Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8379
Peer-review started: August 31, 2023
First decision: October 9, 2023
Revised: November 4, 2023
Accepted: December 5, 2023
Article in press: December 5, 2023
Published online: December 16, 2023
Processing time: 104 Days and 20.4 Hours
Thyroid cancer is not commonly observed in patients with Graves’ disease (GD). The presence of thyroid nodules in GD is not uncommon. However, a link bet
A 26-year-old male patient with GD, receiving carbimazole for 2 years, presented to our hospital. His hyperthyroidism was controlled clinically and biochemically. On clinical examination, he was found to have a left-sided thyroid nodule. Ultra
Careful preoperative assessment and thyroid gland ultrasound might assist in screening and diagnosing thyroid cancer in patients with GD.
Core Tip: Thyroid cancer in male patients with Graves’ disease (GD) is rare. We report the first case of multifocal micropapillary thyroid cancer in a young male patient with GD in Saudi Arabia, which was detected by careful clinical examination followed by ultrasonographic evaluation of the nodule.
- Citation: Alzaman N. Multifocal papillary thyroid cancer in Graves’ disease: A case report. World J Clin Cases 2023; 11(35): 8379-8384
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8379.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8379
Thyroid-stimulating immunoglobulins (TSI) induce thyroid hormone overproduction in Graves’ disease (GD), the most common cause of hyperthyroidism. While GD is not generally considered a risk factor for developing thyroid cancer, which ranks as the eighth most prevalent cancer worldwide[1], other risk factors include childhood exposure to ionizing radiation and iodine deficiency[2].
Thyroid carcinoma in GD was initially regarded as an infrequent phenomenon. However, the prevalence of thyroid carcinoma in patients with GD has recently increased compared with that in the normal population[2,3].
The occurrence of thyroid nodules in patients with GD varies between 13% and 37%[4]. Some evidence suggests that individuals with autoimmune thyroid conditions face a higher risk of thyroid cancer due to elevated expression of bio
The prevalence of thyroid cancer among patients with GD in Saudi Arabia remains unknown. We report a case of multifocal papillary thyroid cancer in a young male who has been undergoing treatment for hyperthyroidism over the past 2 years.
Neck swelling.
A 26-year-old male patient was diagnosed with GD two years ago and had been undergoing treatment with carbimazole.
Initially, he was on a regimen of carbimazole 45 mg for one year. However, a few months before his current presentation, his dose was gradually reduced to 20 mg.
The patient denied any family history of malignant tumors.
During his recent clinical assessment, physical examination revealed an enlarged goiter and the presence of a palpable nodule in the left thyroid lobe. Concerns were raised about the progression of his GD and the development of this thyroid nodule.
Laboratory investigations yielded notable results: His thyroid-stimulating hormone (TSH) level was 0.27, while the free T4 level was 0.99. A significant elevation in TSI was also observed, measuring 4.91 IU/L (normal range < 1.7 IU/L).
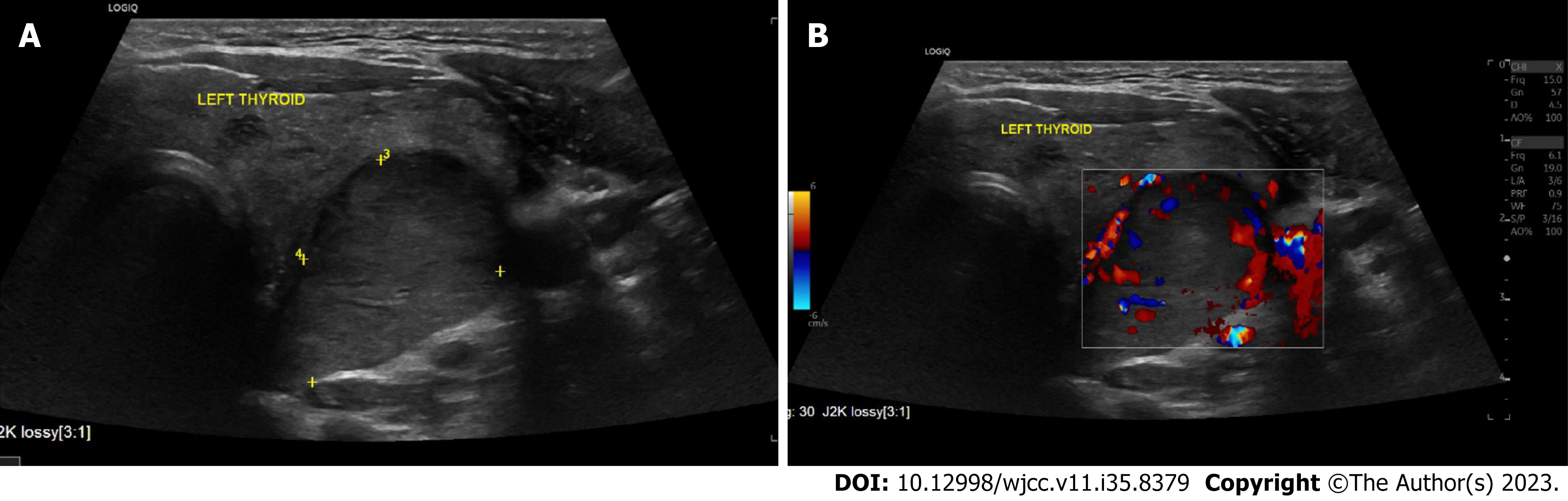
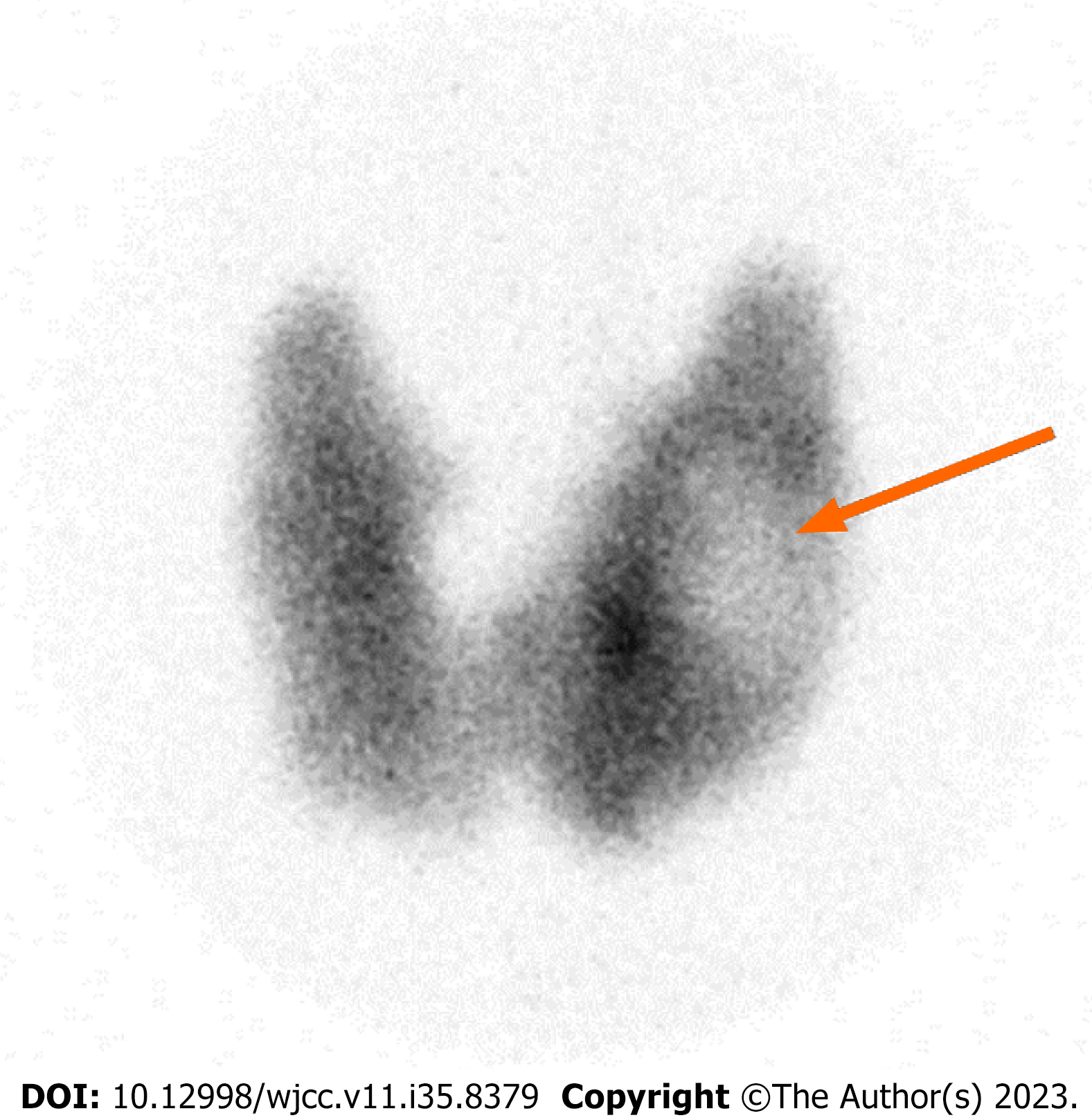
Further evaluation by thyroid ultrasound unveiled a distinct hypoechoic nodule located in the left thyroid lobe. This nodule measured 2.4 cm × 2.2 cm × 2.6 cm, displaying a smooth border and increased vascularity (Figure 1). The nodule was classified as TIRADS 4, indicating a high level of suspicion. To gain deeper insights, a nuclear scan utilizing tech
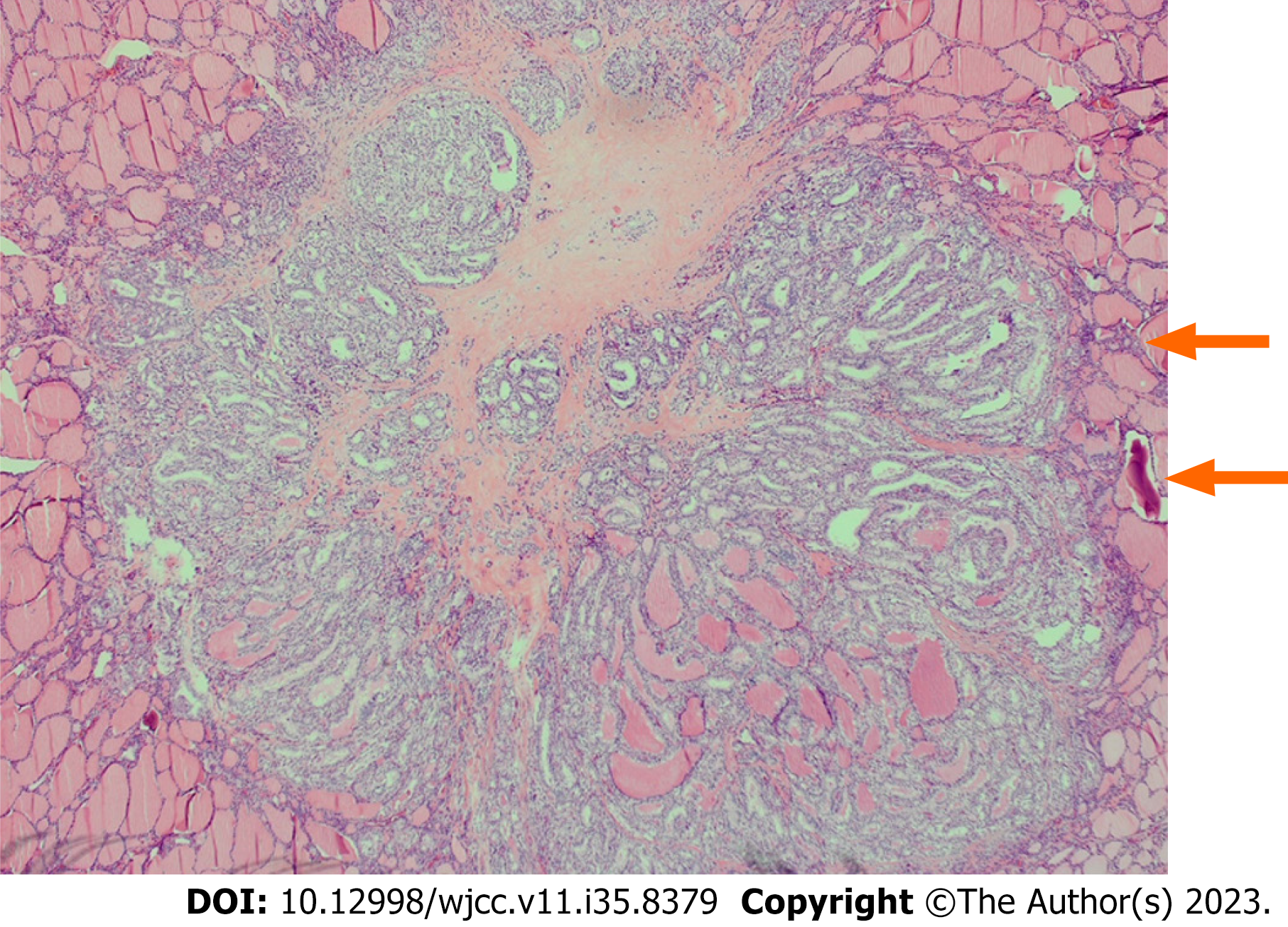
Fine needle aspiration cytology analysis was performed to characterize the nodule further. Clusters, papillae, and sheets of cells were observed, and their overlapping nuclear grooves hinted at features suggestive of papillary thyroid car
Multifocal classical papillary microcarcinoma in both thyroid lobes.
In light of these findings, a decision was made for the patient to undergo total thyroidectomy with lymph node dis
Following the surgery, the patient received radioactive iodine ablation therapy, with a dose of 102.53 mCi of radioactive Iodine-131. This multifaceted approach aimed to address both GD and the identified papillary thyroid carcinoma.
Historically, hyperthyroidism was considered protective against thyroid cancer due to suppressed TSH levels. Con
The American Thyroid Association recommends fine needle aspiration for nonfunctioning or hypofunctioning nodules identified through nuclear scans in patients with hyperthyroidism, as these nodules carry a higher risk of malignancy. Surgical intervention is advised for cases with suspicious or diagnostic cytopathology results[10].
Recent meta-analyses have revealed that the prevalence of thyroid carcinoma in GD is higher than global figures, with 10%-15% of GD-associated nodules reported to be thyroid cancers, predominantly papillary thyroid cancer[3]. This case report presents a young male with GD and a highly suspicious thyroid nodule. The results of fine needle aspiration biopsy were highly suggestive of papillary thyroid cancer. In addition, clinical examination and ultrasound were instrumental in identifying the nodule, and after total thyroidectomy, we established a definitive diagnosis of multifocal papillary microcarcinoma. Patients with multifocal papillary thyroid cancer have higher postoperative disease pro
Notably, research from the University of Chicago indicated that among patients with GD who underwent total thyroidectomy, 20% were diagnosed with both GD and thyroid cancer. These cases were primarily middle-aged females with positive TSI, and most of them presented with unifocal microcarcinomas[12]. Local data at Saudi Arabia showed that majority of patients with GD underwent total thyroidectomy because of failed antithyroid drugs and severe ophthalmopathy[13], while a retrospective study in Saudi Arabia demonstrated that only 5% of patients with thyroid cancer undergoing thyroidectomies were identified as hyperthyroid, with limited details regarding cancer characteristics[14].
The prognosis of thyroid cancer in patients with GD remains a topic of debate. While some studies suggest more aggressive behavior and higher recurrence rates[15,16], others find no significant differences in outcomes[17,18]. Moreover, conflicting findings exist, with certain studies reporting better prognosis and longer disease-free survival[19].
Recent umbrella reviews have incorporated both prospective and retrospective studies, revealing varying evidence regarding the risk of thyroid cancer in patients with GD. These reviews suggest a modest risk compared to patients with TMNG, while a stronger risk is observed in patients with GD with nodules compared to those without. Risk appears modest in patients with GD with solitary nodules compared to those with multiple nodules. In terms of recurrence, per
Thyroid cancer might not be promptly recognized in the context of GD. This case report underscores the importance of preoperative assessment, involving ultrasound, nuclear imaging, and fine needle aspiration, if necessary, to stratify cancer risk. Routine ultrasound is not typically recommended for GD evaluation, as a clinical presentation with suppressed TSH and elevated TSI is often deemed sufficient. Nonetheless, the coexistence of GD and thyroid cancer, albeit uncommon, underscores the necessity of vigilant evaluation, particularly in the presence of thyroid nodules.
This case sheds light on the evolving understanding of the coexistence of GD and thyroid cancer. The intricate relationship between these conditions challenges historical assumptions and emphasizes the need for careful evaluation in patients with GD with thyroid nodules. Based on this case, it is recommended to incorporate ultrasound and nuclear imaging, along with fine needle aspiration when appropriate, to assess malignancy risk. Clinicians should consider these measures for patients with GD and thyroid nodules to ensure timely detection and tailored management strategies. Further research could delve into the prevalence of thyroid cancer among patients with GD and explore the impact of various interventions on patient outcomes. Incorporating these insights into clinical practice will enable improved care for this unique subset of patients
| 1. | Dias Lopes NM, Mendonça Lens HH, Armani A, Marinello PC, Cecchini AL. Thyroid cancer and thyroid autoimmune disease: A review of molecular aspects and clinical outcomes. Pathol Res Pract. 2020;216:153098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 2. | Ferrari SM, Fallahi P, Elia G, Ragusa F, Ruffilli I, Paparo SR, Antonelli A. Thyroid autoimmune disorders and cancer. Semin Cancer Biol. 2020;64:135-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 130] [Article Influence: 21.7] [Reference Citation Analysis (1)] |
| 3. | Staniforth JUL, Erdirimanne S, Eslick GD. Thyroid carcinoma in Graves' disease: A meta-analysis. Int J Surg. 2016;27:118-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 4. | Mishra A, Mishra SK. Thyroid nodules in Graves' disease: implications in an endemically iodine deficient area. J Postgrad Med. 2001;47:244-247. [PubMed] |
| 5. | Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10769] [Cited by in RCA: 10257] [Article Influence: 1025.7] [Reference Citation Analysis (1)] |
| 6. | Means I. The thyroid and its diseases. Philadelphia: Lippincott, 1937. |
| 7. | Cappelli C, Braga M, De Martino E, Castellano M, Gandossi E, Agosti B, Cumetti D, Pirola I, Mattanza C, Cherubini L, Rosei EA. Outcome of patients surgically treated for various forms of hyperthyroidism with differentiated thyroid cancer: experience at an endocrine center in Italy. Surg Today. 2006;36:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Pazaitou-Panayiotou K, Perros P, Boudina M, Siardos G, Drimonitis A, Patakiouta F, Vainas I. Mortality from thyroid cancer in patients with hyperthyroidism: the Theagenion Cancer Hospital experience. Eur J Endocrinol. 2008;159:799-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Vaiana R, Cappelli C, Perini P, Pinelli D, Camoni G, Farfaglia R, Balzano R, Braga M. Hyperthyroidism and concurrent thyroid cancer. Tumori. 1999;85:247-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, Rivkees SA, Samuels M, Sosa JA, Stan MN, Walter MA. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. 2016;26:1343-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2006] [Cited by in RCA: 1623] [Article Influence: 162.3] [Reference Citation Analysis (0)] |
| 11. | Kuo SF, Lin SF, Chao TC, Hsueh C, Lin KJ, Lin JD. Prognosis of multifocal papillary thyroid carcinoma. Int J Endocrinol. 2013;2013:809382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Arosemena MA, Cipriani NA, Dumitrescu AM. Graves' disease and papillary thyroid carcinoma: case report and literature review of a single academic center. BMC Endocr Disord. 2022;22:199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Malabu UH, Alfadda A, Sulimani RA, Al-Rubeaan KA, Al-Ruhaily AD, Fouda MA, Al-Maatouq MA, El-Bakry AA. Surgical management of Graves' hyperthyroidism in Saudi Arabia: A retrospective hospital study. J Med Sci. 2007;7:1061-1064. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Doubi A, Al-Qannass A, Al-Angari SS, Al-Qahtani KH, Alessa M, Al-Dhahri S. Trends in thyroid carcinoma among thyroidectomy patients: a 12-year multicenter study. Ann Saudi Med. 2019;39:345-349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Ozaki O, Ito K, Kobayashi K, Toshima K, Iwasaki H, Yashiro T. Thyroid carcinoma in Graves' disease. World J Surg. 1990;14:437-40; discussion 440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 79] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Menon R, Nair CG, Babu M, Jacob P, Krishna GP. The Outcome of Papillary Thyroid Cancer Associated with Graves' Disease: A Case Control Study. J Thyroid Res. 2018;2018:8253094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Kasuga Y, Sugenoya A, Kobayashi S, Masuda H, Iida F. The outcome of patients with thyroid carcinoma and Graves' disease. Surg Today. 1993;23:9-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Hales IB, McElduff A, Crummer P, Clifton-Bligh P, Delbridge L, Hoschl R, Poole A, Reeve TS, Wilmshurst E, Wiseman J. Does Graves' disease or thyrotoxicosis affect the prognosis of thyroid cancer. J Clin Endocrinol Metab. 1992;75:886-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Kikuchi S, Noguchi S, Yamashita H, Uchino S, Kawamoto H. Prognosis of small thyroid cancer in patients with Graves' disease. Br J Surg. 2006;93:434-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Palella M, Giustolisi FM, Modica Fiascaro A, Fichera M, Palmieri A, Cannarella R, Calogero AE, Ferrante M, Fiore M. Risk and Prognosis of Thyroid Cancer in Patients with Graves' Disease: An Umbrella Review. Cancers (Basel). 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He XH, China S-Editor: Liu JH L-Editor: A P-Editor: Xu ZH