Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8228
Peer-review started: October 10, 2023
First decision: November 22, 2023
Revised: November 24, 2023
Accepted: November 28, 2023
Article in press: November 28, 2023
Published online: December 6, 2023
Processing time: 57 Days and 3.1 Hours
Snapping triceps syndrome (STS) is a rare disease, while occurrence of bilateral STS is extremely rare. It is usually accompanied by dislocation of the ulnar nerve and double snapping is a clinically important feature. However, to the best of our knowledge, there has been no report of bilateral STS in young active patient.
A 23-year-old male presented with a complaint of discomfort and snapping on the medial side of both elbows while performing push-ups. On physical examination, two distinct snaps that were both palpable and audible were detected on additional clinical examination. Dynamic ultrasonography showed that the ulnar nerve and the medial head of the triceps were dislocated anteriorly over the medial epicondyle of the elbow during flexion motion. Finally, he was diagnosed as dislocation of the ulnar nerve and STS. Staged anterior subcutaneous tran
STS should be included in the differential diagnosis for active young patients who present with painful snapping on the medial side of the elbow joint, particularly when dislocation of the ulnar nerve is detected. Dynamic sonography is used to assist in accurate diagnosis and differentiation between isolated dislocation of the ulnar nerve and STS.
Core Tip: Snapping triceps syndrome (STS) is a rare disease, while occurrence of bilateral STS is extremely rare. It is usually accompanied by dislocation of the ulnar nerve and double snapping is a clinically important feature. Dislocation of the ulnar nerve typically occurs first, at approximately 70 to 90 degrees of elbow flexion, followed by dislocation of the triceps at approximately 100 to 110 degrees of elbow flexion. Dynamic sonography is used to assist in accurate diagnosis and differentiation. Here we reported on the case of a patient who underwent surgery for treatment of bilateral STS.
- Citation: Cho CH, Lim KH, Kim DH. Bilateral snapping triceps syndrome: A case report. World J Clin Cases 2023; 11(34): 8228-8234
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8228.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8228
Snapping triceps syndrome (STS), a relatively rare disease, was first described by Rolfsen in 1970. It is defined as a dynamic phenomenon involving dislocation of the distal portion of the triceps over the medial epicondyle of the elbow[1-3]. Risk factors include cubital valgus or varus, hypertrophy or prominence of the distal triceps muscle, or accessory head of the triceps. STS is more common in abnormal triceps position as well as individuals who perform manual work related to hypertrophy of the triceps muscle through training[4,5]. Movement of the bulked medial triceps is more medial, which causes translocation (snapping) of a portion of the triceps over the medial epicondyle with flexion of the elbow[4].
Patients usually complain of local tenderness and a snapping sensation or sound around the medial side of the elbow. Because the condition usually involves coexistence with ulnar nerve dislocation, neuropathy of the ulnar nerve may also be observed. Two distinct snapping sounds can be detected in patients with typical STS. Dislocation of the ulnar nerve typically occurs first, at approximately 70 to 90 degrees of elbow flexion, followed by dislocation of the triceps at approximately 100 to 110 degrees of elbow flexion[6]. Confirmation of two characteristic snapping sounds around the medial side of the elbow during flexion is important. Recently, dynamic sonography is used to assist in accurate diagnosis and differentiation from diseases around elbow[7-11].
To the best of our knowledge, no previous cases of bilateral STS have been reported. Here we reported on the case of a patient who underwent surgery for treatment of bilateral STS.
A 23-year-old male, an amateur bodybuilder, presented with a complaint of discomfort and snapping on the medial side of both elbows while performing push-ups for three years.
His symptoms had worsened over the past two months. The pain, along with the snapping sound, then became constant with development of an intermittent tingling sensation on the ulnar side forearm and 5th finger area. In particular, the symptoms were aggravated by both resisted elbow flexion and resisted elbow extension.
Because he primarily regarded his symptoms as an inconvenience, he did not undergo treatment.
The patient was a college student with no history of elbow surgery, and there was no history of trauma or sport injury as well. There was no other past illness or family history.
On physical examination, tenderness over the medial epicondyle of the elbow was not observed and there were no clinical findings indicative of ulnar nerve compression. Two distinct snaps that were both palpable and audible were detected on additional clinical examination. The first snap had developed at approximately 90 degrees of elbow flexion and the second snap had developed at above 100 degrees of elbow flexion.
The results of preoperative laboratory tests were normal.
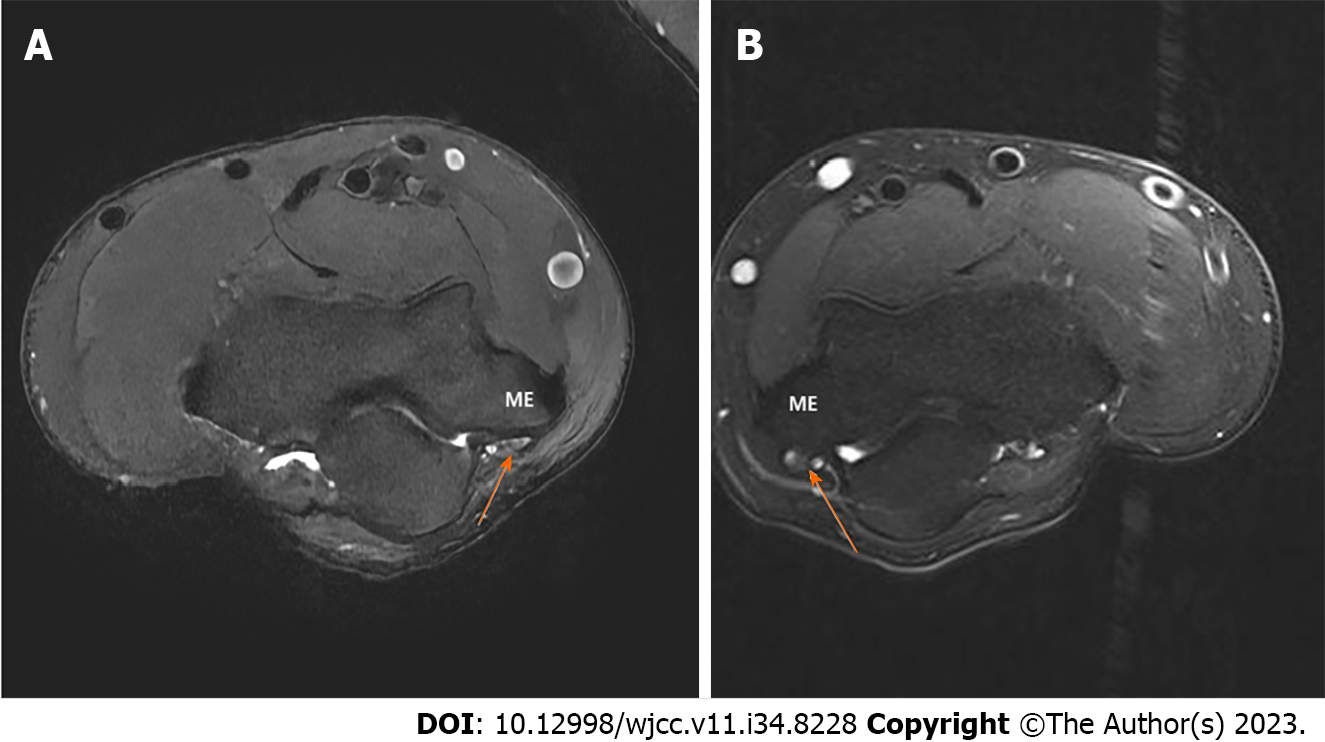
No bony abnormality such as cubitus varus or valgus was observed on the plain radiographs. A T2-weighted magnetic resonance image (MRI) showed a high signal change and swelling of the ulnar nerve (Figure 1). Dynamic ultrasonography showed that the ulnar nerve was dislocated anteriorly over the medial epicondyle of the elbow in flexion of the elbow by 90 degrees and the medial head of the triceps was also dislocated anteriorly over the medial epicondyle in flexion of the elbow by 100 degrees (Figure 2).
The final diagnosis of the presented case was bilateral STS of elbow joints.
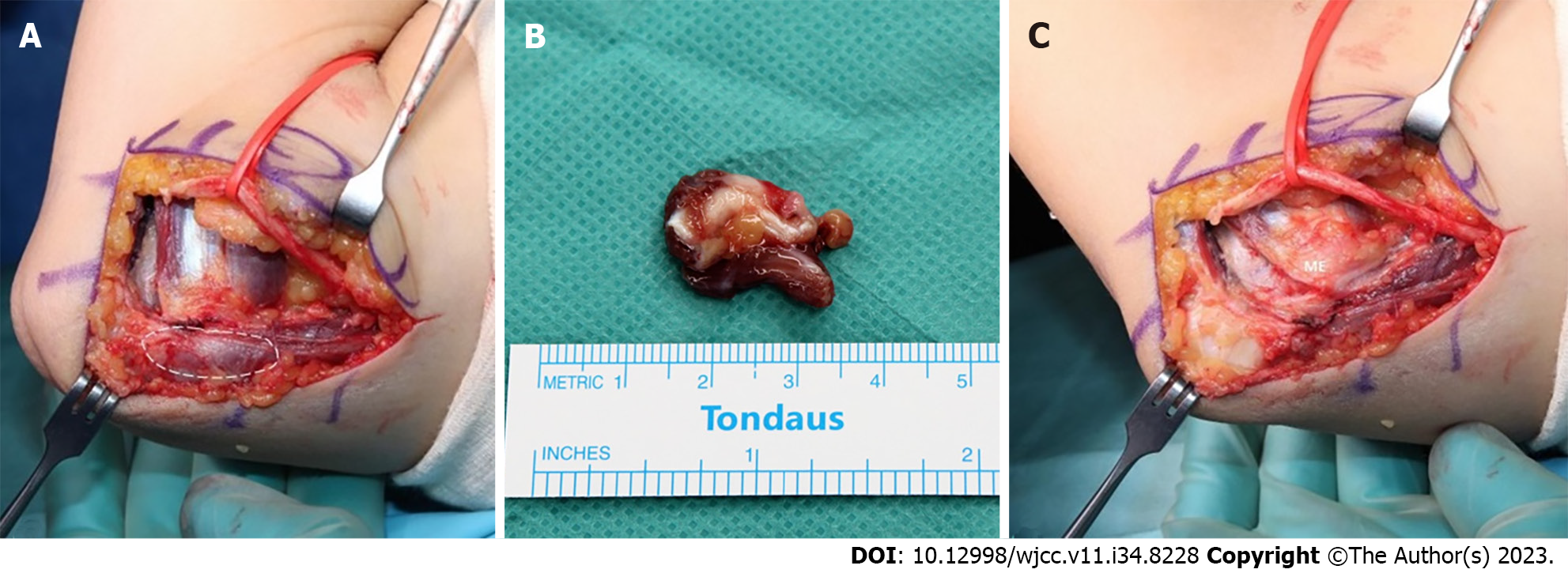
Conservative treatment was initially considered. However, the patient was an amateur bodybuilder who usually participated in several sports activities, and he wanted to anticipate returning to participation in sports as soon as possible. Therefore, surgery on the left elbow, which showed more severe symptoms, was planned. Anterior subcutaneous transposition of the ulnar nerve combined with partial resection of the snapping portion of the triceps was our surgical treatment of choice. After inflating a tourniquet, an 8 cm incision was made from 4 cm proximal to 4 cm distal of the medial epicondyle. During performance of the subcutaneous dissection, the medial antebrachial cutaneous nerve was located, and care was taken to avoid damaging it. The ulnar nerve was thickened and dislocated from the posterior to the anterior of the medial epicondyle with flexion of the elbow by 90 degrees (Figure 3). Neurolysis was performed using a vessel loop and the ulnar nerve was mobilized sufficiently to transpose it anteriorly without tension. With further flexion of the elbow, the leading edge of the medial head of the triceps was dislocated over the medial epicondyle. The minimum extent of the dislocated medial head of the triceps was measured by repeat passive flexion of the elbow and the medial head of the triceps, and was located over the medial epicondyle, was resected (Figure 4). After resection, it was confirmed that flexion of the elbow did not cause any dislocation of the triceps. Hemostasis was performed after the tourniquet was delated. Postoperatively, passive motion was subsequently initiated as pain permitted. Active mobilization was allowed after one week and no snap was observed on physical examination. He had no complaint of discomfort after three months of follow up, therefore, surgery on the right elbow was planned. The surgical method was the same as that used for the left side. The ulnar nerve was also thickened and dislocated from the posterior to the anterior of the medial epicondyle with flexion of the elbow by 80 degrees. After dissection and mobilization of the anterior of the ulnar nerve, the bulked-leading edge of the medial head of the triceps was also dislocated over the medial epicondyle with further flexion of the elbow (Figure 5) (Video 1). The minimum extent of the dislocated medial head of the triceps was measured by repeat passive flexion of the elbow and the medial head of the triceps, measuring 3 cm, located over the medial epicondyle, was resected. After resection, anterior transposition of the ulnar nerve was performed (Figure 6).
The patient’s pain and snapping symptoms showed significant improvement after surgery. Dynamic ultrasonography showed that the ulnar nerve and triceps were not dislocated during flexion and extension of the elbow at six weeks postoperatively. Three months later, the patient was completely asymptomatic and returned to participation in sports. And during the one-year follow-up, there were no symptoms in both elbows.
This case involves a rare disorder with STS in a bilateral elbow joint. STS with dislocation of the ulnar nerve can be easily overlooked when dislocation of the ulnar nerve and triceps occurs simultaneously at a similar angle during flexion of the elbow, resulting in detection of only one snapping sound, or when the second snapping sound is missed on physical examination. In particular, in cases where this disease is not considered, it is often misdiagnosed as isolated dislocation of the ulnar nerve.
Isolated dislocation of the ulnar nerve is relatively common, occurring in approximately 16.2% of healthy adults (subluxation: 12%, complete dislocation: 4%)[12] Causes include congenital general laxity, hypoplasia of the trochlea, and dislocation of the medial head of the triceps with or without cubitus varus/valgus deformity[13-15]. Also, several authors insisted that cubitus varus or valgus, fourth muscular head of the triceps, or accessory triceps tendon and hypertrophy of the medial head of the triceps are risk factors for STS[14-16]. However, in our case, there were no risk factors such as congenital general laxity, bony abnormalities or anatomical variances of the triceps were detected. The patient had performed several strengthening exercises, thus the bulk of the triceps could be confirmed. Therefore, we considered that the bulk of the medial head of the triceps may have caused STS.
MRI or dynamic ultrasound can assist in the diagnosis of snapping triceps syndrome. Although MRI can enable accurate identification of anatomical structures of the elbow joint, there is limitation in identifying dislocation or subluxation of the ulnar nerve and triceps. Therefore, dynamic ultrasound is more useful for diagnosis of STS than MRI[7]. However, in cases where dislocation of the ulnar nerve and the medial head of the triceps occurs at a similar degree, diagnosis of snapping triceps syndrome may not be easy. Careful physical assessment is important during repetition of flexion and extension of the elbow in order to determine whether it is isolated dislocation of the ulnar nerve or STS. The ulnar nerve dislocated at 90 degrees and the medial head of the triceps dislocated at approximately 120 degrees[17].
Surgical options include partial resection of the snapping slip, centralization or lateralization of the medial triceps of the triceps, medial condylotomy or corrective osteotomy, addressing humeral malignment[18]. Centralization or lateralization involves detaching the tendon of the medial head of the olecranon and passing it under, interlacing it with the central tendon or lateral tendon. This procedure is typically chosen in cases where the segment of snapping triceps represents a significant bulk of the medial head[19]. Partial resection of a snapping slip is chosen in select cases with small dislocating segments and easier and more rapid recovery can be expected; most studies have reported excellent results[18]. In our case, the snapping slip was not large in size, therefore, partial triceps resection was selected. Care should be taken not to resect an excessive amount of tendon, with the aim of not compromising the triceps function.
A limitation of this case was that preoperative nerve conduction velocity-electromyography was not performed. Because, on the preoperative physical examination, two snapping sounds were detected during flexion of the elbow and only a tingling sensation of the ulnar side of the hand without weakness was observed.
STS should be included in the differential diagnosis for active young patients who present with painful snapping on the medial side of the elbow joint, particularly when dislocation of the ulnar nerve is detected. Dynamic sonography is used to assist in accurate diagnosis and differentiation between isolated dislocation of the ulnar nerve and STS.
The authors thank Eun-Ji Jeon for her support.
| 1. | Hayashi Y, Kojima T, Kohno T. A case of cubital tunnel syndrome caused by the snapping of the medial head of the triceps brachii muscle. J Hand Surg Am. 1984;9A:96-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Rolfsen L. Snapping triceps tendon with ulnar neuritis. Report on a case. Acta Orthop Scand. 1970;41:74-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 45] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Dreyfuss U, Kessler I. Snapping elbow due to dislocation of the medial head of the triceps. A report of two cases. J Bone Joint Surg Br. 1978;60:56-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 41] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Boon AJ, Spinner RJ, Bernhardt KA, Ross SR, Kaufman KR. Muscle activation patterns in snapping triceps syndrome. Arch Phys Med Rehabil. 2007;88:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 5. | Kim J-H, Cho C-H, Koo T-W, Kim D-H. Misdiagnosed Snapping Triceps Syndrome on Ulnar Nerve Dislocation. J Korean Orthop Assoc. 2023;58:73-77. [DOI] [Full Text] |
| 6. | Vanhees MKD, Geurts GFAE, Van Riet RP. Snapping triceps syndrome: a review of the literature. Shoulder Elbow. 2010;2:30-33. [DOI] [Full Text] |
| 7. | Jeong WK, Park SW, Song DI, Lee SH. Snapping Triceps Syndrome with Dislocation of the Ulnar Nerve-Usefulness of Dynamic Ultrasonography. J Korean Orthop Ultrasound Soc. 2008;1:27-30. |
| 8. | Daliri M, Ebrahimnejad M, Najafi S, Aminzadeh B, Emadzadeh M, Moradi E, Moradi A. Magnetic Resonance Imaging and Sonographic Features before and after Surgery in Carpal Tunnel Syndrome: Association with Clinical Findings. Clin Orthop Surg. 2022;14:603-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Shim JW, Jeon N, Jang MC, Park MJ. Clinical Outcomes of Arthroscopic Debridement for Lateral Epicondylitis with Partial Injury of the Lateral Collateral Ligament Complex. Clin Orthop Surg. 2022;14:434-440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Shin W, Kang T, Han J. Cubital tunnel syndrome associated with previous ganglion cyst excision in the elbow: a case report. Clin Shoulder Elb. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 11. | Colasanti CA, Boin M, Hacquebord J, Virk M. Anterior interosseous nerve palsy in the early postoperative period after open capsular release for elbow stiffness. Clin Shoulder Elb. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 12. | Childress HM. Recurrent ulnar-nerve dislocation at the elbow. Clin Orthop Relat Res. 1975;168-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 142] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Bjerre JJ, Johannsen FE, Rathcke M, Krogsgaard MR. Snapping elbow-A guide to diagnosis and treatment. World J Orthop. 2018;9:65-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 14. | Pfister G, Barbier O, Ollat D. "Snapping triceps": A rare and misleading condition - a clinical case report. Hand Surg Rehabil. 2018;37:121-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Fabrizio PA, Clemente FR. Variation in the triceps brachii muscle: a fourth muscular head. Clin Anat. 1997;10:259-263. [PubMed] [DOI] [Full Text] |
| 16. | Satteson ES, Li Z. Anteriorly positioned ulnar nerve at the elbow: a rare anatomical event: case report. J Hand Surg Am. 2015;40:984-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Spinner RJ, Goldner RD. Snapping of the medial head of the triceps and recurrent dislocation of the ulnar nerve. Anatomical and dynamic factors. J Bone Joint Surg Am. 1998;80:239-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 105] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Imao K, Miwa H, Tsubokawa N, Maki Y, Endo N. Dislocation of the Medial Head of the Triceps With Ulnar Nerve Location Anterior to the Medial Epicondyle. J Hand Surg Am. 2020;45:72.e1-72.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Spinner RJ, O'Driscoll SW, Jupiter JB, Goldner RD. Unrecognized dislocation of the medial portion of the triceps: another cause of failed ulnar nerve transposition. J Neurosurg. 2000;92:52-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lv L, China S-Editor: Liu JH L-Editor: A P-Editor: Yu HG