Published online Feb 6, 2023. doi: 10.12998/wjcc.v11.i4.903
Peer-review started: September 9, 2022
First decision: October 12, 2022
Revised: October 21, 2022
Accepted: January 10, 2023
Article in press: January 10, 2023
Published online: February 6, 2023
Processing time: 149 Days and 22.1 Hours
Duodenum-preserving pancreatic head resection (DPPHR) is the choice of surgery for benign or low-grade malignant tumors of the pancreatic head. Laparoscopic DPPHR (LDPPHR) procedure can be improved by preoperative 3D model reconstruction and the use of intravenous indocyanine green fluorescent before surgery for real-time navigation with fluorescent display to guide the surgical dissection and prevention of from injury to vessels and biliary tract.
Here we report the successful short- and long-term outcomes after one year following LDPPHR for a 60-year lady who had an uneventful recovery and was discharged home one week after the surgery.
There was no bile leakage or pancreatic leakage or delayed gastric emptying. The histopathology report showed multiple cysts in the pancreatic head and localized pancreatic intraepithelial tumor lesions. The resected margin was free of tumor.
Core Tip: Duodenum-preserving pancreatic head resection (DPPHR) is the choice of surgery for benign or low-grade malignant tumors of the pancreatic head. Laparoscopic DPPHR (LDPPHR) procedure can be improved by preoperative 3D model reconstruction and the use of intravenous indocyanine green fluorescent before surgery for real-time navigation with fluorescent display to guide the surgical dissection and prevention of from injury to vessels and biliary tract. Here we report the successful short- and long-term outcomes after one year following LDPPHR for a 60-year lady who had an uneventful recovery and was discharged home one week after the surgery. There was no bile leakage or pancreatic leakage or delayed gastric emptying. The histopathology report showed multiple cysts in the pancreatic head and localized pancreatic intraepithelial tumor lesions. The resected margin was free of tumor.
- Citation: Li XL, Gong LS. Preoperative 3D reconstruction and fluorescent indocyanine green for laparoscopic duodenum preserving pancreatic head resection: A case report. World J Clin Cases 2023; 11(4): 903-908
- URL: https://www.wjgnet.com/2307-8960/full/v11/i4/903.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i4.903
Duodenum-preserving pancreatic head resection (DPPHR) is the choice of surgery for benign or low-grade malignant tumors of the pancreatic head. The most common benign and borderline pancreatic neoplastic lesions include Cystic Tumor, Neuroendocrine Tumor, Solid Pseudopapillary Tumor and Intraductal Papillary Mucinous Neoplasm (IPMN). The DPPHR was first reported in 1972 by Beger for the treatment of the inflammatory mass caused by chronic pancreatitis[1]. Compared with traditional pancreatic surgery, this procedure retains the gastroduodenal continuity, reduces the extent of pancreatic resection, retains the pancreatic intestinal axis, and help preserve normal anatomical and physiological structures with good short- and long-term outcome. A variety of modifications in surgical techniques have been proposed, such as Frey's operation, Berne's operation, Takada's operation, etc[2-5].
With the development of minimally invasive and precision medicine, laparoscopic DPPHR (LDPPHR) has become a better option, but it is less practiced and rarely reported because of the complexity of the operation. Combined with fluorescence technology and preoperative 3D model reconstruction, the LDPPHR under fluorescence navigation is beneficial. The fluorescence dye, indocyanine green (ICG) used intravenously during surgery is excreted through the bile, showing green fluorescence under near-infrared light excitation[6]. The use of fluorescence navigation technology greatly improves the visualization of biliary anatomy for accurate planning and resection and prevents intraoperative bile duct injury. In extrahepatic biliary fluorescence imaging, Vlek et al[7] used the method of injecting ICG through peripheral vein 15~60 min before operation. After ICG was injected into peripheral vein, the liver could fluoresce within 2-5 min, and the biliary tract could fluoresce within 8-10 min. The concentration in bile reached its peak 30 min to 2 h after ICG intravenous injection.
A female patient, aged 60 years, was admitted with a pancreatic head mass found during the physical check-up.
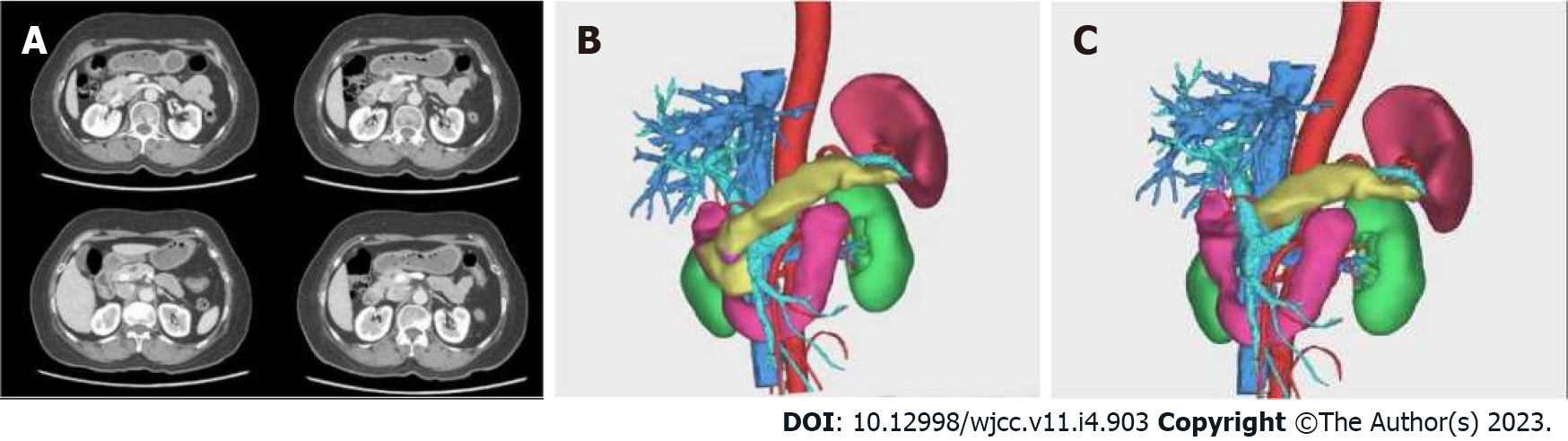
A female patient, aged 60 years, was admitted with a pancreatic head mass found during the physical check-up. The blood routine, coagulation profile, liver function, renal function, serum electrolyte, the markers of HBV, and tumor antigen screening tests were normal. Endoscopic ultrasonography showed multiple mixed-echo nodules in the head and neck of the pancreas, with irregular shape and clear boundary, and mainly a hypoechoic parenchyma. The computed tomography (CT) scan showed cystic lesions in the head and neck of the pancreas. Some lesions were connected to the main pancreatic duct, suspicious of IPMN. The CT angiography (CTA) and venous-phase imaging (CTV) of peripancreatic vessels were normal (Figure 1A).
The blood routine, coagulation profile, liver function, renal function, serum electrolyte, the markers of HBV, and tumor antigen screening tests were normal.
Endoscopic ultrasonography showed multiple mixed-echo nodules in the head and neck of the pancreas, with irregular shape and clear boundary, and mainly a hypoechoic parenchyma. The CT scan showed cystic lesions in the head and neck of the pancreas. Some lesions were connected to the main pancreatic duct, suspicious of IPMN. The CTA and CTV of peripancreatic vessels were normal (Figure 1A).
The 3D reconstruction preoperatively (Figure 1B), and plan of surgical resection with postoperative pancreatic changes are visualized (Figure 1C).
Multiple cysts in pancreatic head and localized pancreatic intraepithelial tumor lesions (PanIN-2).
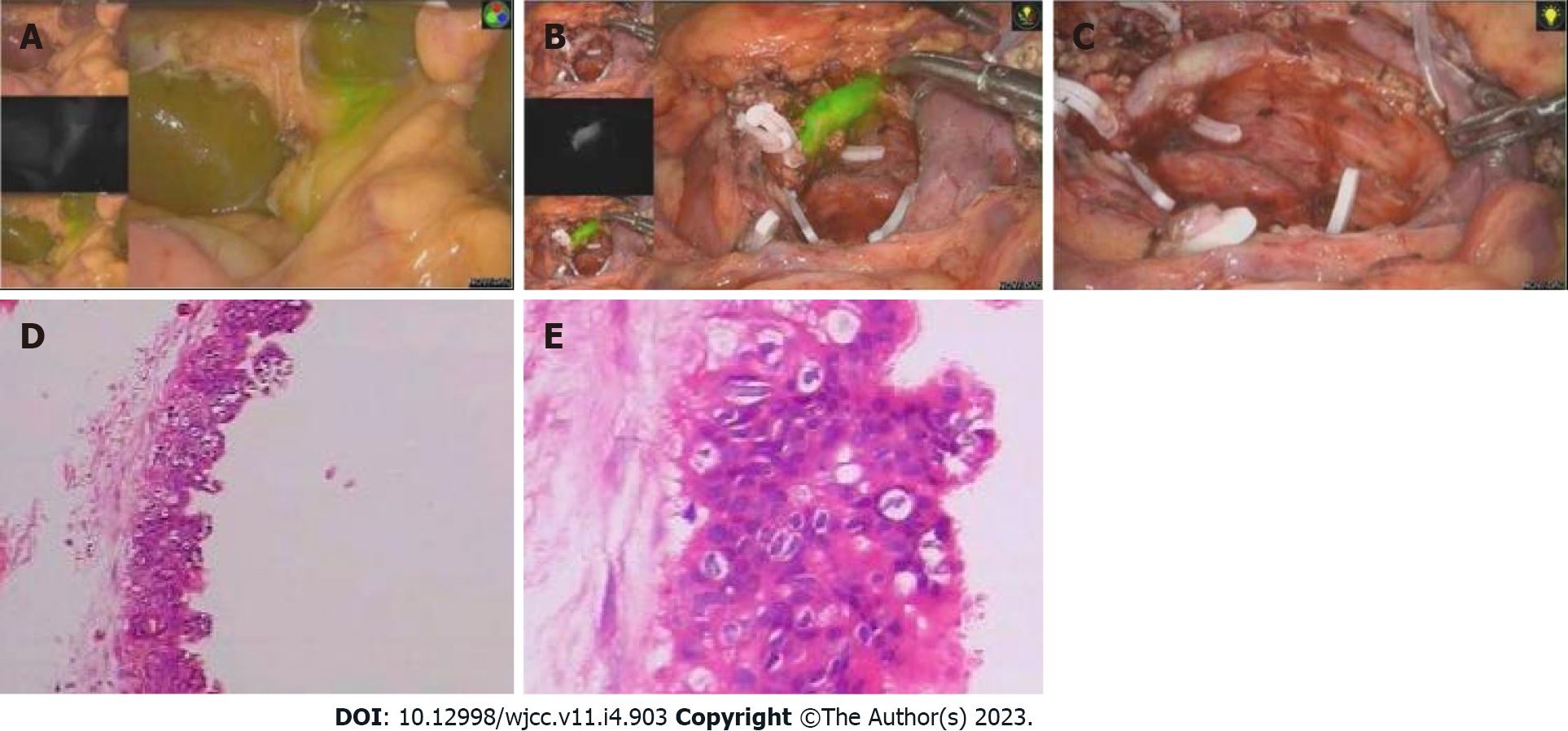
15 min Before operation, one ml (2.5 mg) ICG was injected into the peripheral vein (if the biliary tract development is not satisfactory during operation, the additional dose can be continued). The gastrocolonic ligament was dissected with an ultrasonic knife under laparoscopy, multiple cystic tumors in the pancreatic head were noted. The ultrasonic knife was used for dissection of duodenum and pancreatic head. The superior mesenteric vein was dissected at the lower edge of the pancreas. The tunnel behind the pancreatic neck was established. The pancreatic neck was taped and transected. The bile duct was evaluated in fluorescence laparoscopic mode (Figure 2A). Under fluorescent navigation, dissection of the uncinate process of the pancreas was continued from the lower border and upward under the postpancreatic head capsule. The anterior and posterior inferior pancreaticoduodenal vessels were exposed, and the branches of vessels entering the pancreas were severed keeping the integrity of the posterior fascia of the pancreas. Gastroduodenal artery was dissected. The superior anterior pancreaticoduodenal artery branches entering the pancreatic head were cut, retaining the blood supply of the duodenum. With fluorescent display, the pancreatic tissue was dissected off along the posterior fascial plane of the pancreatic head, protect the common bile duct, duodenum and its blood supply. There was no bile leakage and bleeding detected under fluorescent laparoscopy (Figure 2B and C). For digestive tract reconstruction, the jejunum was severed at 15 cm from the Treitz ligament, the distal jejunum was pulled out from behind the colon, the pancreatic duct was cannulated with a silicone tube, and end-to-side pancreatojejunostomy was performed using continuous 3-0 absorbable suture (Vicryl®). Roux-Y jejuno-jejunostomy was performed about 45 cm away from the pancreatojejunostomy. There was no bleeding, bile leakage and pancreatic leakage. An abdominal drainage tube was placed behind the pancreatojejunostomy (Video).
Post-operative recovery was uneventful. On the 4th day white blood cell: 7.7 x 109 /L. Percentage of neutrophils: 82%, hemoglobin: 114 g/L. Serum albumin: 34 g/L, Serum total bilirubin: 10.3 μmol/L, Serum direct bilirubin: 5.2 μmol/L, ascites amylase: 149 U/L. Postoperative pathological report showed multiple cysts in pancreatic head and localized pancreatic intraepithelial tumor lesions (PanIN-2). Resected margin was free of tumor (Figure 2D and E).
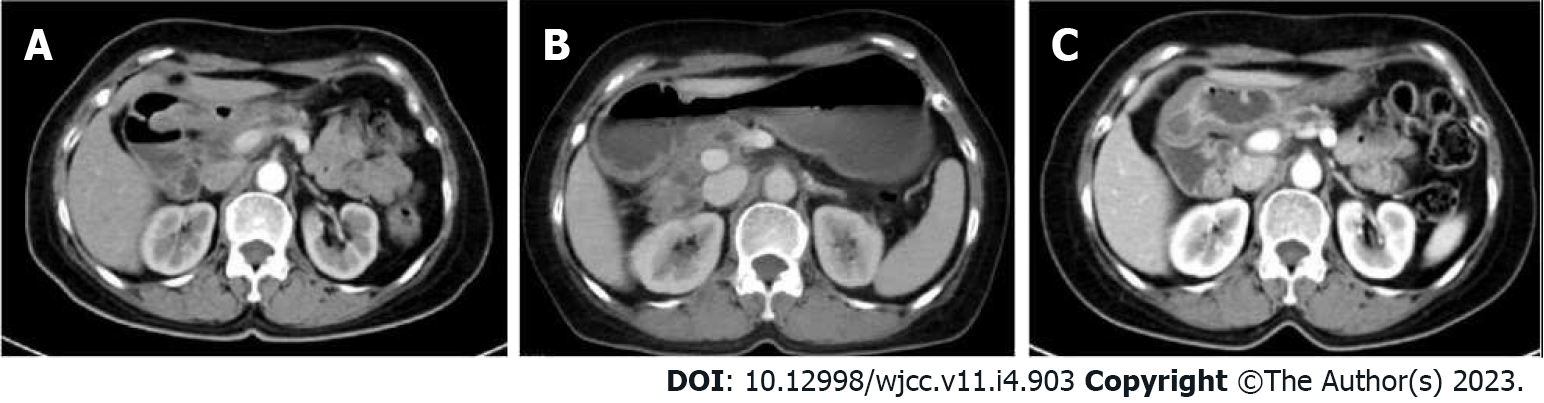
Follow up CT after 5 mo (Figure 3A), 11 mo (Figure 3B) and 17 mo (Figure 3C) were normal. The follow-up hepatorenal function and blood sugar were normal.
In our case the outcome of LDPPHR was satisfactory without biliary or pancreatic leakage, and at one-year follow-up the CT scan, liver function and blood sugar tests were normal. The preoperative 3D reconstruction and intraoperative use of ICG fluorescent was helpful in anatomical dissection, avoiding injury to important vessels and biliary tract.
The traditional pancreaticoduodenectomy (PD) for benign or low-grade malignant tumors of the head of the pancreas, is now performed by laparoscopic PD (LPD) with overall mortality reduced to about 1% in large volume centers. However, postoperative morbidity and complications is still as high as 40%-60%, including malnutrition and pancreatic dysfunction[8]. Patients with benign tumors or low-grade malignant tumors of the pancreatic head will survive for a long time after surgical treatment, If LPD is performed, it may seriously affect the safety and quality of life of the patients after operation. DPPHR with various modifications is a more reasonable procedure for patients with benign and low-grade malignant tumors of the pancreatic head removes the tumor of the pancreatic head, retaining the continuity of gastro-duodenum and biliary tract anatomy and physiological functions. The minimally invasive laparoscopy resection LDPPHR has gained acceptance[9,10].
Intraoperative use of ICG fluorescent has added advantage in dissection and preservation of important vessels, for example, the blood supply of the duodenal papilla and the intrapancreatic part of the bile duct mainly comes from the supply of the posterior pancreaticoduodenal artery arch[11,12], the duodenal papilla is mainly supplied by the papillary artery from the superior posterior pancreaticoduodenal artery, protecting the posterior pancreaticoduodenal artery arch is particularly important for maintaining a good blood supply to the duodenum, the intrapancreatic part of the bile duct and the duodenal papilla. During the LDPPHR procedure in our case, the posterior fascia of the pancreatic head was preserved to avoid damaging the posterior pancreaticoduodenal artery arch, and the anterior pancreaticoduodenal artery arch was preserved as much as possible.
The application of 3D visualization technology combined with 3D printing technology in liver cancer and hilar cholangiocarcinoma has been reported in the literature. The variation of bile duct and blood vessel and the transverse and longitudinal infiltration of tumor can be observed clearly and stereoscopically from multiple dimensions to judge whether the tumor invades blood vessels and the resectability of the tumor. Preoperative 3D model reconstruction can plan different surgical approaches and resection ranges, select the best individualized surgical scheme, and achieve the purpose of accurate lesion resection [13,14]. In this case, the application of 3D visualization technology to LDPPHR has achieved satisfactory results in preoperative diagnosis, surgical planning and intraoperative real-time navigation. By constructing a 3D model before operation, we can more intuitively observe the scope of pancreatic lesions, observe that there is no vascular anatomical variation in this case, and preserve the anterior and posterior pancreaticoduodenal arterial arches to the greatest extent during the operation. In this way, we can "have a clear mind" before operation and “skill and ease" during operation. It laid the foundation for the success of the operation.
ICG, as a water-soluble dye for intravenous injection, can be selectively absorbed by the liver and excreted through the bile. After binding with mucin in the bile, ICG presents green fluorescence under near-infrared light excitation, which provides the possibility for fluorescence visualization of bile duct[15]. In a study by Wikner et al[16], it is easier to expose the common bile duct in ICG fluorescence mode than in traditional mode. The exposure of the intrapancreatic part of the bile duct and blood supply protection are a major difficulty in this operation. If the intrapancreatic part of the bile duct was difficult to be exposed due to inflammation or other factors, ICG fluorescence technology could achieve accurate navigation, and greatly reduces the difficulty of common bile duct exposure.
Use of preoperative 3D was helpful in precise planning, and the intraoperative fluorescent navigation aided in the surgical dissection, preserving the important vessels and biliary anatomy during LDPPHR. This procedure is worthy of promotion hospitals with such facilities.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Casella C, Italy; Cianci P, Italy S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Beger HG, Kunz R, Poch B. The Beger procedure--duodenum-preserving pancreatic head resection. J Gastrointest Surg. 2004;8:1090-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Frey CF, Smith GJ. Description and rationale of a new operation for chronic pancreatitis. Pancreas. 1987;2:701-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 274] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Gloor B, Friess H, Uhl W, Büchler MW. A modified technique of the Beger and Frey procedure in patients with chronic pancreatitis. Dig Surg. 2001;18:21-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 117] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Takada T, Yasuda H, Uchiyama K, Hasegawa H. Duodenum-preserving pancreatoduodenostomy. A new technique for complete excision of the head of the pancreas with preservation of biliary and alimentary integrity. Hepatogastroenterology. 1993;40:356-359. [PubMed] |
| 5. | Lu C, Jin WW, Mou YP, Zhou YC, Wang YY, Xia T, Zhu QC, Xu BW, Ren YF, Meng SJ, He YH, Jiang QT. [Clinical effect of minimally invasive duodenum preserving pancreatic head resection for benign and pre-malignant lesions of pancreatic head]. Zhonghua Waike Zazhi. 2022;60:39-45. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Hong D, Cheng J, Wu W, Liu X, Zheng X. How to Perform Total Laparoscopic Duodenum-Preserving Pancreatic Head Resection Safely and Efficiently with Innovative Techniques. Ann Surg Oncol. 2021;28:3209-3216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Vlek SL, van Dam DA, Rubinstein SM, de Lange-de Klerk ESM, Schoonmade LJ, Tuynman JB, Meijerink WJHJ, Ankersmit M. Biliary tract visualization using near-infrared imaging with indocyanine green during laparoscopic cholecystectomy: results of a systematic review. Surg Endosc. 2017;31:2731-2742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 97] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 8. | He K, Hong X, Chi C, Cai C, Wang K, Li P, Liu X, Li J, Shan H, Tian J. A new method of near-infrared fluorescence image-guided hepatectomy for patients with hepatolithiasis: a randomized controlled trial. Surg Endosc. 2020;34:4975-4982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Stauffer JA, Coppola A, Villacreses D, Mody K, Johnson E, Li Z, Asbun HJ. Laparoscopic versus open pancreaticoduodenectomy for pancreatic adenocarcinoma: long-term results at a single institution. Surg Endosc. 2017;31:2233-2241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 123] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 10. | Beger HG. Benign Tumors of the Pancreas-Radical Surgery Versus Parenchyma-Sparing Local Resection-the Challenge Facing Surgeons. J Gastrointest Surg. 2018;22:562-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Prete FP, Di Meo G, Liguori P, Gurrado A, De Luca GM, De Leo V, Testini M, Prete F. Modified "Blumgart-Type" Suture for Wirsung-Pancreaticogastrostomy: Technique and Results of a Pilot Study. Eur Surg Res. 2021;62:105-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Liang B, Chen Y, Li M, Dong X, Yao S, Liu T. Total laparoscopic central pancreatectomy with Roux-Y pancreaticojejunostomy for solid pseudopapillary neoplasm of pancreas: A case report. Medicine (Baltimore). 2019;98:e15495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Beger HG, Mayer B, Rau BM. Parenchyma-Sparing, Limited Pancreatic Head Resection for Benign Tumors and Low-Risk Periampullary Cancer--a Systematic Review. J Gastrointest Surg. 2016;20:206-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Bai RJ, Wang JE, Jiang HJ, Hao XJ, Dong XP, Huang YH, Wei L. Investigation on the optical scan condition for imaging of multi-slice spiral CT liver perfusion in rats. Chin Med J (Engl). 2013;126:4742-4746. [PubMed] |
| 15. | Dîrzu DS, Dicu C, Dîrzu N. Urinary retention: a possible complication of unilateral continuous quadratus lumborum analgesia - a case report. Rom J Anaesth Intensive Care. 2019;26:75-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 16. | Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthesia. 2017;72:230-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 89] [Article Influence: 8.9] [Reference Citation Analysis (1)] |