Published online Oct 6, 2023. doi: 10.12998/wjcc.v11.i28.6792
Peer-review started: April 28, 2023
First decision: July 27, 2023
Revised: August 11, 2023
Accepted: September 6, 2023
Article in press: September 6, 2023
Published online: October 6, 2023
Processing time: 150 Days and 4.9 Hours
Pulmonary artery (PA) aneurysms are usually diagnosed radiographically and present as small or large lesions resembling inflammation or a neoplasm on chest radiography. It has rarely been reported as an endobronchial mass.
We report the case of a 64-year-old man who presented with recurrent hemo
Although endobronchial PA aneurysms are rare, bronchoscopists need to add this lesion to the list of endobronchial masses for which a biopsy is to be assiduously avoided.
Core Tip: Pulmonary artery (PA) aneurysms usually present as small or large lesions resembling inflammation or a neoplasm on chest radiography. It is rarely reported as an endobronchial mass. We report a case of a tumorous protrusion blocking the right middle lobe bronchus, which was confirmed to be a PA aneurysm by endobronchial ultrasound bronchoscopy and computed tomography angiography. Although endobronchial pulmonary arterial aneurysm is rare, bronchoscopists need to enhance their awareness and vigilance of this lesion in order to avoid the disastrous consequences caused by improper biopsy.
- Citation: Li M, Zhu WY, Wu RR, Wang L, Mo MT, Liu SN, Zhu DY, Luo Z. Pulmonary artery aneurysm protruding into the bronchus as an endobronchial mass: A case report. World J Clin Cases 2023; 11(28): 6792-6796
- URL: https://www.wjgnet.com/2307-8960/full/v11/i28/6792.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i28.6792
Pulmonary artery (PA) aneurysms are uncommon but often lethal abnormalities of the pulmonary vasculature. The clinical presentation of a PA aneurysm ranges from a silent incidental finding on imaging to severe hemoptysis[1]. Generally, most cases of PA aneurysms are diagnosed radiographically and present as small or large lesions resembling inflammation or neoplasms on chest radiography[2]. Here, we report a rare case of a PA aneurysm diagnosed using a combination of endobronchial ultrasound (EBUS) bronchoscopy and chest computed tomography angiography (CTA), in which the PA aneurysm protruded into the bronchus as an endobronchial mass that blocked the airway lumen.
A 64-year old male patient was admitted to our hospital due to intermittent hemoptysis for 2 wk.
The patient experienced severe episodes of massive hemoptysis without any premonitory symptoms, with a total blood loss of approximately 400-500 mL. Except for a slight cough, no other symptoms, such as fever, sputum production, or chest pain were observed. Before admission, the patient was treated with antibiotics and hemostatics at another hospital. However, the patient’s clinical symptoms were not completely resolved.
The patient had no significant past medical or surgical history.
The patient had no significant personal or family history.
At our hospital, the patient’s vital signs were normal and stable. Pulmonary auscultation revealed moist rales in the middle and lower field of the right lung.
Laboratory tests were unremarkable except for a hemoglobin concentration of 109 g/L (normal 115-150 g/L) and D-dimer 0.69 μg/mL (normal 0-0.5 μg/mL).
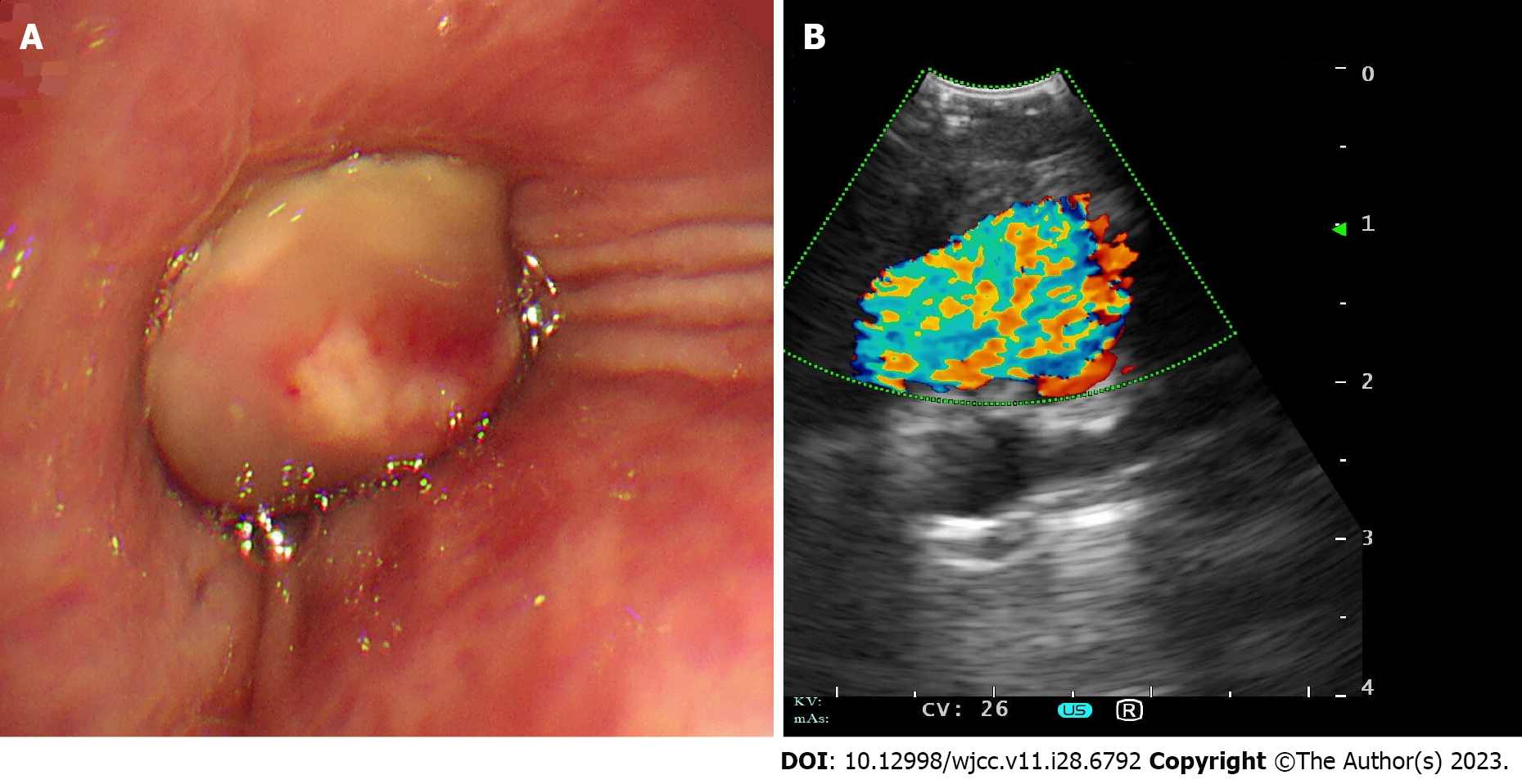
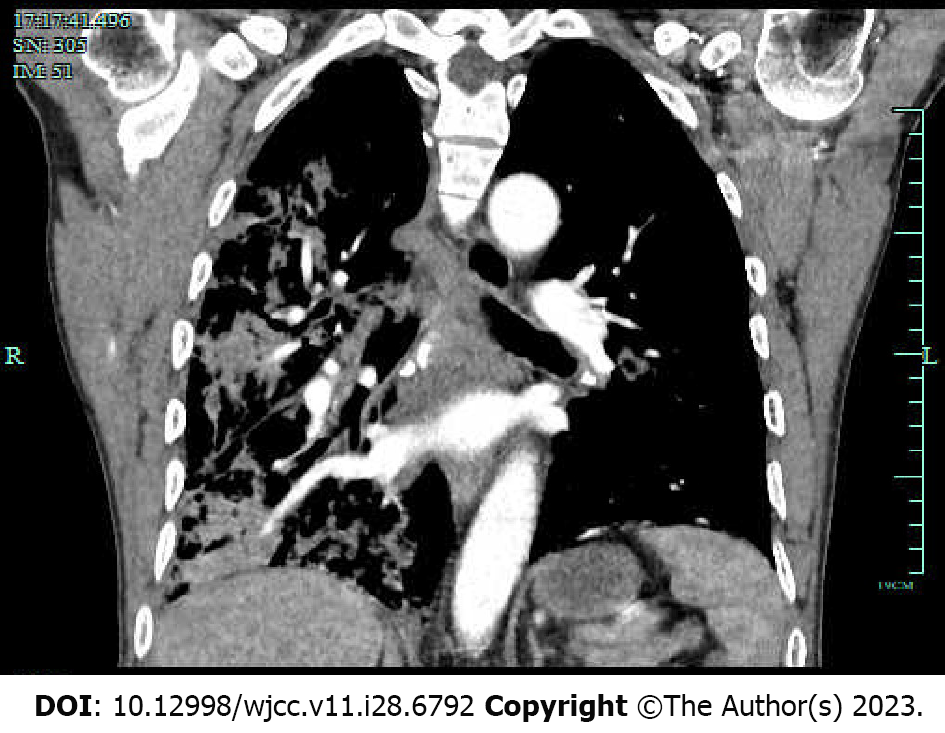
High-resolution computed tomography of the chest revealed partial exudation and consolidation of the right lung. Flexible bronchoscopy was performed to confirm the diagnosis, which showed a smooth-surfaced, flesh colored and tumorous protrusion completely blocking the right middle lobe of the bronchus (Figure 1A). Subsequently, EBUS bronchoscopy was performed to detect the mass, only to find a hypoechoic vascular lesion with a color Doppler flow signal (Figure 1B), suggesting a vascular abnormality of the bronchus. Therefore, the endobronchial biopsy was discontinued because the irritation caused by the biopsy procedure may have caused massive bleeding. CTA of the chest was also performed and revealed a right middle lobe PA aneurysm protruding into the right middle lobe bronchus (Figure 2).
PA aneurysm.
The patient underwent a right middle lobectomy.
The postoperative course was uneventful, and hemoptysis did not recur after the surgery. The patient was discharged on the seventh postoperative day.
PA aneurysms are rare and their prevalence has been estimated to be 1 in 14000 based on the findings from 109571 autopsies conducted at the Mayo Clinic[3]. Currently, PA aneurysms are categorized based on their etiology. PA aneurysms secondary to congenital heart disease have been most frequently reported, with patent ductus arteriosus, ventricular septal defect and atrial septal defects being the most frequently described causes. In addition, PA aneurysms caused by infectious diseases, such as mucormycosis, tuberculosis, and syphilis, have also been reported. PA aneurysms may also occur secondary to pulmonary hypertension, autoimmune diseases or vasculitis. Finally, PA aneurysms with no clear cause were considered idiopathic[4-6]. Generally, PA aneurysms are less often clinically evident and are usually diagnosed based on chest radiographs or at autopsies[7]. Some patients with PA aneurysms may experience shortness of breath, coughing or chest pain[8]. Hemoptysis may imply that an unstable PA aneurysm erodes the airway mucosa[9]. Spontaneous PA aneurysm rupture is rare but is, when it occurs, often a catastrophic complication of massive hemoptysis. Most PA aneurysms appear to rupture into the alveolar parenchyma and do not impinge directly on the bronchus, and they are rarely detected by bronchoscopy[4]. Here, we report a rare condition in which a PA aneurysm protruded into the bronchus as an endobronchial mass that blocked the airway lumen, providing clinical implications for the differential diagnosis and management of endobronchial lesions.
Although the incidence of tumor-like vascular malformations of the bronchus is low, it is highly risky and making the differential diagnosis from a solid endobronchial mass is extremely important. Inappropriate interventions, such as biopsy or fine-needle aspiration of vascular lesions, can have devastating consequences, and in some cases, lead to massive intra-pulmonary bleeding and even death[7,10]. Among the vascular malformations of the bronchus, there are relatively more reports of Dieulafoy's disease[11]. There are even fewer reports of PA aneurysms presenting as endobronchial masses, which rarely protrude into the airway lumen. Two studies described such a condition and both cases were initially misdiagnosed as solid lung masses on conventional imaging[7,12]. Conventional bronchoscopy alone was ineffective. In one case, the lesion was described as a smooth, orange-red intrabronchial mass that protruded into the airway lumen. The signs suggestive of a vascular region, such as a pulsating sensation, and tortuous blood vessels within the submucosa, were absent. Fine needle aspiration biopsy was subsequently performed, resulting in brisk massive hemorrhage[7]. In another case, an endobronchial mass was diagnosed as a PA aneurysm using a convex probe EBUS bronchoscope. Invasive interventions, such as endobronchial biopsies, have been avoided[12]. In the present case, the endobronchial mass was diagnosed as a PA aneurysm using EBUS. Thus, as a useful tool to differentiate vascular from solid endobronchial masses, the EBUS bronchoscope helps to avoid potentially disastrous interventions.
However, we must also mention that intervention techniques like EBUS may not be available in all health care settings. Therefore, it is important to distinguish vascular lesions from solid masses using conventional methods, such as conventional bronchoscopy. In the case reported by Lerner and Riker[12], the endobronchial PA aneurysm presented as a flesh colored and hypervascular lesion. Following continued examination for several circulatory cycles, the lesion was observed to be pulsatile, and its size changed in synchrony with the patient’s pulse[12]. In another case, the PA aneurysm presented as a smooth, orange-red endobronchial mass with a plexiform red pattern, protruding into the airway lumen[7]. In our case, the endobronchial mass had a smooth-surface, was, flesh colored and hypervascularized. Fluoroscopy may show a pulsation within the lesion, known as Pezzi`s sign[3]. All the bronchoscopic appearances could provide bronchoscopists with implications for the endobronchial vascular lesions, in which a biopsy should be assiduously avoided.
Endobronchial vascular malformations, such as endobronchial PA aneurysms, are so rare that they are often not included in the differential diagnoses and are usually missed on plain CT scan. In cases of recurrent unexplained hemoptysis, where chest CT shows no abnormalities, these types of diseases should be considered, and it is necessary to perform CTA. CTA is relatively non-invasive and can effectively identify abnormalities in the vasculature. This case report was confirmed using CTA. Our case emphasizes the importance of CTA for unexplained hemoptysis.
In conclusion, we report a rare endobronchial PA aneurysm, notable for its mimicry of an endobronchial solid mass. Although pathological vascular conditions are extremely rare, they may result in massive hemorrhage with a possibly fatal outcome. Therefore, bronchoscopists must enhance their awareness and vigilance of this lesion to avoid the disastrous consequences of improper biopsy. CTA and EBUS are useful tools for confirming the diagnosis of PA aneurysms and may help avoid inappropriate invasive interventions.
| 1. | Kalra-Lall A, Donaldson J, Martin C 3rd. Brief review: Pulmonary artery aneurysms and pseudoaneurysms. Int J Cardiovasc Imaging. 2019;35:1357-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Gupta M, Agrawal A, Iakovou A, Cohen S, Shah R, Talwar A. Pulmonary artery aneurysm: a review. Pulm Circ. 2020;10:2045894020908780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 68] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 3. | Deterling RA Jr, Clagett OT. Aneurysm of the pulmonary artery; review of the literature and report of a case. Am Heart J. 1947;34:471-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 258] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Badders J, Roughneen P, Mohan N, Roughneen E. Pulmonary Artery Aneurysm: A Rarity and Surgical Enigma. Cureus. 2023;15:e38157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Saldanha R, Ghatanatti R, Gan MD, Kurkure K, Suresh G, Dhorigol VM. Pulmonary mucormycosis causing a mycotic pulmonary artery aneurysm. Asian Cardiovasc Thorac Ann. 2021;29:848-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Salehi AM, Khansari N. Idiopathic Pulmonary Artery Aneurysm: A Case Report. Curr Cardiol Rev. 2022;18:50-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Gibbs PM, Hami A. Pulmonary arterial aneurysm presenting as an endobronchial mass. Thorax. 1995;50:1013-4; discussion 1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Chung CW, Doherty JU, Kotler R, Finkelstein A, Dresdale A. Pulmonary artery aneurysm presenting as a lung mass. Chest. 1995;108:1164-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Bartter T, Irwin RS, Nash G. Aneurysms of the pulmonary arteries. Chest. 1988;94:1065-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 172] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Butto F, Lucas RV Jr, Edwards JE. Pulmonary arterial aneurysm. A pathologic study of five cases. Chest. 1987;91:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Foo AZX, Hsu AAL. Dieulafoy's disease with mediastinal arteriovenous malformation. Thorax. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Lerner AD, Riker DR. Use of endobronchial ultrasonography in the diagnosis of a pulmonary artery aneurysm. Ann Thorac Surg. 2014;97:e139-e141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mansour AM, Lebanon S-Editor: Fan JR L-Editor: Webster JR P-Editor: Fan JR