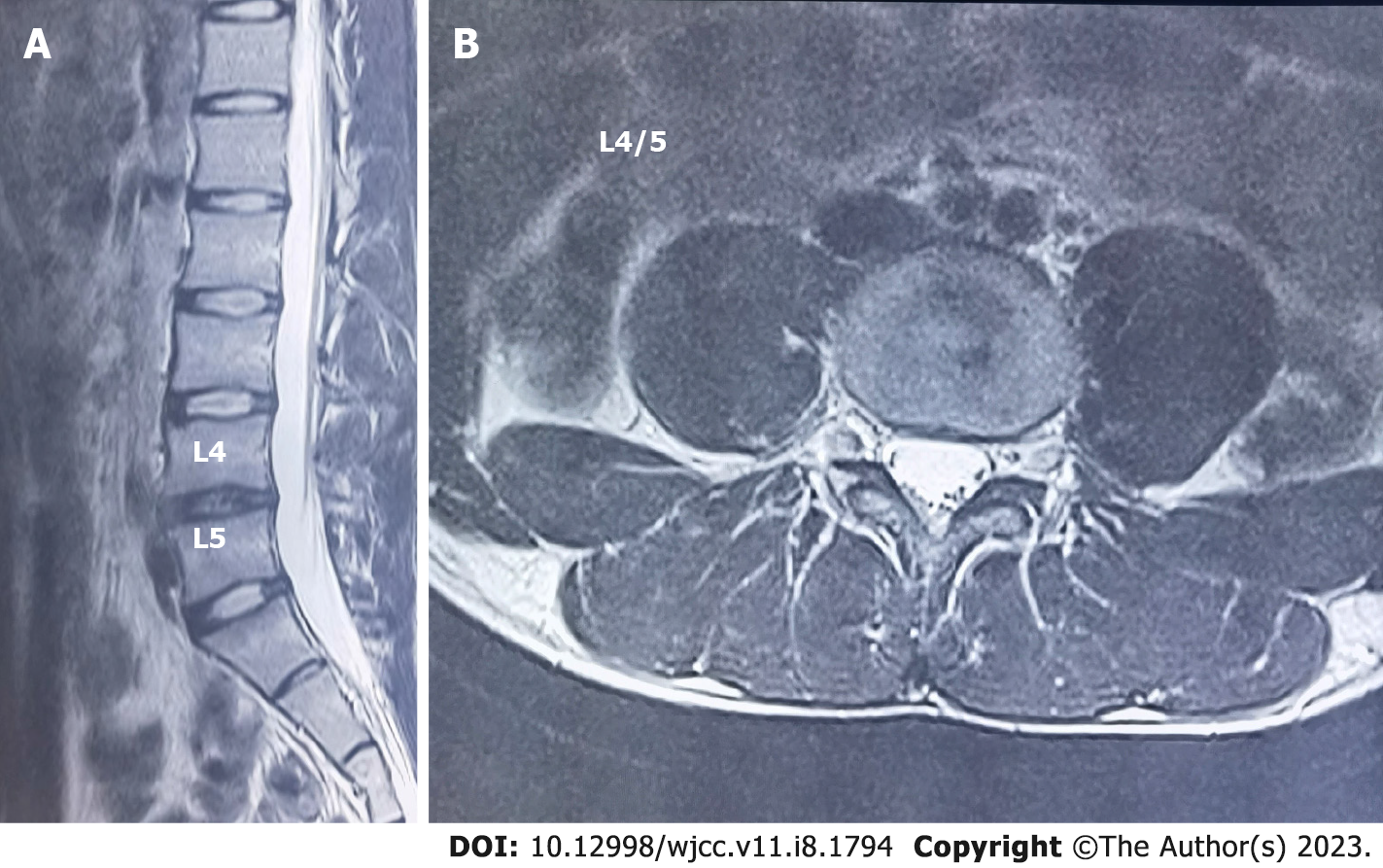
The height of L4/5 intervertebral space was lower in the radiographs of lumbar spine (Figure 1); Sagittal (left) and axial (right) T2-weighted magnetic resonance imaging of the lumbar spine images showed obvious degeneration of the L4/5 disc (Figure 2).
Discogenic low back pain with testicular pain.
The procedure was performed under fluoroscopy, and we used a standard posterolateral approach and a double needle technique[4]. We conducted the discography for the L3/4 disc and the L4/5 disc. About 0.2 mL of 2% lidocaine hydrochloride was slowly injected into the nucleus pulposus after the needle was accurately inserted into the center of the disc. When performing discography on the L3/4 disc, there was no change in low back pain or testicular pain. In contrast, when discography on the L4/5 disc was performed, the patient clearly demonstrated a significant improvement in low back pain. At almost the same time, testicular pain disappeared. Subsequently, about 0.3 mL of 1% methylene blue was injected into the diseased disc. The patient required bedrest for the 24 h after surgery.
The patient’s bilateral testicular pain quickly disappeared after the analgesic discography. The testicular pain VAS score was 0, and the low back pain VAS score was 2.
At the 1-year follow-up, the patient’s testicular pain did not recur, and the patient's low back pain improved significantly.
Chronic testicular pain originating from lumbar disc degeneration is very rare clinically. This may be due to the insufficient awareness of this disease or the lack of a clear diagnostic method. In 2003, Doubleday et al[5] reported a case who had central low back symptoms and right testicular pain with a small central disc protrusion between the T12 and L1 vertebrae. They successfully eased the symptoms with 12 sessions of physical therapy during a 3-mo period. Peng et al[6] has also reported that degenerative lumbar spondylolisthesis can cause testicular pain and suggested that this type of testicular pain is an involvement pain arising from lumbar spine disease.
Bogduk et al[7] showed the innervation of cervical and lumbar intervertebral discs, which receive innervation posteriorly from the sinuvertebral nerves, laterally from the vertebral nerve and anteriorly from the sympathetic trunks. Furthermore, the innervation of cervical and lumbar discs is multi-segmental[8,9]. For example, low back pain caused by L4/5 or L5/S1 disc degeneration is not transmitted upward via the L5 or S1 spinal nerves as traditionally believed but is transmitted through the paravertebral sympathetic chain to the dorsal root ganglia of L1 and L2 and then to the center[6]. In addition, the distribution of nerves in the lumbar disc is consistent with the distribution of nerves in the testis (genitofemoral nerve and genital branch of the ilioinguinal nerve), mainly originating from the L1 and L2 nerve roots[9]. Such neural pathways provide the basis for testicular pain induced by intervertebral disc degeneration.
Lumbar discography and methylene blue injection are common clinical methods for the diagnosis and treatment of discogenic lower back pain. The vascularized granulation tissue and the tissue repair process of injurious nerve fibers growing into the degenerated disc are important pathophysiological mechanisms of discogenic lower back pain[10]. Methylene blue as a nerve inactivator can inhibit the nociceptive nerves growing into the lumbar disc, eventually making the pain disappear[10]. For the patient in this case, the imaging manifestations and positive signs were typical signs of discogenic low back pain, and the analgesic discography improved both low back pain and testicular pain. After intradiscal methylene blue injection, the low back pain and testicular pain improved, suggesting that the testicular pain possibly originated from lumbar disc degeneration rather than the testis itself.
The mechanism of discogenic testicular pain may therefore originate from the pain induced by the degenerated L4/5 disc non-segmentally transmitted through the paravertebral sympathetic chain to the L1 and L2 spinal nerve roots and then upward in conjunction with visceral sympathetic afferent nerves transmitted in the L1 and L2 spinal nerve roots[11]. In the present case, the patient's diagnosis and treatment were based on discogenic low back pain rather than specifically on testicular pain. Although lumbar analgesic discography suppressed both low back pain and testicular pain, this does not mean that lumbar analgesic discography is an effective method for diagnosed testicular pain. However, the disappearance of testicular pain in the patient after the procedure may further support that lumbar disc degeneration is a significant clinical resource for testicular pain.
In this case, we found that disc degeneration, as the etiology of low back pain, can also evoke concomitant testicular pain. Analgesic discography can be chosen as an effective diagnostic method, and intradiscal methylene blue injection can significantly improve low back pain and testicular pain.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rakhshan V, Iran; Zhou T, China S-Editor: Liu GL L-Editor: Filipodia P-Editor: Liu GL
| 1. | Calixte N, Brahmbhatt J, Parekattil S. Chronic Testicular and Groin Pain: Pathway to Relief. Curr Urol Rep. 2017;18:83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Vanoli S, Vouga L, Iselin C. [Chronic testicular pain: A multidisciplinary challenge]. Rev Med Suisse. 2021;17:2086-2089. [PubMed] |
| 3. | Chu ECP. Taming of the Testicular Pain Complicating Lumbar Disc Herniation With Spinal Manipulation. Am J Mens Health. 2020;14:1557988320949358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine (Phila Pa 1976). 1995;20:1878-1883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 545] [Cited by in RCA: 464] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 5. | Doubleday KL, Kulig K, Landel R. Treatment of testicular pain using conservative management of the thoracolumbar spine: a case report. Arch Phys Med Rehabil. 2003;84:1903-1905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Peng B, Li D, Pang X. Degenerative lumbar spondylolisthesis with testicular pain. Pain Med. 2014;15:169-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Bogduk N, Windsor M, Inglis A. The innervation of the cervical intervertebral discs. Spine (Phila Pa 1976). 1988;13:2-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 104] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Wu B, Yang L, Peng B. Ingrowth of Nociceptive Receptors into Diseased Cervical Intervertebral Disc Is Associated with Discogenic Neck Pain. Pain Med. 2019;20:1072-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Masarani M, Cox R. The aetiology, pathophysiology and management of chronic orchialgia. BJU Int. 2003;91:435-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Peng B, Pang X, Wu Y, Zhao C, Song X. A randomized placebo-controlled trial of intradiscal methylene blue injection for the treatment of chronic discogenic low back pain. Pain. 2010;149:124-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Murata Y, Kato Y, Miyamoto K, Takahashi K. Clinical study of low back pain and radicular pain pathways by using l2 spinal nerve root infiltration: a randomized, controlled, clinical trial. Spine (Phila Pa 1976). 2009;34:2008-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |