Published online Mar 6, 2023. doi: 10.12998/wjcc.v11.i7.1650
Peer-review started: December 7, 2022
First decision: January 19, 2023
Revised: January 27, 2023
Accepted: February 15, 2023
Article in press: February 15, 2023
Published online: March 6, 2023
Processing time: 85 Days and 6.8 Hours
Patients with foreign bodies in the digestive tract are often encountered, but complete penetration of a foreign body through the gastrointestinal tract is rare, and the choice of imaging method is very important. Improper selection may lead to missed diagnosis or misdiagnosis.
An 81-year-old man was diagnosed as having a liver malignancy after he took magnetic resonance imaging and positron emission tomography/computed tomography (CT) examinations. The pain improved after the patient accepted gamma knife treatment. However, he was admitted to our hospital 2 mo later due to fever and abdominal pain. This time, he received a contrast-enhanced CT scan, which showed fish-boon-like foreign bodies in the liver with peripheral abscess formation, then he went to the superior hospital for surgery. It lasted for more than 2 mo from the onset of the disease to the surgical treatment. A 43-year-old woman with a 1 mo history of a perianal mass with no obvious pain or discomfort was diagnosed as having an anal fistula with the formation of a local small abscess cavity. Clinical perianal abscess surgery was performed, and fish bone foreign body was found in perianal soft tissue during the operation.
For patients with pain symptoms, the possibility of foreign body perforation should be considered. Magnetic resonance imaging is not comprehensive and that a plain computed tomography scan of the pain area is necessary.
Core Tip: We report two cases of digestive tract foreign body perforation, with one foreign body located in the liver and the other foreign body located around the anus, both of which were misdiagnosed by magnetic resonance examination. We hope that through our report, there will be more diagnostic ideas for similar problems in clinics in the future.
- Citation: Ji D, Lu JD, Zhang ZG, Mao XP. Misdiagnosis of food-borne foreign bodies outside of the digestive tract on magnetic resonance imaging: Two case reports. World J Clin Cases 2023; 11(7): 1650-1655
- URL: https://www.wjgnet.com/2307-8960/full/v11/i7/1650.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i7.1650
Patients with foreign bodies in the digestive tract are often encountered in the emergency room. The most common foreign bodies include fish bones, date stones, chicken bones, and toothpicks[1]. To achieve a precise diagnosis, imaging is often performed first; however, the choice of imaging modality is extremely important. A study has shown that the detection rate for fishbone foreign bodies is only 32%[2]. Ultrasound can detect most foreign bodies; however, ultrasound is susceptible to gastrointestinal gas interference, limited by low image resolution and operator's skills, and have a high probability of misdiagnosis[3,4]. Computed tomography (CT) has a good density resolution. A foreign body has a strong contrast, in color and texture, with the surrounding soft tissue and, as such, can be easily detected on a regular CT examination. As reported in the medical literature, CT has a 100% sensitivity for the recognition of calcified foreign bodies[5]. Magnetic resonance imaging (MRI) is not a good option for detecting foreign bodies in or out of the digestive tract. It is likely to lead to missed diagnosis or misdiagnosis. This report describes two patients in whom a foreign body completely perforated the digestive tract. Neither patient had typical clinical manifestations of digestive tract perforation. MRI without CT was performed before surgery, which is a likely cause of the misdiagnoses.
Case 1: On May 26, 2014, an 81-year-old man developed a fever (39.2 ℃) of unknown cause accompanied by general weakness presented in our clinic.
Case 2: A 43-year-old woman presented with a 1 mo history of a perianal mass with no obvious pain or discomfort.
Case 1: The fever had been lasted for several hours.
Case 2: The perianal mass had lasted for over a month.
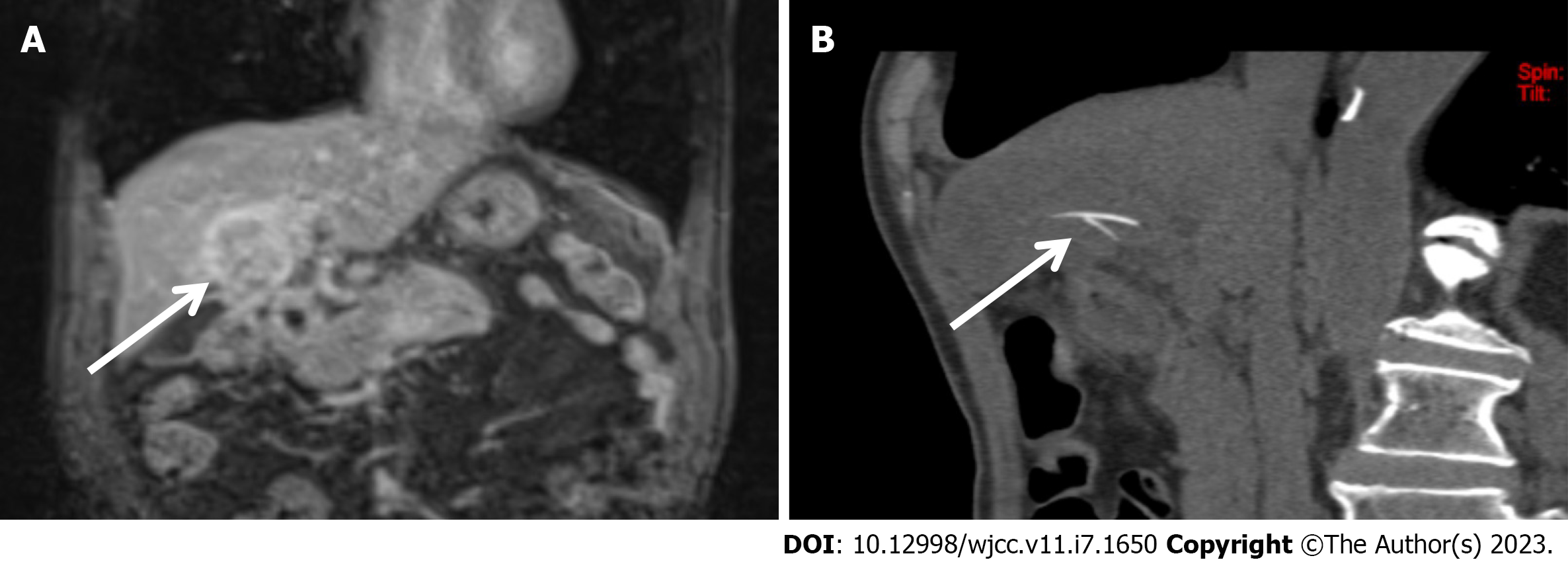
Case 1: At the end of March 2014, the patient developed upper abdominal pain and discomfort without chills or fever and was admitted to the First People’s Hospital of our city. Electronic gastroscopy was performed during hospitalization, but no abnormality was found. Abdominal MRI showed that there was a mass in the Ⅳ segment of his liver, and the possibility of a malignant tumor was considered (Figure 1A). Laboratory examination showed that the alpha fetoprotein concentration was normal, and hepatitis B virus test was negative. On April 11, 2014, the patient underwent positron emission tomography/CT examination at Huaxi Hospital in Jiangyin City. This imaging examination showed a hypermetabolic mass in the Ⅳ segment of the liver, and the possibility of liver cancer with a tumor thrombus in the inferior vena cava was considered. Significant fluorodeoxyglucose uptake was present. The patient was then admitted to the 81st Hospital of the Chinese People’s Liberation Army and diagnosed with primary liver cancer. He underwent gamma knife treatment for the liver mass in mid-April 2014. The abdominal pain improved after surgery.
Case 2: Past medical history was not remarkable for this patient.
The personal and family history was not remarkable for these two patients.
Case 1: The patient had not receive special medical examination.
Case 2: A specialist examination revealed a 4 cm × 4 cm mass 3 cm away from the anal verge at 8-11-o’clock of lithotomy position. The skin temperature over the mass was elevated, the mass was painful when touched, and it exhibited no obvious fluctuation on palpation. Digital examination and anoscopy were not performed because of pain.
Case 1: The patient had a white blood cell count of 7.4 × 109/L and C-reactive protein level of 108 mg/L.
Case 2: The patient had a white blood cell count of 8.08 × 109 g/L, neutrophil ratio of 0.775, lymphocyte ratio of 0.158, and C-reactive protein level of 77.9 mg/L.
Case 1: In march 2014, Abdominal MRI showed that there was a mass in the Ⅳ segment of his liver and the possibility of a malignant tumor was considered. On April 11, 2014, the patient underwent positron emission tomography/CT examination. This imaging examination showed a hypermetabolic mass in the Ⅳ segment of the liver, and the possibility of liver cancer with a tumor thrombus in the inferior vena cava was considered. Significant fluorodeoxyglucose uptake was present. CT examination on June 9, 2014 showed multiple annular low-density shadows in the left hepatic lobe after the previous gamma knife treatment. The possibility of infection, the presence of linear dense shadows, and the possibility of foreign bodies were considered (Figure 1B).
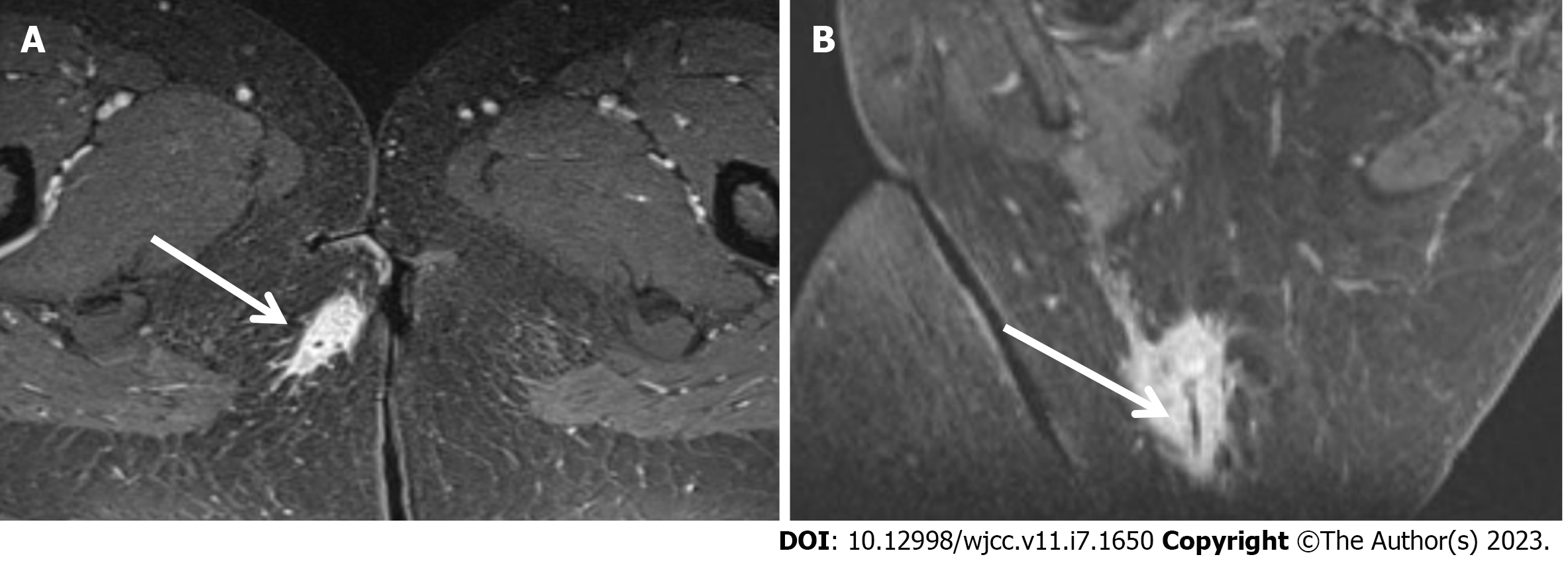
Case 2: MRI in August 12 showed an abnormal signal in the back of the anal canal; this abnormal signal started at the 9-o’clock position of the anal canal, extended to the posterolateral side of the external anal sphincter, and ended at the skin of the right posterior buttock. There was a low signal on T1WI sequence and high signal on T2 fat-suppression sequence. An enhanced scan showed obvious local enhancement. Tube-like unenhanced areas can be seen in some layers. Additionally, exudation changes were present in the surrounding subcutaneous fat (Figure 2).
Case 1: The final diagnosis of the patient was liver abscess caused by fish bone.
Case 2: The final diagnosis of the patient was para-anal abscess caused by fish bone.
Case 1: The patient went to Shanghai Changhai Hospital for special liver segmentectomy + cholecystectomy + intestinal adhesion release.
Case 2: The patient accepted perianal abscess resection + catheter drainage + removal of foreign body in the anus.
The two patients were cured.
The clinical manifestations of foreign body perforation of the digestive tract vary according to the perforation site[6]. The most common presentation is pain at the perforation site, followed by fever and peritonitis; however, pneumoperitoneum is rare[7]. Unlike acute gastrointestinal perforation caused by ulcers or trauma, gastrointestinal perforation caused by foreign bodies often presents as a chronic process, and clinical peritonitis can progress to subacute or abscessation with milder clinical symptoms[1,8-10]. Because most patients are unable to recall a history of foreign body ingestion, emergency physicians often do not consider the diagnosis of a gastrointestinal tract foreign body[9]. Choosing the most appropriate imaging method is very important and is correlated with the accuracy of diagnosis.
The two cases of foreign bodies described in the present report were misdiagnosed. One foreign body was found more than 2 mo after the onset of symptoms, and the other was found during surgery. The first patient was diagnosed with a malignant tumor and underwent gamma knife treatment. Neither patient recalled a history of foreign body ingestion when they were admitted to the hospital. The time from symptom onset to admission was long. The clinical manifestations were dull pain at the lesion site, and there were no typical symptoms of gastrointestinal perforation, and no obvious free gas on imaging. Ultrasound and MRI examinations were performed in case 2, which suggested anal fistula. Case 1 was considered to have a liver malignancy. The misdiagnosis of case 1 led to incorrect clinical management and brought great physical and mental pain to the patient. We believe that the main reasons for misdiagnosis in the two cases described in the present report are as follows: (1) The patients did not provide a history of foreign bodies; (2) The disease course was long, the clinical symptoms were mild, and there were no typical symptoms of gastrointestinal perforation; and (3) It is rarely to see foreign bodies that penetrate the gastrointestinal tract completely. Moreover, many physicians are inexperienced in the selection of imaging protocols for such cases, and clinicians and radiologists do not consider the possibility of foreign body puncture.
In patients with perforation of the digestive tract by foreign bodies who undergo MRI, an inflammatory mass develops near the perforation site, the MRI resolution is high, and the lesions are easy to find[11]. However, because of the dense tissue of the foreign body, the MRI signal is extremely low, and the lesion is easily mistaken for gas; thus, misdiagnosis may occur[12]. When the foreign body is located in a solid organ, it is easy to confuse the foreign body for an abscess or tumor on MRI[13,14]. In particular, when the inflammatory mass is blurred and the boundary with the surrounding tissue is unclear, it is easily misdiagnosed as an advanced tumor[15]. In these cases, doctors and patients often forgo surgery; this occurred in case 1 of the present report, in whom a fish bone penetrated the liver. When the foreign body is located in a hollow organ, a large number of artifacts will be generated because of the influence of gas, making the diagnosis more difficult. Missed diagnosis or misdiagnosis is especially common when the patient does not provide a history of foreign body ingestion.
According to the literature, the sensitivity of CT for the identification of calcified foreign bodies is 100%. In one retrospective study, all fish bone foreign bodies were found by CT. The CT density resolution is good, and such foreign bodies have strong contrast with the surrounding soft tissue and are thus easy to find[16,17]. Especially if the patient provides a history of foreign body ingestion, the doctor can specifically look for the lesion in the area of discomfort, which can greatly improve the detection rate. Three-dimensional CT reconstruction can be used to reconstruct the overall shape and direction of foreign bodies, providing assistance for surgery[18]. Contrast-enhanced scans are not recommended for initial diagnosis. Ingested contrast agent will cover the foreign body, greatly increasing the risk of missed diagnosis[19]. Research has shown that blood vessels are easily confused with foreign bodies after enhanced scanning; however, we believe that if clinicians are careful enough and use anatomical knowledge to observe suspicious high densities at the scan level, blood vessels can be distinguished from foreign bodies[9]. This combined with the high diagnostic accuracy of 3D reconstruction can greatly improve the chance of a correct diagnosis.
In conclusion, we believe that for patients with local pain as the main symptom, clinicians should consider the possibility of perforation of the digestive tract by a foreign body. Obtaining the history of the patient’s living and eating habits in combination with CT examination of the pain site is helpful for diagnosis.
The authors thank the patients and their family. We also thank the whole project team who worked on these two cases.
| 1. | E Silva GS, Gomes NBN, Pacheco EO, Bezerra FMR, Nunes RB, Mcphee HL, Torres US, D'Ippolito G. Emergency CT of abdominal complications of ingested fish bones: what not to miss. Emerg Radiol. 2021;28:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 2. | Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg. 1990;211:459-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 174] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Li F, Zhou X, Wang B, Guo L, Ma Y, Wang D, Wang L, Zhang L, Wang H, Tian M, Tao M, Xiu D, Fu W. Intestinal Perforation Secondary to Pits of Jujube Ingestion: A Single-Center Experience with 18 Cases. World J Surg. 2019;43:1198-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Coppolino F, Gatta G, Di Grezia G, Reginelli A, Iacobellis F, Vallone G, Giganti M, Genovese E. Gastrointestinal perforation: ultrasonographic diagnosis. Crit Ultrasound J. 2013;5 Suppl 1:S4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Park S, Choi DS, Shin HS, Cho JM, Jeon KN, Bae KS, Koh EH, Park JJ. Fish bone foreign bodies in the pharynx and upper esophagus: evaluation with 64-slice MDCT. Acta Radiol. 2014;55:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Shin D, Rahimi H, Haroon S, Merritt A, Vemula A, Noronha A, LeBedis CA. Imaging of Gastrointestinal Tract Perforation. Radiol Clin North Am. 2020;58:19-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Emir S, Ozkan Z, Altınsoy HB, Yazar FM, Sözen S, Bali I. Ingested bone fragment in the bowel: Two cases and a review of the literature. World J Clin Cases. 2013;1:212-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Lee NK, Kim S, Hong SB, Lee SJ, Kim TU, Ryu H, Lee JW, Kim JY, Suh HB. CT diagnosis of non-traumatic gastrointestinal perforation: an emphasis on the causes. Jpn J Radiol. 2020;38:101-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Paixão TS, Leão RV, de Souza Maciel Rocha Horvat N, Viana PC, Da Costa Leite C, de Azambuja RL, Damasceno RS, Ortega CD, de Menezes MR, Cerri GG. Abdominal manifestations of fishbone perforation: a pictorial essay. Abdom Radiol (NY). 2017;42:1087-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Gheorghiu MI, Bolliet M, David P, Denis B. Case report of abdominal left upper quadrant collection secondary to fish bone perforation. Med Pharm Rep. 2020;93:301-305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Mortelé KJ, Segatto E, Ros PR. The infected liver: radiologic-pathologic correlation. Radiographics. 2004;24:937-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 205] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 12. | Wehrli FW. Magnetic resonance of calcified tissues. J Magn Reson. 2013;229:35-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Chan JH, Tsui EY, Luk SH, Fung AS, Yuen MK, Szeto ML, Cheung YK, Wong KP. Diffusion-weighted MR imaging of the liver: distinguishing hepatic abscess from cystic or necrotic tumor. Abdom Imaging. 2001;26:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 137] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 14. | Choo YH, Seo Y. Multiple brain abscesses presented with monoparesis in a patient with lung abscess mimicking lung cancer. Radiol Case Rep. 2021;16:3007-3011. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Feraco P, Donner D, Gagliardo C, Leonardi I, Piccinini S, Del Poggio A, Franciosi R, Petralia B, van den Hauwe L. Cerebral abscesses imaging: A practical approach. J Popul Ther Clin Pharmacol. 2020;27:e11-e24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Koito Y, Asano T, Matsumoto S, Mashima H. Endoscopic Mucosal Incision to Remove a Fish Bone Completely Embedded Under the Esophageal Mucosa: A Case Report and Literature Review. Am J Case Rep. 2022;23:e936773. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Deniz MA, Turmak M. CT Evaluation of Swallowed Foreign Bodies Located in the Gastrointestinal System. Cureus. 2022;14:e26355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 18. | Goh BK, Tan YM, Lin SE, Chow PK, Cheah FK, Ooi LL, Wong WK. CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol. 2006;187:710-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 140] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 19. | Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L, Meining A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 439] [Article Influence: 43.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hefny AF, United Arab Emirates; Shiryajev YN, Russia S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL