Published online Oct 26, 2023. doi: 10.12998/wjcc.v11.i30.7485
Peer-review started: August 4, 2023
First decision: August 24, 2023
Revised: August 26, 2023
Accepted: September 25, 2023
Article in press: September 25, 2023
Published online: October 26, 2023
Processing time: 82 Days and 1.6 Hours
Immunoglobulin G4-related prostate disease (IgG4-RPD) characterized by a high count of IgG4-positive plasma cells has distinctive serological and radiological findings. Here we report a case of a patient who was successfully treated for IgG4-RPD, which manifested as frequent micturition, dysuric, and systemic lymphadenopathy.
The patient was a 33-year-old man who was referred to our hospital because of urinary tract symptoms that had persisted for 4 years. A physical examination revealed systemic lymphadenopathy and blood tests showed hyperglobulinemia with an IgG level of 18.90 g/L and an IgG4 level of 18.40 g/L. Computed tomography (CT) revealed bilateral lacrimal gland, right parotid gland and prostatic enlargement. Based on these findings, IgG4-RD was suspected, and further pathological examination and follow-up results showed expected results. Finally, the patient was diagnosed with IgG4-RPD based on clinical symptoms, pathological examination, therapeutic effects, and follow-up results. He received 50 mg oral prednisolone (the dose was gradually reduced and a low dose was used for long-term maintenance) in combination with cyclophosphamide 1.0 g via an intravenous drip for 6 mo. One year after the treatment was initiated, he was free of urinary or other complaints and his serum IgG4 level normalized.
In IgG4-RPD with severe urinary tract symptoms, radiological findings should be carefully examined. IgG4-RPD prognosis is good because the disease responds well to glucocorticoids. Furthermore, it is urgent for clinicians and pathologists to improve their understanding of IgG4-RPD.
Core Tip: Immunoglobulin G4-related prostate disease (IgG4-RPD) characterized by a high count of IgG4-positive plasma cells has distinctive serological and radiological findings. Here we report a case of a patient who was successfully treated for IgG4-RPD, which manifested as frequent micturition, dysuric, and systemic lymphadenopathy.
- Citation: Yu Y, Wang QQ, Jian L, Yang DC. Infrequent organ involvement in immunoglobulin G4-related prostate disease: A case report. World J Clin Cases 2023; 11(30): 7485-7491
- URL: https://www.wjgnet.com/2307-8960/full/v11/i30/7485.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i30.7485
IgG4-related disease (IgG4-RD) is a chronic and systemic disease that can involve multiple organs. It has been recently recognized as an emerging clinicopathological entity characterized by several features[1,2]. Its clinical symptoms vary depending on the affected organs, but they are relatively mild, and organ swelling may be the only diagnostic clue in many patients. IgG4-RD is diagnosed by a combination of clinical, serological, and radiological findings along with pathological features[3]. IgG4-related prostate disease (IgG4-RPD) is a comprehensive term for prostate lesions associated with IgG4-RD[4]. In view of the general lack of understanding of the disease and the small number of cases reported at home and abroad, in order to improve the understanding, diagnosis, and treatment of the disease, the clinical characteristics and experience of the diagnosis and treatment of IgG4-RPD are discussed[5,6]. Here, we describe a case of highly advanced IgG4-RPD presenting as mass-like regions with urinary tract symptoms.
frequent urination, dysuric, and urinary hesitancy for 4 years.
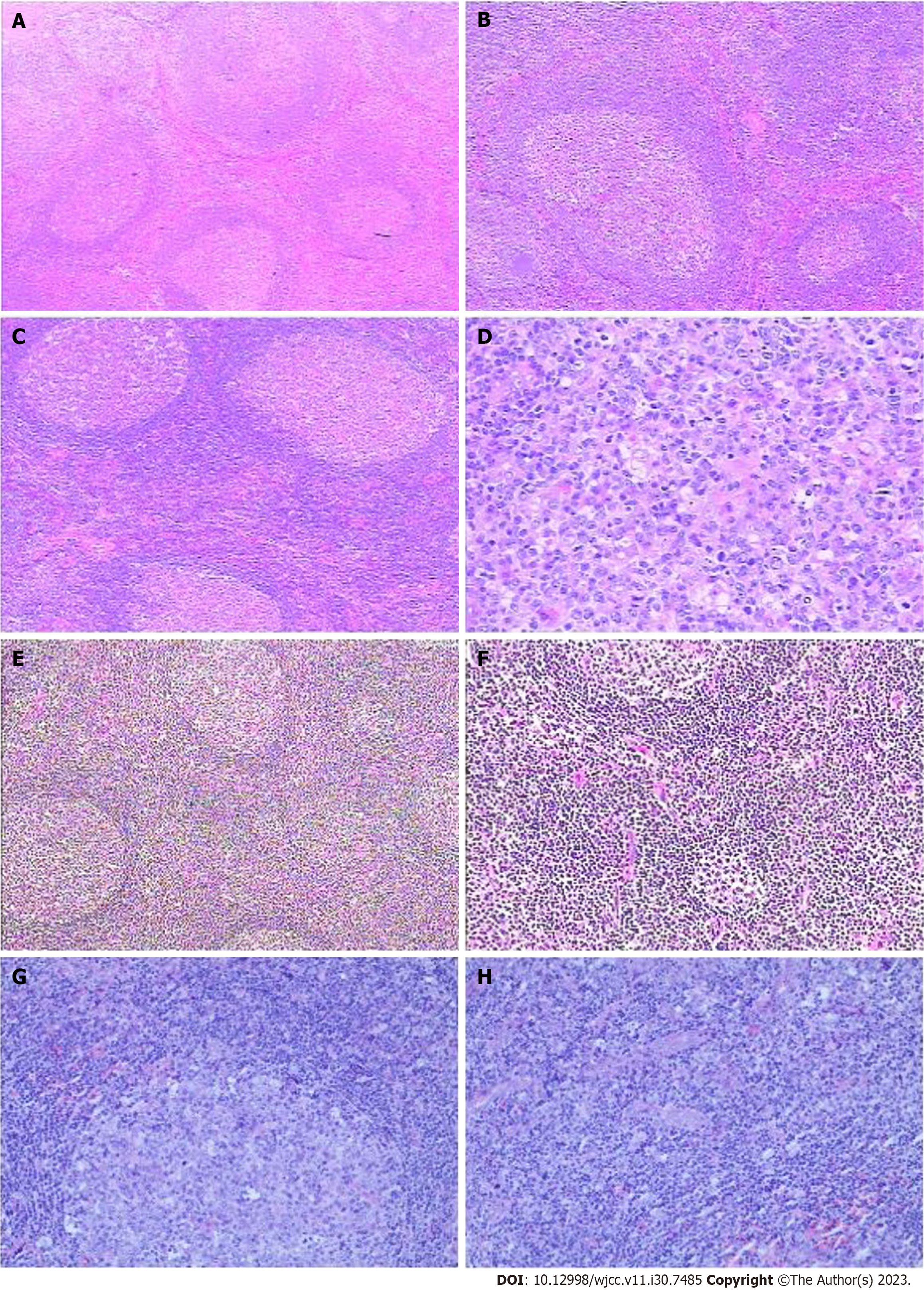
The patient had a cough and expectoration in February 2015. A peanut-sized mass was found in the right mandibular. The mass was not painful and showed a progressive increase in size accompanied by pharynx itch and sensation of a foreign body in the pharynx. In June 2015, the patient gradually developed urinary tract symptoms including frequent urination, nocturia, and urinary retention. Positron emission tomography/computed tomography (CT) showed multiple enlarged lymph nodes in the pelvic cavity. Prostatic posterior metabolism was active and the lesions were considered benign. Biopsy of right submaxillary lymph nodes suggested Castleman’s disease (CD) (Figure 1). Thus, two courses of the R-cyclophosphamide, adriamycin, vincristine, and prednisone (CHOP) regimen (mabthera 600 mg d1, cyclophosphamide 1.4 g d2, doxorubicin 30 mg d2, vincristine 2 mg d2, and prednisone 100 mg d2-6) was administered. The patient was administered prednisone 100 mg for 3 d after discharge. The mandibular lymph nodes significantly reduced after treatment. However, the patient required treatment with lenalidomide 25 mg qd for 3 years, but was irregular in taking his medication. The patient was treated with the IL-6R antibody at the department of lymphomatology of our hospital 13th August 2018.
He doesn’t have a chronic illness.
No special medical history.
The patient’s eyelids of both eyes were found to be slightly swollen and the eyeballs appeared slightly prominent. Furthermore, bilateral cervical lymph nodes were enlarged, about 3 cm × 3 cm, in size and elliptical; the texture was soft, the surface was smooth, and there was no adhesion with the surrounding tissue and no tenderness. There was no deformity in the skull; slight edema was noted on the head and face. Bilateral inguinal lymph nodes might have been enlarged.
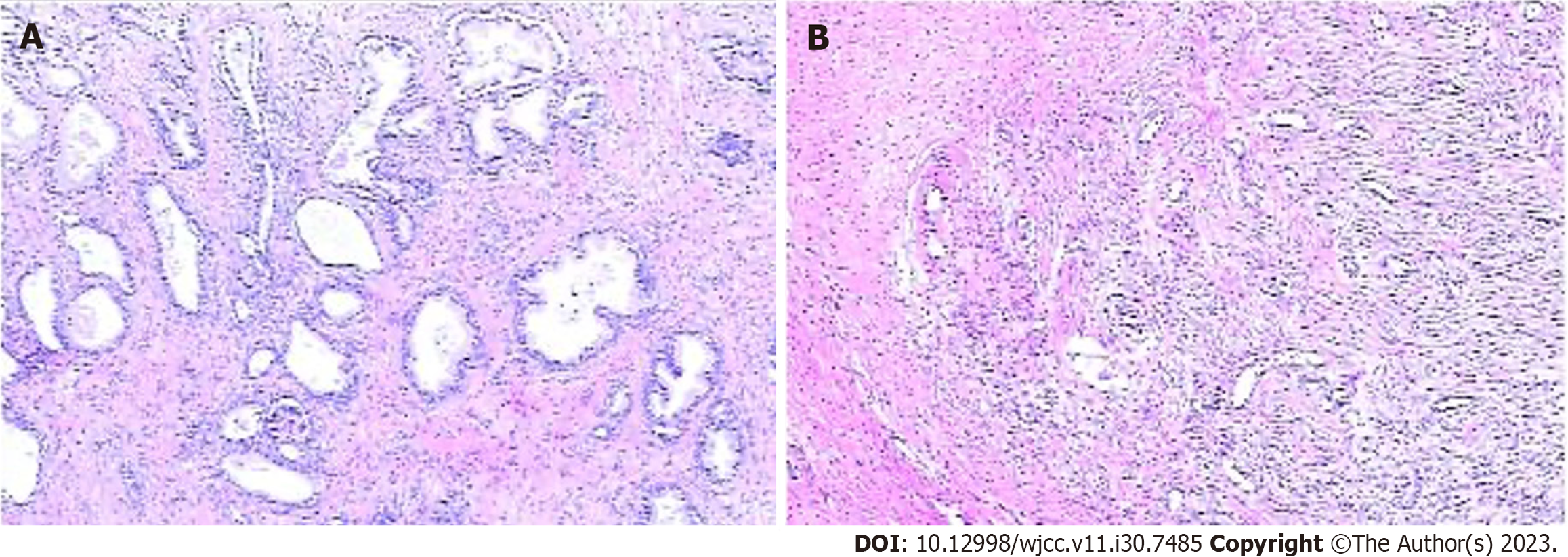
Prostate gland biopsy: Immunohistochemical examination showed a large number of IgG4-positive plasma cells and the IgG4/IgG ratio was more than 50% (Figure 2).
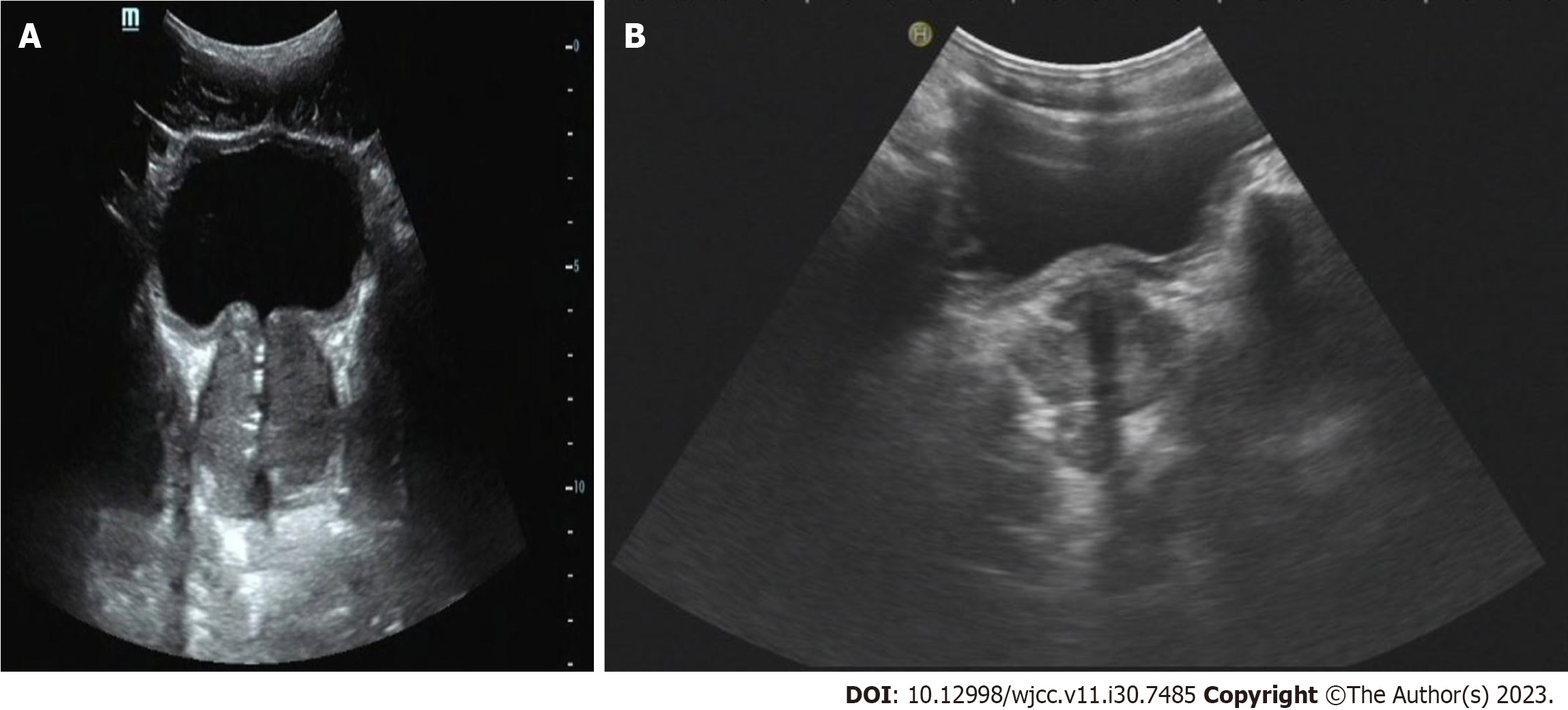
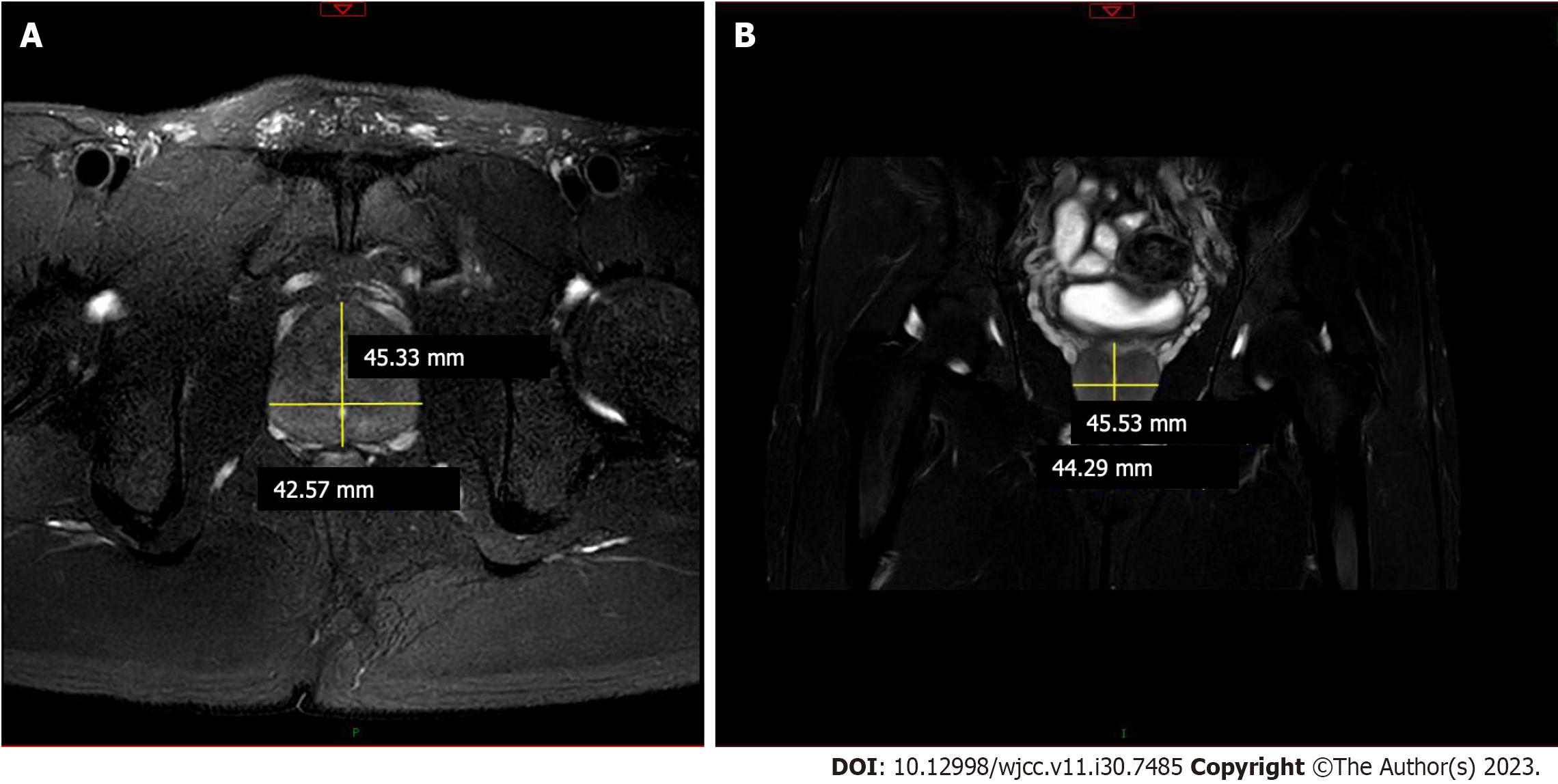
B ultrasonic and magnetic resonance imaging examination revealed prostatic enlargement and multiple lymphadenopathies (Figures 3 and 4).
He had multiple lymphadenopathies. The patient’s serum IgG4 level was > 1.89 g/L, and prostate gland biopsy indicated an IgG4/IgG ratio of > 40%, which was in accord with the diagnostic criteria of IgG4-RPD.
The patient was additionally treated with an intravenous drip of cyclophosphamide 1.0 g for 6 mo and oral prednisolone (the dose was gradually reduced and a low dose was used for long-term maintenance).
One year later (25th December 2019), we documented substantial reductions in the levels of serum IgG (1.22 g/L) and IgG4 (1.18 g/L). In the following 12 mo, the patient’s medical condition remained stable, and he was free of urinary or other complaints. A repeat prostate B-ultrasound showed significant reduction of the prostate gland, indicating an obvious effect.
The concept of IgG4-RD was first introduced by Kamisawa et al[7] and the condition was named in 2010. At present, IgG4-RD is considered to be an autoimmune syndrome involving multiple organs and tissues, and chronic and progressive. Due to the extensive proliferative infiltration and sclerosis of IgG4-positive plasmacytes in organs or tissues, one or more organs often show tumor-like swelling and enlargement. This characteristic makes it difficult to distinguish the disease from other lymphoproliferative diseases such as CD or lymphoma, especially in the early stages. IgG4-RD is an autoimmune-mediated inflammatory fibrotic disease, which has been gradually recognized. The disease can involve many organs or systems, resulting in tissue damage, organ enlargement, and even organ failure.
In recent years, IgG4-associated lymphadenopathy has been in focus. The histologic characteristics of lymphadenopathy are varied and can be summarized as follows: CD, lymphoid follicular reactive hyperplasia, follicular plasmacytes, immunoblastoma, progressive transformation of the germinal center, and inflammatory pseudotumor. However, not all IgG4-RD patients who have the histologic characteristics of lymphadenopathy mentioned above. Only few patients had increased IgG4-positive plasma cells. For example, in a study conducted 26 patients, the histological characteristics of lymph nodes were similar to those associated with CD. Follicular proliferative and interstitial plasmacytes increased in one patient, but only one patient showed an increase in the number and proportion of IgG4-positive plasma cells in the lymph nodes[7,8]. The risk of malignant tumor is increased in IgG4-RD, especially malignant lymphoma. The clinical manifestations of lymphoma can be similar to the primary disease, which can easily result in misdiagnosis or delayed diagnosis and treatment, and should be paid attention to by clinicians. However, the tumor can progress in the later stage, and clinicians are highly suspicious of the tumor. Lymphoma is often diagnosed at the same time as IgG4-RD or after the diagnosis of IgG4-RD. Two studies reported that patients diagnosed with IgG4-RD had MALT lymphoma at the same time or at different times[9,10]. In another study, three patients with IgG4-RD were misdiagnosed with multicentric CD[11].
Multiple lymphadenopathies are a common clinical manifestation of CD and IgG4-RD. Diffuse lymphoplasmacytic infiltration, fibrosis, and a high percentage of IgG4 (+) plasmacytes are the histopathological features of IgG4-related diseases. The pathological characteristics of IgG4-RD and CD intersect to some extent. The differential diagnosis of IgG4-RD and CD is thus very difficult, and comprehensive evaluation is necessary as diagnosis cannot be solely based on serological, pathological, or immunohistochemical results. IgG4-RPD is a comprehensive term for prostate lesions associated with IgG4-RD, prostate involvement with IgG4-RD is very rare, patients were often presented with urine retention symptoms[12,13].
Because IgG4-RD and polycentric CD have their own effective and different treatment schemes, antidiastole is very important[14]. Polycentric CD is mostly invasive, and the treatment usually involves combination chemotherapy. Combination chemotherapy regimens such as CHOP and cyclophosphamide, vincristine, and prednisone can be used. The use of glucocorticoids alone can alleviate the clinical symptoms of CD to some extent but the duration of maintenance is short. Patients with IgG4-RD responded well to glucocorticoids[15]. Therefore, a definite diagnosis is helpful to guide treatment and avoid unnecessary chemotherapy or surgery due to the misdiagnosis of the tumor.
To avoid misdiagnosis or delayed diagnosis of patients with injury or organ dysfunction, it is urgent for clinicians and pathologists to improve the understanding of IgG4-RD. Thus far, for the diagnosis of IgG4-RD, clinicians need to determine clinical, serological, imaging, and pathological features, but the diagnosis cannot be solely based on a single examination or pathological results alone[16]. IgG4-RD responds well to glucocorticoid therapy, resulting in a good prognosis. Therefore, it is very important to correctly diagnose and distinguish this disease.
The lesson from this case is that as this is a new disease, not many cases of IgG4-RPD have yet been reported and that doctors’ understanding of the disease is inadequate. Therefore, it is of great significance to improve pathologists’ understanding of the disease and to treat the disease correctly.
| 1. | Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, Klöppel G, Heathcote JG, Khosroshahi A, Ferry JA, Aalberse RC, Bloch DB, Brugge WR, Bateman AC, Carruthers MN, Chari ST, Cheuk W, Cornell LD, Fernandez-Del Castillo C, Forcione DG, Hamilos DL, Kamisawa T, Kasashima S, Kawa S, Kawano M, Lauwers GY, Masaki Y, Nakanuma Y, Notohara K, Okazaki K, Ryu JK, Saeki T, Sahani DV, Smyrk TC, Stone JR, Takahira M, Webster GJ, Yamamoto M, Zamboni G, Umehara H, Stone JH. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25:1181-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1714] [Cited by in RCA: 1820] [Article Influence: 130.0] [Reference Citation Analysis (0)] |
| 2. | Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366:539-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1856] [Cited by in RCA: 1930] [Article Influence: 137.9] [Reference Citation Analysis (83)] |
| 3. | Yadlapati S, Verheyen E, Efthimiou P. IgG4-related disease: a complex under-diagnosed clinical entity. Rheumatol Int. 2018;38:169-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Martínez-de-Alegría A, Baleato-González S, García-Figueiras R, Bermúdez-Naveira A, Abdulkader-Nallib I, Díaz-Peromingo JA, Villalba-Martín C. IgG4-related Disease from Head to Toe. Radiographics. 2015;35:2007-2025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 5. | Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Matsui S, Sumida T, Mimori T, Tanaka Y, Tsubota K, Yoshino T, Kawa S, Suzuki R, Takegami T, Tomosugi N, Kurose N, Ishigaki Y, Azumi A, Kojima M, Nakamura S, Inoue D; Research Program for Intractable Disease by Ministry of Health, Labor and Welfare (MHLW) Japan G4 team. A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol. 2012;22:1-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 296] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 6. | Takahashi H, Yamamoto M, Suzuki C, Naishiro Y, Shinomura Y, Imai K. The birthday of a new syndrome: IgG4-related diseases constitute a clinical entity. Autoimmun Rev. 2010;9:591-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 117] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 7. | Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, Okamoto A, Egawa N, Nakajima H. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38:982-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1011] [Cited by in RCA: 1000] [Article Influence: 45.5] [Reference Citation Analysis (0)] |
| 8. | Rollins-Raval MA, Felgar RE, Krasinskas AM, Roth CG. Increased numbers of IgG4-positive plasma cells may rarely be seen in lymph nodes of patients without IgG4-related sclerosing disease. Int J Surg Pathol. 2012;20:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Matsuo T, Ichimura K, Yoshino T. Local recurrence as immunoglobulin G4 (IgG4)-related disease 10 years after radiotherapy to ocular adnexal extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. J Clin Exp Hematop. 2011;51:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Oyama T, Takizawa J, Nakamura N, Aoki S, Aizawa Y, Abe H. Multifocal mucosa-associated lymphoid tissue lymphoma associated with IgG4-related disease: a case report. Jpn J Ophthalmol. 2011;55:304-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Sato Y, Kojima M, Takata K, Morito T, Mizobuchi K, Tanaka T, Inoue D, Shiomi H, Iwao H, Yoshino T. Multicentric Castleman’s disease with abundant IgG4-positive cells: a clinical and pathological analysis of six cases. J Clin Pathol. 2010;63:1084-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Li D, Kan Y, Fu F, Wang S, Shi L, Liu J, Kong L. IgG4-related prostatitis progressed from localized IgG4-related lymphadenopathy. Int J Clin Exp Pathol. 2015;8:11747-11752. [PubMed] |
| 13. | Chang J, Zhang W. Infrequent organ involvement of IgG4-related diseases: a literature review. Clin Rheumatol. 2018;37:1153-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Wallace ZS, Zhang Y, Perugino CA, Naden R, Choi HK, Stone JH; ACR/EULAR IgG4-RD Classification Criteria Committee. Clinical phenotypes of IgG4-related disease: an analysis of two international cross-sectional cohorts. Ann Rheum Dis. 2019;78:406-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 290] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 15. | Bledsoe JR, Della-Torre E, Rovati L, Deshpande V. IgG4-related disease: review of the histopathologic features, differential diagnosis, and therapeutic approach. APMIS. 2018;126:459-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 16. | Umehara H, Okazaki K, Kawano M, Mimori T, Chiba T. How to diagnose IgG4-related disease. Ann Rheum Dis. 2017;76:e46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Rheumatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Glumac S, Croatia; Pavlidis TE, Greece S-Editor: Chen YL L-Editor: A P-Editor: Zhang XD