Published online Nov 26, 2023. doi: 10.12998/wjcc.v11.i33.7943
Peer-review started: September 7, 2023
First decision: September 20, 2023
Revised: September 27, 2023
Accepted: November 16, 2023
Article in press: November 16, 2023
Published online: November 26, 2023
Processing time: 78 Days and 6.2 Hours
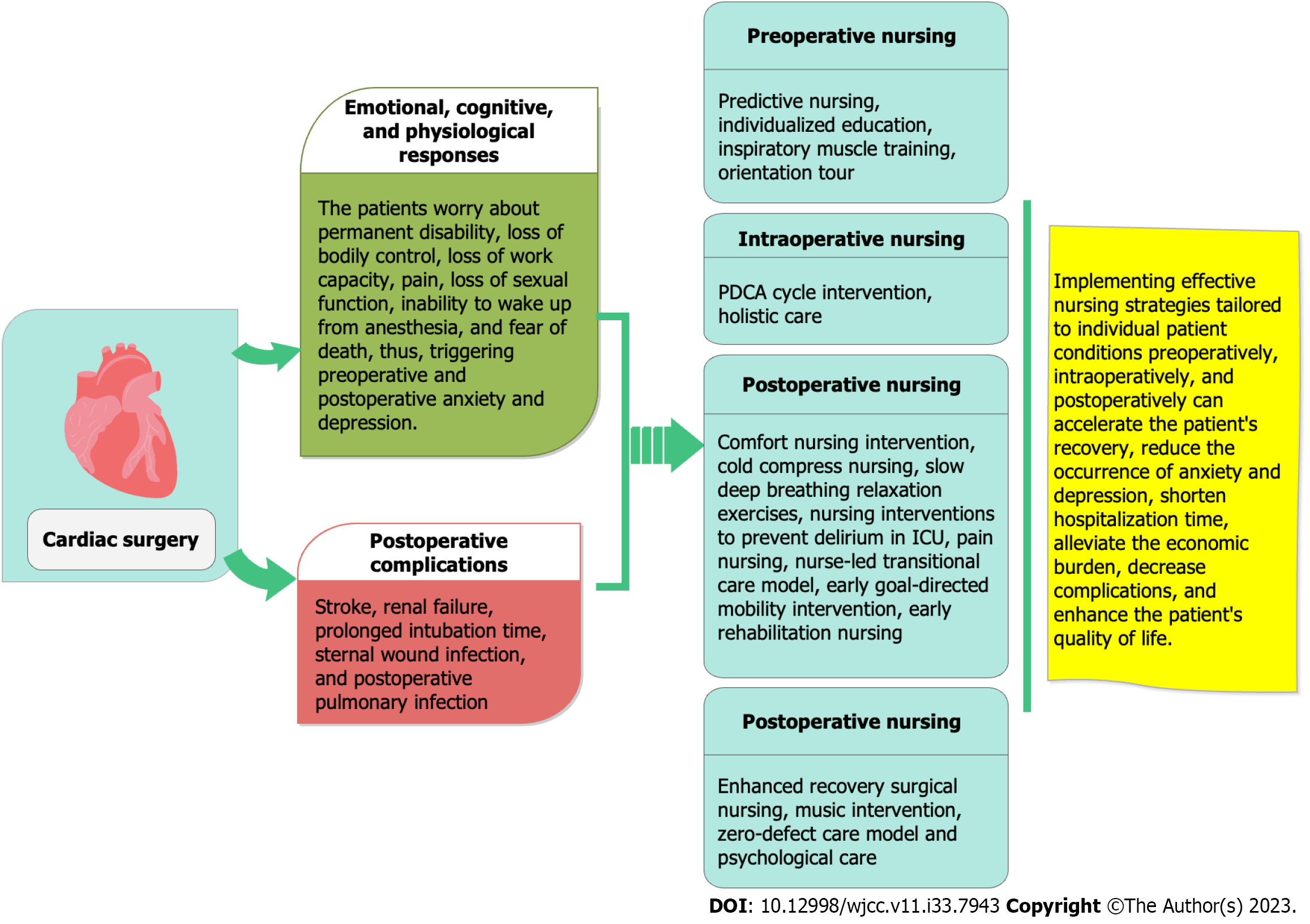
As a stressor, cardiac surgery affects the physiology and psychology of patients, as well as their postoperative recovery. Patients tend to worry about cognitive deficiency, pain, discomfort, the risk of death, sleep, complications, and other factors, resulting in stress and anxiety. Moreover, serious adverse events, such as circulatory and respiratory dysfunction and infection, tend to occur after cardiac surgery and increase the economic burden on patients. Therefore, appropriate nursing interventions should be selected to strengthen patients’ cognitive levels, compliance, and postoperative practices to accelerate their recovery, reduce complications, and shorten hospital stays so as to contribute to patients’ lives and health.
Core Tip: Surgery can extend the life of patients with heart diseases (such as congenital and coronary heart diseases) and improve their quality of life. However, it can trigger emotional, cognitive, and physiological responses in patients, leading to fear and anxiety regarding mortality and even depression. Through nursing interventions, we can strengthen patients' cognitive abilities, compliance, and postoperative recovery, thereby reducing complications, shortening hospital stays, and providing importance for patients' overall health and well-being.
- Citation: Wang SR, Zhou K, Zhang W. Application progress of nursing intervention in cardiac surgery. World J Clin Cases 2023; 11(33): 7943-7950
- URL: https://www.wjgnet.com/2307-8960/full/v11/i33/7943.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i33.7943
Cardiovascular disease (CVD) is the world’s deadliest disease. According to a report by the World Health Organization, more than 23 million people will die of CVD every year by 2030. This situation is not optimistic, and surgical treatment plays an important role in prolonging and improving the quality of life of patients with heart disease[1,2]. Cardiac surgery is often used to treat valvular heart disease, congenital heart disease, coronary heart disease, and other heart diseases. It is characterized by complicated steps, high risk, great difficulty, and a lengthy postoperative recovery period[3], all of which can cause emotional, cognitive, and physiological reactions. Patients undergoing surgery often experience anxiety and even depression from fears regarding permanent disability, loss of physical control, loss of the ability to work, pain, loss of sexual ability, the inability to awaken from anesthesia, and death[2,4-6]. One study reported that 34% of patients undergoing cardiac surgery experienced preoperative anxiety, 24.7% experienced postoperative anxiety, and 16.5% experienced both preoperative and postoperative anxiety[7].
Postoperative complications can easily occur, with an incidence rate ranging from 15% to 30%. Possible complications include the following: Stroke, renal failure, prolonged intubation time, sternal wound infection[8,9], and postoperative pulmonary infections (e.g., atelectasis, pleural effusion, pneumonia, pulmonary edema, cardiogenic pulmonary edema, acute respiratory distress syndrome, pulmonary embolism, phrenic nerve injury, pneumothorax, and mediastinitis)[10]. In view of the serious nature of cardiac surgery, the study objective was to summarize applicable preoperative, intraoperative, postoperative, and perioperative nursing intervention methods to provide a reference for clinical practice. The information conveyed is vitally important for improving the health and quality of life of patients (Figure 1).
Postoperative pneumonia is one of the most common complications after cardiac surgery and it can increase the morbidity, mortality, and health care burden of patients. Bardia et al[11] guided 1125 patients undergoing cardiac surgery to use a chlorhexidine mouthwash before surgery and found that the risk of postoperative pneumonia was reduced by approximately half[11].
Individualized care is defined as reducing patients’ anxiety according to their beliefs, values, emotions, thoughts, preferences, personal experiences, and opinions[12]. Ertürk and Ünlü[13] identified the source of anxiety in 300 patients undergoing cardiac surgery and provided preoperative individualized care for 30-90 min. They found that the main sources of preoperative anxiety were a lack of knowledge, distance from family, the risk of death, and pain. A total of 95.4% of patients were satisfied with the preoperative education, and they could quickly adapt to the intensive care unit (ICU) environment and perform guided breathing and coughing exercises following surgery.
In their study, Chen et al[14] selected 197 patients over age 50 who had undergone cardiac surgery and received five days of respiratory muscle training before surgery. The results of the training showed that the postoperative respiratory muscle strength of these patients was substantially enhanced, and the incidence of postoperative pulmonary complications and a lengthy hospital stay were reduced[14].
For their study, Niknejad et al[15] selected 70 patients scheduled for coronary artery bypass grafting. They learned about the procedure one day before surgery and were shown around the hospital for 40 min by an anesthesia technician, a nurse, and a researcher. The tour included a 10-min visit to an unattended operating room during the night shift, a 5-min visit to an ICU, a 10-min visit to an operating room to familiarize themselves with personnel who could answer questions about surgery, and a 15-min conversation with inpatients. Findings showed that the anxiety levels of the patients decreased after the orientation tour.
The operating room is the most important place for patients, as it is the location where they undergo surgery. Owing to the variability and high risk of the work in this environment, operating rooms have higher requirements for nursing quality[16]. Du et al[17] adopted the Plan-Do-Check-Act (PDCA) cycle management method to continuously improve the quality of cardiac surgery preparation time by identifying the causes of illness, developing countermeasures, eliminating hidden dangers, and optimizing workflow to ensure smooth Surgeries.
Khajian Gelogahi et al[18] selected 80 patients undergoing coronary artery bypass surgery and provided each one with four 30- to 45-min individual sessions of intentional nursing presence during surgery. The results showed that conscious nursing arrangements were an effective way to relieve depression, stress, and anxiety in patients undergoing surgery.
Complications after cardiac surgery, such as pain, mental distress, and hemodynamic instability, have multiple negative effects on children and surgical outcomes. Comfort theory is a comprehensive, descriptive nursing theory that can be used as a guide for patients requiring holistic care. Nurses implement three levels of comfort measures (relief, ease, and transcendence) from four dimensions: Body, psychology, social culture, and the environment. Khaleghi et al[19] selected 60 infants aged 28 d to 2 years and collected demographic details, information regarding comfort behavior, hemodynamic parameters, and other data, and carried out a comfort nursing intervention. This approach can significantly improve a patient’s postoperative pain, as well as respiration and heart rate.
Chest tube placement is necessary in all types of cardiac surgery to maintain cardiopulmonary function and prevent pneumothorax, hemothorax, and pleural effusion. Generally, the tube should be removed within 24-48 h after cardiac surgery, but removal of the chest tube can cause patients to experience considerable pain. Mohammadi et al[20] used cold compresses to relieve the pain caused by chest tube removal after cardiac surgery and found that their use could significantly reduce the pain severity score. However, the effect was not significant 15 min after removal[20].
Jarrah et al[21] guided 25 patients undergoing coronary artery bypass transplantation to perform slow deep breathing relaxation exercises before chest tube extraction (after surgery) and found that their pain levels decreased significantly 5 and 15 min after extubation. Thus, slow deep breathing relaxation exercises can be used effectively to relieve pain during chest tube extubation and minimize related side effects and the need for analgesics.
Postoperative delirium is a state of acute brain dysfunction following anesthesia and surgery[22]; it occurs in 25%-52% of patients undergoing cardiac surgery and is associated with increased mortality, a prolonged hospital stay, and long-term cognitive decline[23]. From a literature review, Pieri et al[24] concluded that the most commonly used strategies for preventing postoperative delirium are therapies involving dexmedetomidine, ketamine, antipsychotics, glucocorticoids, propofol, opioids, volatile anesthetics, local anesthetics, and remote ischemic preconditioning, among which dexmedetomidine is the most promising measure. The nUrsiNg DEliRium Preventive INterventions in the ICU (UNDERPIN-ICU) is a nurse-oriented intervention to prevent delirium developed for the main risk factors, such as visual and auditory disorders, sleep disorders, cognitive disorders, and activity disorders[25]. Song et al[26] established a delirium research group to develop UNDERPIN-ICU for cardiac surgery and trained nurses for two months to implement it with patients undergoing cardiac surgery. The results pointed to the effectiveness of this program in preventing or reducing the incidence of postoperative delirium following cardiac surgery and shortening the duration of mechanical ventilation and length of the ICU stay.
Doğan and Saritaş[27] applied the new behavioral formation technique of neuro-linguistic programming (NLP) and the guided imagination relaxation technique using a 30-min audio CD for patients undergoing cardiac surgery. Consequently, the postoperative pain level of patients in the NLP group decreased significantly, and the comfort level of patients in the guided imagination group increased substantially. Luque Oliveros and Morilla Romero de la Osa[28] applied 0.5% bupivacaine to 69 patients in order to infiltrate their surgical wounds within 12 h after cardiac surgery, and the results showed that this practice could relieve pain considerably and effectively.
Coskun and Duygulu[29] adopted a nurse-led transitional care model to carry out a transitional nursing program nine weeks after 33 elderly patients were discharged following cardiac surgery. The authors found that the functional autonomous measurement system and quality of life scores of these patients improved significantly, and readmission and rehospitalization rates decreased substantially.
In Early goal-directed therapy (EGDT), a team of medical staff and rehabilitation technicians develops a humanized, feasible, and progressive rehabilitation plan for patients undergoing cardiac surgery. Lin et al[30] evaluated 60 cardiac surgery patients attended to by an EGDT team and formulated and implemented an accurate and effective personalized EGDT plan. They found that this method could shorten the indwelling time of endotracheal intubation and the length of stay in the ICU, reduce the occurrence of complications, and improve patient satisfaction[30].
Cardiac surgery is a risky and challenging procedure. The rapid recovery of motor function and mental health is challenging in the field of post-nursing care. Ge et al[31] searched cardiac surgery-related vocabulary through a database, extracted and summarized the evidence related to early postoperative rehabilitation exercise, and concluded that early cardiac rehabilitation should be implemented in a planned and procedural manner based on the concept of multidisciplinary team collaboration and nursing orientation. Further, psychological nursing and health education should be implemented throughout the entire rehabilitation training process[31]. Long et al[32] implemented rehabilitation process management for 127 patients who had undergone cardiac surgery. By establishing a rehabilitation nursing quality control group, they formulated and implemented a progressive graded activity process for patients in the early postoperative period and controlled for quality in the implementation process. The results showed that this method could improve the cognitive level of nurses’ early related knowledge, increase the efficiency of team cooperation, accelerate the recovery of patients, and shorten the length of the hospital stay.
Enhanced recovery after surgery (ERAS) is a multimodel, interdisciplinary nursing improvement program designed to promote the recovery of patients undergoing surgery throughout the perioperative period[33]. Interventions cover the entire surgical process, including preoperative, intraoperative, and postoperative periods[34]. The idea is that patients perform better when emotional and physical stress is minimized during surgery. The goal is to return them to normal functioning as soon as possible[35]. Li et al[36] selected 104 patients undergoing cardiac valve surgery for ERAS protocol optimization nursing, and the results showed that this method could reduce ICU and hospital stays, postoperative complications, and costs for cardiac surgery patients.
Kakar et al[37] conducted a database search for a review and meta-analysis of music intervention during cardiac surgery and found that it significantly reduced postoperative anxiety and pain during surgery. Furthermore, no side effects were observed.
The zero-defect nursing theory is a personalized and creative holistic nursing model based on zero defects, with the goal of minimizing patients’ physical pain and psychological unhappiness. Nursing staff should receive professional training in zero-defect theoretical knowledge before carrying out nursing practices. Preoperative health education and psychological counseling for patients can improve their cognitive and psychological stress responses to surgery. Wang et al[38] adopted zero-defect and psychological nursing models to provide perioperative nursing care for 30 patients undergoing cardiac surgery and found that the operative time, intraoperative blood loss, and length of hospital stay decreased significantly. Moreover, the sleep quality and mental and psychological status of patients improved significantly, indicating clinical value.
Cardiac surgery is the most effective method for treating heart disease, especially valvular disease. However, patients’ conditions are complicated, the operations are difficult, and many urgent conditions arise during surgery. In recent years, with the development of science and technology, the mortality rate of patients after cardiac surgery has declined. However, the surgical procedure still has a negative impact on patients’ lives. Adverse effects include post-traumatic stress reactions, decreased postoperative activity, and a reduced quality of life. Most studies have focused on patients’ postoperative health status and functional symptoms. An increasing number of studies have found that the disease burden, functional status, and psychological feelings of patients throughout the perioperative period affect postoperative rehabilitation. Therefore, reasonable and feasible treatment and nursing modes should be formulated according to a patient’s status and psychological state to improve the treatment effect and promote recovery[39]. In summary (Table 1), effective nursing methods can be implemented before, during, and after surgery according to the individual situations of patients to accelerate their recovery, shorten the length of the hospital stay, reduce the economic burden and complications, and provide a reference for clinical practice.
| Item | Nursing approach | Nursing measures | Nursing outcomes |
| Preoperative nursing | Predictive nursing[11] | Guiding the patient to use Betadine mouthwash before surgery | Postoperative pneumonia risk reduced by approximately 50% |
| Individualized education[12,13] | Providing individualized preoperative care for 30-90 min based on the patient's sources of anxiety | Patients quickly adapt to the ICU environment, with a satisfaction rate of 94% given for preoperative education | |
| Inspiratory muscle training[14] | Instructing the patient to undergo respiratory muscle training for 5 d | Marked improvement in postoperative respiratory muscle strength, reducing the incidence of complications and hospital stay | |
| Orientation tour[15] | One day before surgery, healthcare personnel visit the patient to explain the surgical process (15 min) and accompany them to visit an unattended operating room at night (10 min), the ICU (5 min), an operating room (10 min) | Decreased levels of anxiety | |
| Intraoperative nursing | PDCA cycle intervention[16,17] | Using the PDCA cycle management method, continuous quality improvement is implemented in the preparation phrase for cardiac surgery by the methods of identifying the causes, formulating countermeasures, eliminating potential risks, optimizing workflow, and so on | Reduces the variability and risks of operating room work to ensure smooth surgical procedures |
| Holistic care[18] | Four 30- to 45-min sessions of nursing intentional presence were conducted for each patient individually in the intervention group | Effectively reduce depression, stress, and anxiety in surgical patients | |
| Postoperative nursing | Comfort nursing intervention[19] | Collecting demographic details, comfort behaviors, hemodynamic parameters, and other data and implementing comfort care interventions | Majorly improve indicators of postoperative pain, discomfort, respiration, and heart rate in pediatric patients |
| Cold compress nursing[20] | Using cold compresses to alleviate pain caused by chest tube removal after cardiac surgery | Cold compress during chest tube removal significantly reduces the severity of pain scores, but the effect is not significant after 15 min of removal | |
| Slow, deep breathing relaxation exercises[21] | Instructing 25 patients undergoing coronary artery bypass graft surgery to perform slow deep breathing relaxation exercises before chest tube removal | Pain levels are significantly reduced at 5 min and 15 min after extubation | |
| Nursing interventions to prevent delirium in ICU[22-25] | Nurse-led preventive nursing interventions targeting patients with visual and auditory impairments, sleep disorders, cognitive impairments, and mobility impairments, among other major risk factors for delirium | Prevents postoperative delirium, reduces its incidence, and shortens mechanical ventilation time and ICU stay | |
| Pain nursing[27,28] | Patients are provided with a 30-min continuous NLP technique and guided imagery relaxation technique using audio CDs to promote behavior formation. Additionally, 0.5% bupivacaine wound infiltration is administered within 12 h after surgery to alleviate pain | Comfort levels markedly improve, reducing postoperative pain and enhancing patient comfort in patients undergoing cardiac surgery | |
| Nurse-led transitional care model[29] | Transitional care is provided for 9 wk after patient discharge, to facilitate their gradual adjustment, along with provision of necessary support | The self-measurement system and quality of life scale scores both significantly improved, and readmission rates were significantly reduced | |
| EGDT | An EGDT team is established to develop personalized, feasible, and progressive rehabilitation plans for patients | EGDT can shorten the duration of endotracheal intubation and ICU stay for patients, reduce the occurrence of complications, and enhance patient satisfaction | |
| Early rehabilitation nursing[30] | A rehabilitation nursing quality control group is created to develop and implement postoperative early progressive graded activity protocols and ensure quality control throughout the implementation process | Early rehabilitation nursing has enhanced nurses' awareness of early interventions and improved team collaboration efficiency, which can accelerate patient recovery and shorten hospital stay | |
| Perioperative nursing intervention | Enhanced recovery surgical nursing[31,32] | A multimodal and interdisciplinary approach is implemented to optimize nursing care throughout the entire surgical process, including preoperative, intraoperative, and postoperative phases | Reduce ICU and hospital stay, postoperative complications, and costs for patients undergoing cardiac surgery |
| Music intervention[37] | Music interventions are utilized for patients during the surgical procedure | Significantly reduce postoperative anxiety and pain in patients undergoing cardiac surgery without any side effects | |
| Zero-defect care model and psychological care[38] | Nursing staff undergo specialized training on the theory of zero defects to enhance their professional competence. They also provide preoperative health education and psychological counseling for patients | Significantly decrease surgical time, intraoperative bleeding, and hospital stay and improve sleep quality, mental well-being, and psychological condition |
| 1. | Erdil F, Elbaş NÖ. Surgical Nursing. 6th ed. Ankara: Tasarım Offset; 2012: 322–328. |
| 2. | Xue J, Li J, Sun D, Sheng L, Gong Y, Wang D, Zhang S, Zou Y, Shi J, Xu W, An M, Dai C, Li W, Zheng L, Vinograd A, Liu G, Kong Y, Li Y. Functional Evaluation of Intermediate Coronary Lesions with Integrated Computed Tomography Angiography and Invasive Angiography in Patients with Stable Coronary Artery Disease. J Transl Int Med. 2022;10:255-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 22] [Reference Citation Analysis (1)] |
| 3. | Zhao J. [Effect of continuous nursing on cardiac rehabilitation in patients with cardiac surgery]. Dangdai Linchuang Yikan. 2022;35:117-119. |
| 4. | Prado-Olivares J, Chover-Sierra E. Preoperatory Anxiety in Patients Undergoing Cardiac Surgery. Diseases. 2019;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Guo P, East L, Arthur A. A preoperative education intervention to reduce anxiety and improve recovery among Chinese cardiac patients: a randomized controlled trial. Int J Nurs Stud. 2012;49:129-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 133] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 6. | Guo P. Preoperative education interventions to reduce anxiety and improve recovery among cardiac surgery patients: a review of randomised controlled trials. J Clin Nurs. 2015;24:34-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Vencloviene J, Beresnevaite M, Cerkauskaite S, Lopatiene K, Grizas V, Benetis R. The effects of weather on depressive symptoms in patients after cardiac surgery. Psychol Health Med. 2023;28:682-692. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 8. | Song X, Wang H, Kashani KB, Wang C. Extracorporeal Membrane Oxygenation using a Modified Cardiopulmonary Bypass System. J Transl Int Med. 2022;10:175-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (1)] |
| 9. | Ball L, Costantino F, Pelosi P. Postoperative complications of patients undergoing cardiac surgery. Curr Opin Crit Care. 2016;22:386-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 10. | Mali S, Haghaninejad H. Pulmonary complications following cardiac surgery. Arch Med Sci Atheroscler Dis. 2019;4:e280-e285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Bardia A, Blitz D, Dai F, Hersey D, Jinadasa S, Tickoo M, Schonberger RB. Preoperative chlorhexidine mouthwash to reduce pneumonia after cardiac surgery: A systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2019;158:1094-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Suhonen R, Leino-Kilpi H, Välimäki M. Development and psychometric properties of the Individualized Care Scale. J Eval Clin Pract. 2005;11:7-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 85] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Ertürk EB, Ünlü H. Effects of pre-operative individualized education on anxiety and pain severity in patients following open-heart surgery. Int J Health Sci (Qassim). 2018;12:26-34. [PubMed] |
| 14. | Chen X, Hou L, Zhang Y, Liu X, Shao B, Yuan B, Li J, Li M, Cheng H, Teng L, Guo M, Wang Z, Chen T, Liu J, Liu Y, Liu Z, Guo Q. The effects of five days of intensive preoperative inspiratory muscle training on postoperative complications and outcome in patients having cardiac surgery: a randomized controlled trial. Clin Rehabil. 2019;33:913-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (2)] |
| 15. | Niknejad R, Mirmohammad-Sadeghi M, Akbari M, Ghadami A. Effects of an orientation tour on preoperative anxiety in candidates for coronary artery bypass grafting: A randomized clinical trial. ARYA Atheroscler. 2019;15:154-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (1)] |
| 16. | Yao X, Zhu H, Wang Y, Xiang Y, Chen Y. Study on the Effect of PDCA Circulation Method on Nursing Quality Management in the Day Operating Room. Contrast Media Mol Imaging. 2022;2022:3503095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 17. | Du J, Yang J, Sun S, Zhi H. [Application Effect of PDCA Cycle in Shortening Preparation Time Management in Compound Operating Room]. Zhongwai Yixue Yanjiu. 2022;20:169-173. [DOI] [Full Text] |
| 18. | Khajian Gelogahi Z, Aghebati N, Mazloum SR, Mohajer S. Effectiveness of Nurse's Intentional Presence as a Holistic Modality on Depression, Anxiety, and Stress of Cardiac Surgery Patients. Holist Nurs Pract. 2018;32:296-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Khaleghi M, Fomani F, Hoseini A. The effect of the comfort care model on distress, pain, and hemodynamic parameters in infants after congenital heart defect surgery. J Neonatal Nurs. 2022;29:108-116. [DOI] [Full Text] |
| 20. | Mohammadi N, Pooria A, Yarahmadi S, Tarrahi MJ, Najafizadeh H, Abbasi P, Moradi B. Effects of Cold Application on Chest Tube Removal Pain in Heart Surgery Patients. Tanaffos. 2018;17:29-36. [PubMed] |
| 21. | Jarrah MI, Hweidi IM, Al-Dolat SA, Alhawatmeh HN, Al-Obeisat SM, Hweidi LI, Hweidi AI, Alkouri OA. The effect of slow deep breathing relaxation exercise on pain levels during and post chest tube removal after coronary artery bypass graft surgery. Int J Nurs Sci. 2022;9:155-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Pantzaris ND, Platanaki C, Tsiotsios K, Koniari I, Velissaris D. The Use of Electroencephalography in Patients with Sepsis: a Review of The Literature. J Transl Int Med. 2021;9:12-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 23. | Lopez MG, Hughes CG, DeMatteo A, O'Neal JB, McNeil JB, Shotwell MS, Morse J, Petracek MR, Shah AS, Brown NJ, Billings FT 4th. Intraoperative Oxidative Damage and Delirium after Cardiac Surgery. Anesthesiology. 2020;132:551-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 83] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 24. | Pieri M, De Simone A, Rose S, De Domenico P, Lembo R, Denaro G, Landoni G, Monaco F. Trials Focusing on Prevention and Treatment of Delirium After Cardiac Surgery: A systematic Review of Randomized Evidence. J Cardiothorac Vasc Anesth. 2020;34:1641-1654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 25. | Wassenaar A, Rood P, Schoonhoven L, Teerenstra S, Zegers M, Pickkers P, van den Boogaard M. The impact of nUrsiNg DEliRium Preventive INnterventions in the Intensive Care Unit (UNDERPIN-ICU): A study protocol for a multi-centre, stepped wedge randomized controlled trial. Int J Nurs Stud. 2017;68:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Song Y, Yang M, Ling Y, Lin Q. [Effects of nursing delirium preventive interventions in the intensive care unit on delirium management in patients after cardiac surgery]. Zhongguo Huli Guanli. 2022;22:507-511. |
| 27. | Doğan A, Saritaş S. The effects of neuro-linguistic programming and guided imagery on the pain and comfort after open-heart surgery. J Card Surg. 2021;36:2389-2397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Luque Oliveros M, Morilla Romero de la Osa R. Bupivacaine infiltration for acute postoperative pain management after cardiac surgery. Nurs Crit Care. 2022;27:223-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Coskun S, Duygulu S. The effects of Nurse Led Transitional Care Model on elderly patients undergoing open heart surgery: a randomized controlled trial. Eur J Cardiovasc Nurs. 2022;21:46-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Lin Y, Li S, Xie B. [Nursing effect analysis of intervention based on early goal-directed activities in the rehabilitation of patients after cardiac surgery]. Xinxueguanbing Fangzhi Zhishi. 2021;11:82-84. |
| 31. | Ge W, Liu F, Yao H. [Summary of best evidence on early rehabilitation exercise for patients after cardiac surgery]. Hulixue Zazhi. 2021;36:85-89. |
| 32. | Long H, Yang J, Li S, Zhong X, Huang Z, Wu L. [Early rehabilitation nursing process management for ICU patients after cardiac surgery]. Hulixue Zazhi. 2020;35:1-4. |
| 33. | Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg. 2017;152:292-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1487] [Cited by in RCA: 2434] [Article Influence: 270.4] [Reference Citation Analysis (1)] |
| 34. | Varadhan KK, Lobo DN, Ljungqvist O. Enhanced recovery after surgery: the future of improving surgical care. Crit Care Clin. 2010;26:527-547, x. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 35. | Salenger R, Morton-Bailey V, Grant M, Gregory A, Williams JB, Engelman DT. Cardiac Enhanced Recovery After Surgery: A Guide to Team Building and Successful Implementation. Semin Thorac Cardiovasc Surg. 2020;32:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 36. | Li M, Zhang J, Gan TJ, Qin G, Wang L, Zhu M, Zhang Z, Pan Y, Ye Z, Zhang F, Chen X, Lin G, Huang L, Luo W, Guo Q, Wang E. Enhanced recovery after surgery pathway for patients undergoing cardiac surgery: a randomized clinical trial. Eur J Cardiothorac Surg. 2018;54:491-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 139] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 37. | Kakar E, Billar RJ, van Rosmalen J, Klimek M, Takkenberg JJM, Jeekel J. Music intervention to relieve anxiety and pain in adults undergoing cardiac surgery: a systematic review and meta-analysis. Open Heart. 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 38. | Wang H, Zhao X, Liu L, Zhang L. [Application of zero defect nursing model and psychological nursing in operating room in the practice of heart surgery]. Xinli Yuekan. 2020;15:152-153. |
| 39. | Guo H, Chen X, Zheng J. [Application progress of patient-reported outcomes assessment tools for patients undergoing cardiac surgery]. Huli Yanjiu. 2021;35:1027-1030. |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Leker RR, Israel; Lerner A, Israel S-Editor: Fan JR L-Editor: A P-Editor: Zhang XD