Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8404
Peer-review started: September 24, 2023
First decision: October 12, 2023
Revised: October 21, 2023
Accepted: October 27, 2023
Article in press: October 27, 2023
Published online: December 16, 2023
Processing time: 80 Days and 21.6 Hours
Phlebosclerosis is a common age-related fibrotic degeneration of the venous wall. It is a disorder rather than a disease, which may cause venous dysfunction and even venous thrombosis. It is rarely reported in patients with varicose veins.
The present report describes the case of a 70-year-old man with varicose veins, vitiligo, and phlebosclerosis. Venous angiography revealed blood reflux in the superficial and deep veins. The patient underwent surgery to remove the saphe
This is probably the first report of a wooden stick-like structure being found in the venous wall in patients with varicose veins and venous ulcers. Phlebosclerosis can be observed in the late stage of varicose veins complicated by frequent infections and worse clinical outcomes. Therefore, it is important to be aware of this condition and address it rather than overlook it.
Core Tip: Phlebosclerosis is a common age-related fibrotic degeneration of the venous wall, which is overlooked and little-known. It may cause venous dysfunction and lead to venous thrombosis. We report a 70-year-old man with phlebosclerosis, varicose veins, and vitiligo. During surgery, a rod-like calcified vein was discovered. Surprisingly, a wooden stick-like structure was retrieved from this thickened venous wall. Phlebosclerosis often exists in the late stages of varicose veins and complicates the clinical outcome. Therefore, we should be aware of this condition rather than overlooking it.
- Citation: Ren SY, Qian SY, Gao RD. Phlebosclerosis: An overlooked complication of varicose veins that affects clinical outcome: A case report. World J Clin Cases 2023; 11(35): 8404-8410
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8404.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8404
Phlebosclerosis is a common age-related fibrotic degeneration of the venous wall. While it is not a distinct disease entity, it may cause venous dysfunction and even phlebothrombosis[1-3]. Although phlebosclerosis is often found in non-varicose veins of elderly individuals, it is also found in idiopathic mesenteric phlebosclerosis and chronic venous disease, especially varicose veins[1,4-7].
Idiopathic mesenteric phlebosclerosis is a rare disease that is predominantly reported in East Asian countries. It mainly affects the right side of the colon. With an incidence rate of 0.01/100000 in Japan, its etiology remains unclear. However, it has been associated with long-term consumption of herbal medicine[4-7].
The manifestations of varicose veins can range from being asymptomatic and showing pigmentation to conditions such as ankle edema, ankle joint stiffness, periostitis, and leg ulcers[8,9]. Varicose veins are caused by venous valve incompetence and failure of the calf muscle pump, which gradually increases venous hypertension[9,10]. Venous hypertension causes tissue edema, hypoxia, stasis dermatitis, chronic inflammation, hypercoagulable state, and subsequent phlebosclerosis[11,12].
Although phlebosclerosis is rarely reported in patients with varicose veins[12], herein, we present a case of severe rod-like phlebosclerosis in a 70-year-old man with varicose veins and a venous skin ulcer.
A 70-year-old man presented with a 30-year history of varicose veins and vitiligo on both extremities. He also complained of recurrent skin infections and an ulcer on his left ankle for 3 years.
The blood pressure of the patient had been fluctuating around 160/110 mmHg for 3 years, which had been controlled with medication. In addition, about 1.5 years ago, he had occasionally consumed Chinese herbs containing astragalus, papaya, angelica, spatholoba, and cassia twig to relieve leg discomfort.
Constant discomfort accompanied by intermittent pain due to skin infection and ulcers over 3 years had prompted the patient to consult a doctor at a local hospital. However, his symptoms failed to resolve, prompting him to visit our hospital.
He denied having a history of smoking or alcohol consumption, and his family history was unremarkable.
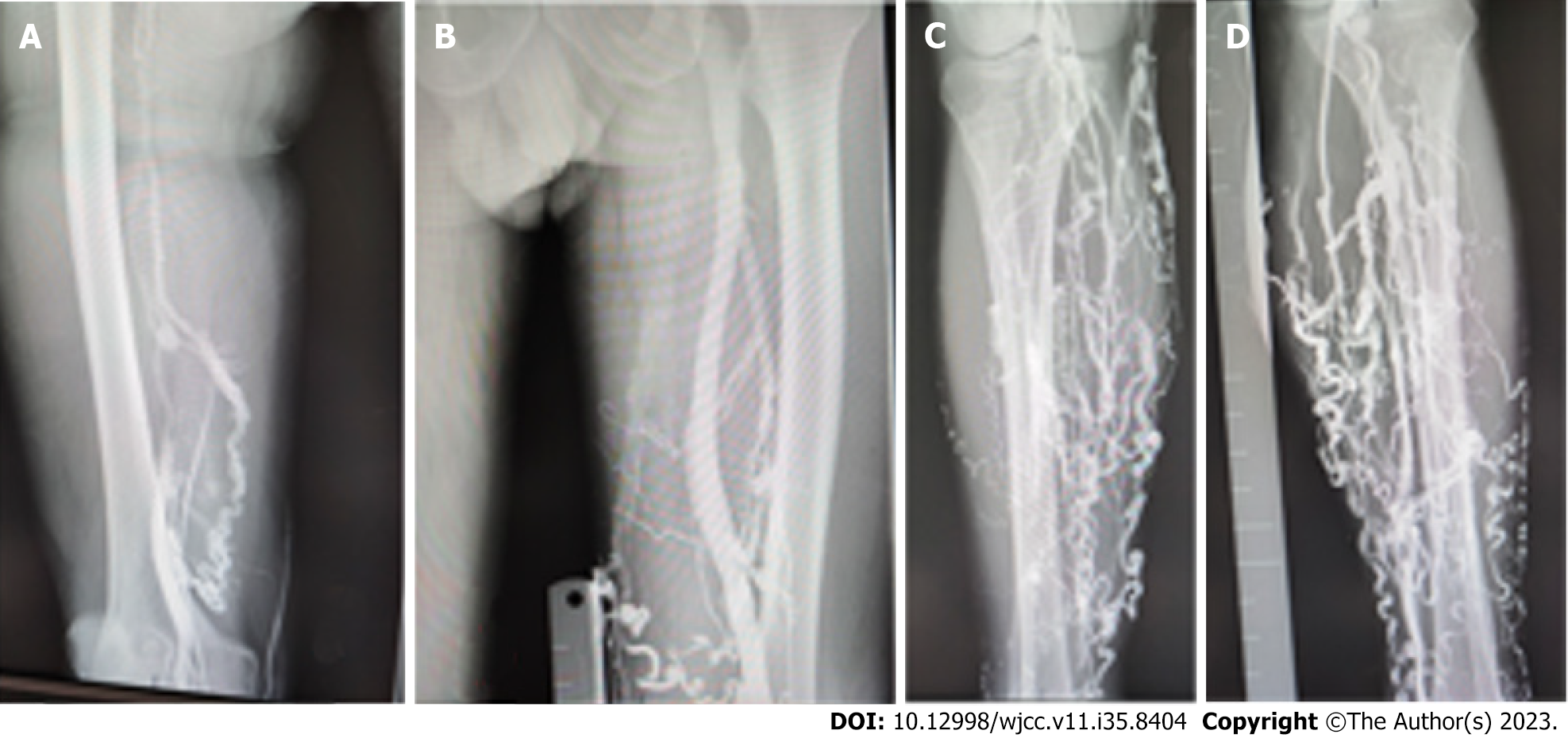
Physical examination on admission revealed obvious varicose veins on both lower extremities, which were palpated as hardened threads under the skin. An ulcer was located on the medial aspect of the left ankle (Figure 1). In addition, vitiligo was observed on both legs and the trunk (Figure 1). Venous angiography showed a tortuous varicose vein in the leg, with venous reflux to the level of the knee (Figure 2).
The patient was hospitalized for 10 d. Laboratory data showed that his white blood cell count ranged from 5.27 × 109/L to 11.7 × 109/L and neutrophil count ranged from 2.82 × 109/L to 7.34 × 109/L. His serum total protein measured 64.1 (normal range: 65-85) g/L, and his blood albumin level was 37 (normal range: 40-55) g/L.
Venous radiography revealed numerous dilated varicose veins and thrombus in the great saphenous veins (Figure 2).
The final diagnoses were hypertension, chronic venous dysfunction, varicose veins stage C6, vitiligo, skin infection, and venous ulcer.
The patient was treated surgically on April 18, 2023. Before surgery, he had provided written informed consent for surgical treatment and the possible publication of a case report in the future.
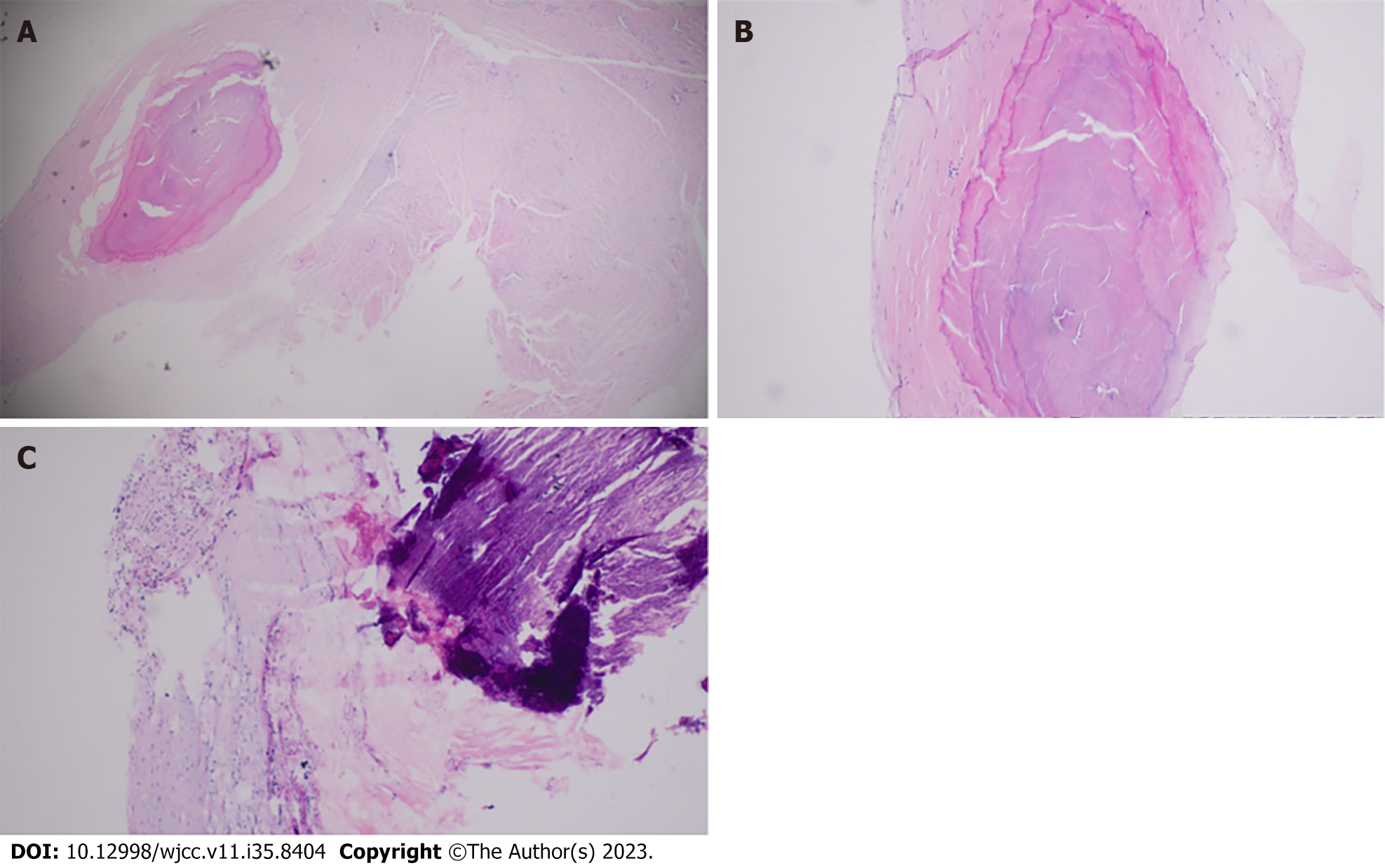
During surgery, the varicose veins that were removed were found to be hardened and tortuous, with thrombi blocking the venous lumen and fibrous tissue distributed along the entire length of the removed veins. The venous wall was thickened and the lumen was irregularly narrowed or even occluded (Figures 3 and 4). The calcified vein wall was as hard as a wooden stick or skeleton (Video).
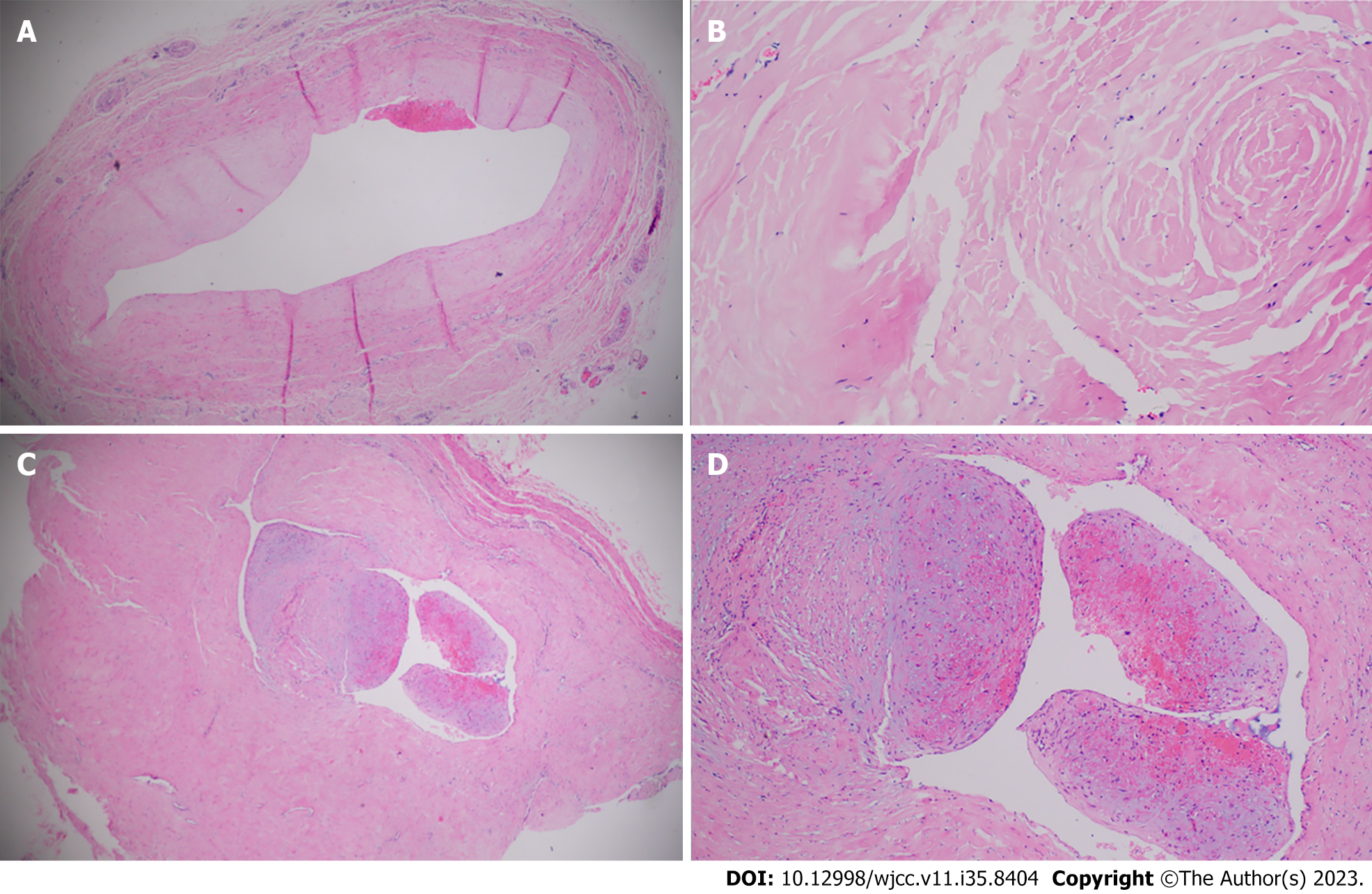
Pathologic examination revealed necrotic changes, erosion and ulceration of the vein, and hemorrhagic and edematous intima with inflammatory cell infiltration in the venous wall (Figures 5 and 6). There were numerous sclerotic veins with hyalinization, calcification, and areas of ossification. A focal area showed almost complete occlusion of the venous lumen with ossification and thrombosis. Hematoxylin and eosin staining revealed hyalinization, calcification, ossification, and thrombosis of the varicose veins. The intima of the venous wall was thickened, with parts of veins being closed due to hyperplasia and fibrosis (Figures 5 and 6). Microscopic examination showed fibrosis, thrombosis, and calcification in the resected varicose veins.
The patient was hospitalized for 10 d and recovered well. He resumed his normal daily life and showed no recurrent symptoms at the 6-mo follow-up after surgery. In addition, the venous ulcer on his ankle had healed (Figure 1C and D).
We found a rod-like phlebosclerosis of the venous wall in a 70-year-old patient with varicose veins and a venous ulcer. To our surprise, from the thickened vein wall, a structure resembling a tiny wood rod was obtained. At one point during the operation, we speculated that a wooden stick had been accidentally inserted into his leg during an unrecognized injury and penetrated into the venous wall. However, further careful study of the specimen dismissed our preliminary thought. We found that the venous wall was asymmetrically thickened. The entire varicose vein had hardened, and part of the venous lumen was either narrowed or completely closed. The cross-section of this wooden rod-like vein showed venous fibrosis and calcification, thickening of the venous wall, extensive collagen deposition on the venous wall, hyaline degeneration, and venous sclerosis causing closure of the venous lumen.
While phlebosclerosis of the superficial saphenous veins has been rarely described[1,2], after reviewing the literature, we believe that this is likely the first report of severe phlebosclerosis in a patient with varicose veins and a venous ulcer. The hardened venous wall was comparable to a wooden stick or skeleton. Our pathological study revealed that the phlebosclerosis had developed inside the asymmetrically thickened venous wall.
It has been reported that the calcification and ossification of the venous wall mainly involves the intima or an organized thrombus and does not involve the media and adventitia unlike arteriosclerosis, where the media is often calcified and ossified[2-4]. However, our findings in the present case show that ossification of the venous wall also involves the intimal layer and the media.
The cause of phlebosclerosis is not fully understood. Phlebosclerosis of superficial veins is less common than arteriosclerosis in elderly individuals, but phlebosclerosis of veins has been occasionally reported, such as idiopathic mesenteric phlebosclerosis in Asians, which has been associated with long-term use of herbal medicines containing geniposide and gardenia fruit[1-5]. Our patient had not consumed any herbal medicine containing these ingredients. Potential causes may be related to chronic venous disease, varicose veins, venous inflammation, and recurrent skin infections and ulcers. Phlebosclerosis is associated with age, venous insufficiency, and hemodialysis[4]. Chronic venous dysfunction, such as varicose veins, causes obstruction of venous blood flow and deterioration of venous function[6]. Gradual hyperplasia of the intima and muscle in the media of the vein leads to fibrosis, calcification, and deposition of collagen inside the venous wall, eventually causing phlebosclerosis[2,4,7,8].
Phlebosclerosis is a degenerative disease of the venous wall, which has often been overlooked in the literature owing to its uncertain clinical significance[8]. Its incidence is 1.5%-9.7% depending on the radiologic features, and the incidence of phlebosclerotic great saphenous vein was reported as 26.9%-91% according to histologic examination prior to its use as a vein graft[4]. The exact pathogenesis of phlebosclerosis is unclear. It occurs more frequently in the small saphenous vein than in the great saphenous vein, and more frequently in superficial veins than in deep veins[4]. It can be diagnosed on the basis of increased echogenicity and thickness or calcification of the vein wall by direct observation or pathological examination[4].
It has been reported that calcification and ossification of the venous wall predominantly involve the intima or an organized thrombus and not the media and adventitia as observed in arteriosclerosis[1,2]. This contradicts findings in arteries where calcification and ossification of the media are common. However, our findings in the present case show that ossification of the venous wall involves both the intimal layer and the media.
Most medical practitioners are familiar with arteriosclerosis, but phlebosclerosis is mostly overlooked or even unrecognized in clinical practice[1-4]. Our surgical observation showed that the features of phlebosclerosis are associated with venous fibrosis, hyalinization, sclerosis and calcifications, intimal ulceration, wall thickening, and luminal strictures. During surgery, a rod-like hardened vein was observed, which may have developed over the patient’s 30-year history of varicose veins. This case underscores the importance of recognizing and understanding the clinical significance of phlebosclerosis, similar to the importance given to arteriosclerosis.
| 1. | Tepelenis K, Papathanakos G, Kitsouli A, Barbouti A, Varvarousis DN, Kefalas AA, Anastasopoulos N, Paraskevas G, Kanavaros P. Prevalence and risk factors of phlebosclerosis in the great saphenous vein. Vascular. 2023;17085381231162134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 2. | Kitamura T, Kubo M, Nakanishi T, Fushimi H, Yoshikawa K, Taenaka N, Furukawa T, Tsujimura T, Kameyama M. Phlebosclerosis of the colon with positive anti-centromere antibody. Intern Med. 1999;38:416-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Leu HJ, Vogt M, Pfrunder H, Odermatt BF. Phlebosclerosis: disorder or disease? Vasa. 1991;20:230-236. [PubMed] |
| 4. | Wang J, Shao J, Lu H, Wang B, Chen J. Idiopathic mesenteric phlebosclerosis: one case report and systematic literature review of 240 cases. Am J Transl Res. 2021;13:13156-13166. [PubMed] |
| 5. | Hu YB, Hu ML, Ding J, Wang QY, Yang XY. Mesenteric phlebosclerosis with amyloidosis in association with the long-term use of medicinal liquor: A case report. World J Clin Cases. 2020;8:798-805. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Takahashi J, Miyakura Y, Maemoto R, Takayama N, Fukuda R, Tamaki S, Ishikawa H, Tsujinaka S, Lefor AK, Rikiyama T. Idiopathic mesenteric phlebosclerosis treated with laparoscopic subtotal colectomy: A case report. Asian J Endosc Surg. 2020;13:223-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Guo F, Zhou YF, Zhang F, Yuan F, Yuan YZ, Yao WY. Idiopathic mesenteric phlebosclerosis associated with long-term use of medical liquor: two case reports and literature review. World J Gastroenterol. 2014;20:5561-5566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 8. | Gao RD, Qian SY, Wang HH, Liu YS, Ren SY. Strategies and challenges in treatment of varicose veins and venous insufficiency. World J Clin Cases. 2022;10:5946-5956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (6)] |
| 9. | Sun Y, Li X, Chen Z, Ren S. Feasibility and safety of foam sclerotherapy followed by a multiple subcutaneously interrupt ligation under local anaesthesia for outpatients with varicose veins. Int J Surg. 2017;42:49-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Li X, Yang B, Li X, Ren S. Prospective Comparison of Effect of Ligation and Foam Sclerotherapy with Foam Sclerotherapy Alone for Varicose Veins. Ann Vasc Surg. 2018;49:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Langes K, Hort W. Intimal fibrosis (phlebosclerosis) in the saphenous vein of the lower limb: a quantitative analysis. Virchows Arch A Pathol Anat Histopathol. 1992;421:127-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Tepelenis K, Papathanakos G, Barbouti A, Paraskevas G, Kitsouli A, Alexandra Kefala M, Tepelenis N, Kanavaros P, Kitsoulis P. Phlebosclerosis in lower extremities veins - a systematic review. Vasa. 2020;49:349-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Inagawa Y, Japan S-Editor: Liu JH L-Editor: Filipodia P-Editor: Yu HG