Published online Oct 16, 2023. doi: 10.12998/wjcc.v11.i29.7187
Peer-review started: July 18, 2023
First decision: August 24, 2023
Revised: August 30, 2023
Accepted: September 12, 2023
Article in press: September 12, 2023
Published online: October 16, 2023
Processing time: 86 Days and 21.5 Hours
Takotsubo cardiomyopathy, also called apical ballooning syndrome, is a disease that is often triggered by stress factors in postmenopausal women and mimics acute coronary syndrome. The aim of this article is to draw attention to takotsubo cardiomyopathy after surgical treatment of liver hydatid cyst.
A 50-year-old diabetic and hypertensive female patient was evaluated preoperatively before general surgery for liver hydatid cyst, and no cardiac problems were found. The patient was discharged on the 3rd postoperative day without any postoperative complications. On postoperative day 5, the patient presented to the emergency department with fever, shortness of breath, chills, and shivering and was hospitalized with the diagnosis of pneumonia. The troponin levels remained high during follow-up. Echocardiography was performed on postoperative day 7, after which the patient was referred to a tertiary center with the diagnosis of non-ST-elevation myocardial infarction due to akinesia in the apical region. Coronary angiography performed at the tertiary center showed normal coronary anatomy, and the patient was diagnosed with takotsubo cardiomyopathy.
Takotsubo cardiomyopathy mimicking myocardial infarction without ST segment elevation may develop after surgical treatment of liver hydatid cyst.
Core Tip: Takotsubo cardiomyopathy is a type of cardiomyopathy triggered by stress. Echocardiography shows akinesia in the apical region and hyperkinesis in other regions. Clinical, electrocardiographic, and laboratory findings mimic acute coronary syndrome. The diagnosis is made by excluding acute coronary syndrome. In our case, cardiomyopathy developed after surgical treatment of liver hydatid cyst.
- Citation: Altaş Y, Abdullayeva Ü. Case of takotsubo cardiomyopathy after surgical treatment of liver hydatid cyst: A case report. World J Clin Cases 2023; 11(29): 7187-7192
- URL: https://www.wjgnet.com/2307-8960/full/v11/i29/7187.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i29.7187
Takotsubo cardiomyopathy, also referred to as apical ballooning syndrome or broken heart syndrome, is a disease that mimics acute myocardial infarction triggered by stress[1]. Its pathophysiology is thought to include epicardial coronary artery spasm and myocardial dysfunction due to catecholamine discharge[2]. More than 95% of patients are female and mostly postmenopausal[3]. Takotsubo cardiomyopathy was first described by Dote et al[1] in Japan in 1991. Its name refers to the appearance of the left ventricle on ventriculography, which resembles the vessel used by Japanese fishermen for octopus fishing. In subsequent years, many reports on the disease have been published worldwide. According to the Mayo Clinic diagnostic criteria, takotsubo cardiomyopathy has four diagnostic criteria: (1) Transient regional left ventricular akinesia, hypokinesia, or dyskinesia with or without involvement of the apical region; (2) Absence of obstructive coronary artery disease; (3) Electrocardiogram (ECG) derivations including ST segment change and negative T wave or significant elevation of cardiac troponins; and (4) Absence of pheochromocytoma and myocarditis[4]. Diagnosis of the disease is based on the exclusion of acute coronary syndrome. The symptoms of takotsubo cardiomyopathy are often chest pain, shortness of breath, and sweating. ECG shows ST deviation, negative T wave, QT prolongation, and elevated cardiac biomarkers. Echocardiography may reveal akinesia, hypokinesia, dyskinesia in the apical region, and hyperkinesia in other regions. However, coronary angiography reveals normal coronary anatomy.
A 50-year-old woman presented to our hospital with abdominal distension, nausea, and vomiting for 2 mo.
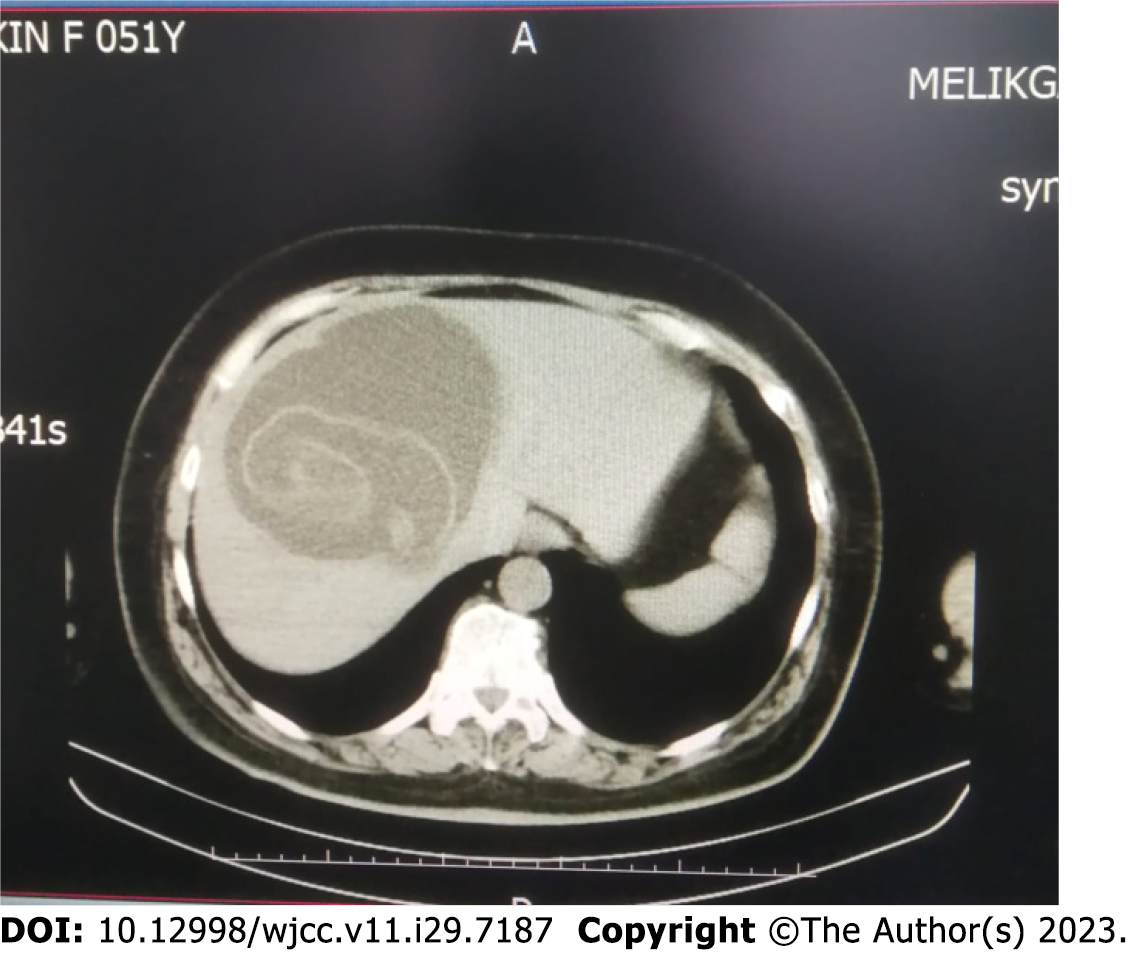
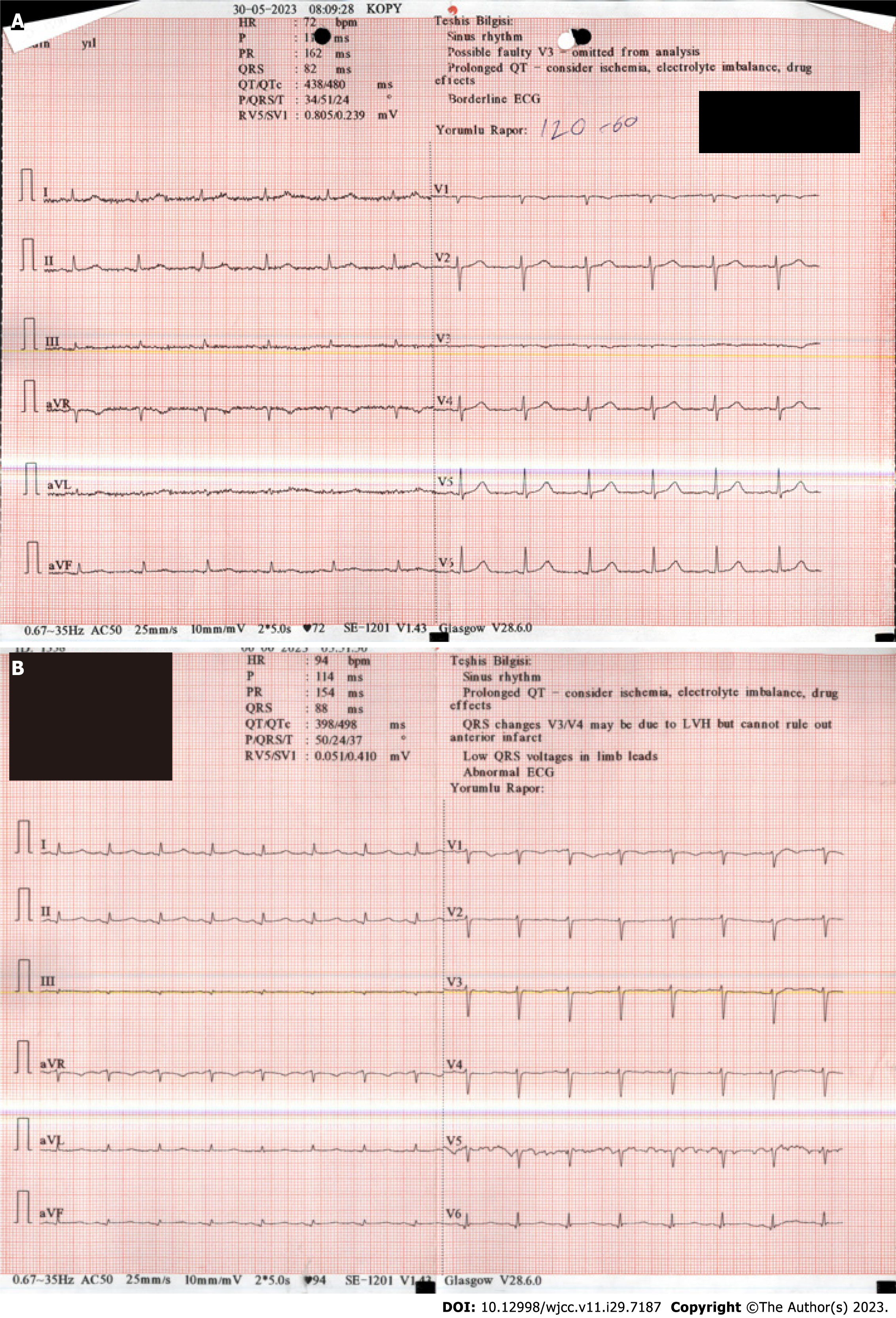
The patient, who had complaints for 2 mo, was admitted to the general surgery outpatient clinic. Abdominal computed tomography (CT) showed a space-occupying lesion consistent with type II liver hydatid cyst with dissociated germinant membrane in liver segments 8, 7, and 5, which was approximately 12 cm × 11 cm in size. Surgery was recommended (Figure 1). The patient's preoperative ECG was unremarkable (Figure 2A). Losartan and metformin treatment was continued during the surgical period.
The patient had a history of type 2 diabetes mellitus and hypertension.
The patient’s personal and family history was unremarkable.
The patient had no remarkable physical examination findings other than a pale appearance.
There were no abnormalities in the patient’s laboratory tests.
The patient’s abdominal CT examination showed a space-occupying lesion consistent with type II hydatid cyst with a dissociated germinal membrane, approximately 12 cm × 11 cm in size in liver segments 8, 7, and 5.
The patient was evaluated by multidisciplinary experts in cardiology, internal medicine and pulmonology in the preoperative period. No serious problems were detected, and the patient was considered suitable for surgery with low risk.
The final diagnosis according to Mayo Clinic criteria was takotsubo cardiomyopathy.
The patient underwent surgical removal of the cyst (Figure 3).
The patient did not require inotropic agents nor vasopressors during surgery. She was discharged on postoperative day 2 without any complication. On postoperative day 4, she was admitted to the emergency room with complaints of fever, shortness of breath, and palpitations. Her C-reactive protein level was 105 mg/L, white blood cell count was 21400/mcL, and troponin I level was 1800 ng/mL. The initial ECG showed no significant features except sinus tachycardia. The ECG taken after rate control was achieved showed a long QTc duration (467 ms) (Figure 2B). Echocardiography performed as a result of the cardiology consultation on these findings showed an akinetic apex and ejection fraction of about 40%. However, we did not record an echo because we initially thought the patient had acute coronary syndrome. The patient was referred to a tertiary center for emergency percutaneous coronary intervention with a diagnosis of non-ST-elevation acute coronary syndrome. Coronary angiography performed at the tertiary center revealed normal coronary anatomy. Takotsubo cardiomyopathy was considered and our patient was followed up. Control echocardiography performed on postoperative day 33 showed complete normalization of left ventricular function. After the patient's left ventricular function improved, only antihypertensive and antidiabetic treatments were continued.
Takotsubo cardiomyopathy is thought to develop due to coronary spasm and myocardial dysfunction as a result of noradrenaline discharge following illness, emotional, and physical stress. Since the 1990s, there have been numerous studies on this condition, some of which are surgically relevant. Cases of takotsubo cardiomyopathy following infection have been reported. Among these, George et al[5] described a case after influenza ¾ a common infection and Achuthanandan et al[6] described a case involving global hypokinesia after coronavirus disease-2019 in a young female. In addition, Izumi[7] reported on a case of takotsubo cardiomyopathy development following drug abuse, and Jalan et al[8] reported on a case developing after a migraine attack.
Some cases of takotsubo cardiomyopathy have developed after cardiac valve surgery. Vazhev and Stoev[9] published a case of takotsubo cardiomyopathy developing after aortic and mitral valve replacement. Some cases develop in the preoperative period. Rodrigues et al[10] published a case of takotsubo cardiomyopathy mimicking ST-elevation myocardial infarction that developed in the preoperative period after general anesthesia. There are also cases in the literature of development after liver transplantation[11-13]. Bhojraj et al[14] published a case of takotsubo cardiomyopathy developing after vaginal hysterectomy. In contrast to takotsubo cardiomyopathy cases, which are frequently seen in the postmenopausal period, Kim et al[15] published a case that developed after cesarean section. The distinctive feature of our case is the development of takotsubo cardiomyopathy after surgery for liver hydatid cyst, specifically in the postoperative period of a noncardiac surgery and which has never before been reported in the literature.
Our patient was diagnosed via interdisciplinary coordination. Pneumonia was initially considered according to physical examination and laboratory findings. Subsequently, postoperative non-ST elevation myocardial infarction was considered according to echocardiography and elevated cardiac biomarker findings; however, coronary angiography showed normal coronary anatomy. A diagnosis of takotsubo cardiomyopathy was made according to Mayo Clinic diagnostic criteria. To the best of our knowledge, this is the first reported case of takotsubo cardiomyopathy after surgical treatment of liver hydatid cyst. Additional studies on takotsubo cardiomyopathy developing after noncardiac surgery are needed.
| 1. | Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. [Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases]. J Cardiol. 1991;21:203-214. [PubMed] |
| 2. | Salathe M, Weiss P, Ritz R. Rapid reversal of heart failure in a patient with phaeochromocytoma and catecholamine-induced cardiomyopathy who was treated with captopril. Br Heart J. 1992;68:527-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Pilgrim TM, Wyss TR. Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: A systematic review. Int J Cardiol. 2008;124:283-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 364] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 4. | Madhavan M, Prasad A. Proposed Mayo Clinic criteria for the diagnosis of Tako-Tsubo cardiomyopathy and long-term prognosis. Herz. 2010;35:240-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 211] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 5. | George AA, John KJ, Jha A, Mishra AK. Infections precipitating Takotsubo cardiomyopathy, an uncommon complication of a common infection. Monaldi Arch Chest Dis. 2022;93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Achuthanandan S, Cordeiro NL, Dhaliwal A, Masri DJ, Sadiq A, Hollander G. COVID-19 Resulting in Global Stress Cardiomyopathy in a Young Female. Cureus. 2022;14:e26779. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Izumi Y. Drug-induced takotsubo cardiomyopathy. Heart Fail Clin. 2013;9:225-231, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Jalan P, Dhakal L, Pandav V, Omar AI. Status migrainosus as a potential stressor leading to takotsubo cardiomyopathy. Cephalalgia. 2012;32:1140-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Vazhev Z, Stoev H. Takotsubo Cardiomyopathy after Elective Aortic and Mitral Valve Replacement. Folia Med (Plovdiv). 2020;62:204-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Rodrigues LB, Batista A, Monteiro F, Duarte JS. ST-segment elevation during general anesthesia for non-cardiac surgery: a case of takotsubo. Braz J Anesthesiol. 2015;65:403-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Vachiat A, McCutcheon K, Mahomed A, Schleicher G, Brand L, Botha J, Sussman M, Manga P. Takotsubo cardiomyopathy post liver transplantation. Cardiovasc J Afr. 2016;27:e1-e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Tachotti Pires LJ, Cardoso Curiati MN, Vissoci Reiche F, Silvestre OM, Mangini S, Carballo Afonso R, Ferraz-Neto BH, Bacal F. Stress-induced cardiomyopathy (takotsubo cardiomyopathy) after liver transplantation-report of two cases. Transplant Proc. 2012;44:2497-2500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Badwan OZ, Abu-Shawer O, Paul A, Faulx M, Barzilai B. Postoperative Apical Ballooning Syndrome Following Orthotopic Liver Transplantation. Cureus. 2023;15:e34450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (1)] |
| 14. | Bhojraj S, Sheth S, Pahlajani D. Postoperative Takotsubo cardiomyopathy. Ann Card Anaesth. 2014;17:157-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Kim SY, Yoon JH, Lee SH. Takotsubo-like severe left ventricular dysfunction after cesarean delivery in a 28-year old woman. Korean Circ J. 2011;41:101-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: El-Serafy AS, Egypt; Mishra AK, United States S-Editor: Lin C L-Editor: A P-Editor: Zhao S