Published online Oct 6, 2023. doi: 10.12998/wjcc.v11.i28.6733
Peer-review started: July 25, 2023
First decision: August 16, 2023
Revised: August 20, 2023
Accepted: September 11, 2023
Article in press: September 11, 2023
Published online: October 6, 2023
Processing time: 62 Days and 10.3 Hours
Subchondral fatigue fracture of the femoral head (SFFFH) mainly occurs in young military recruits and might be confused with osteonecrosis of the femoral head. However, less research focuses on the risk factor for SFFFH.
To evaluate the intrinsic risk factors for SFFFH in young military recruits.
X-ray and magnetic resonance imaging data were used for analysis. Acetabular anteversion of the superior acetabulum, acetabular anteversion of the center of the acetabulum (AVcen), anterior acetabular sector angle (AASA), posterior aceta
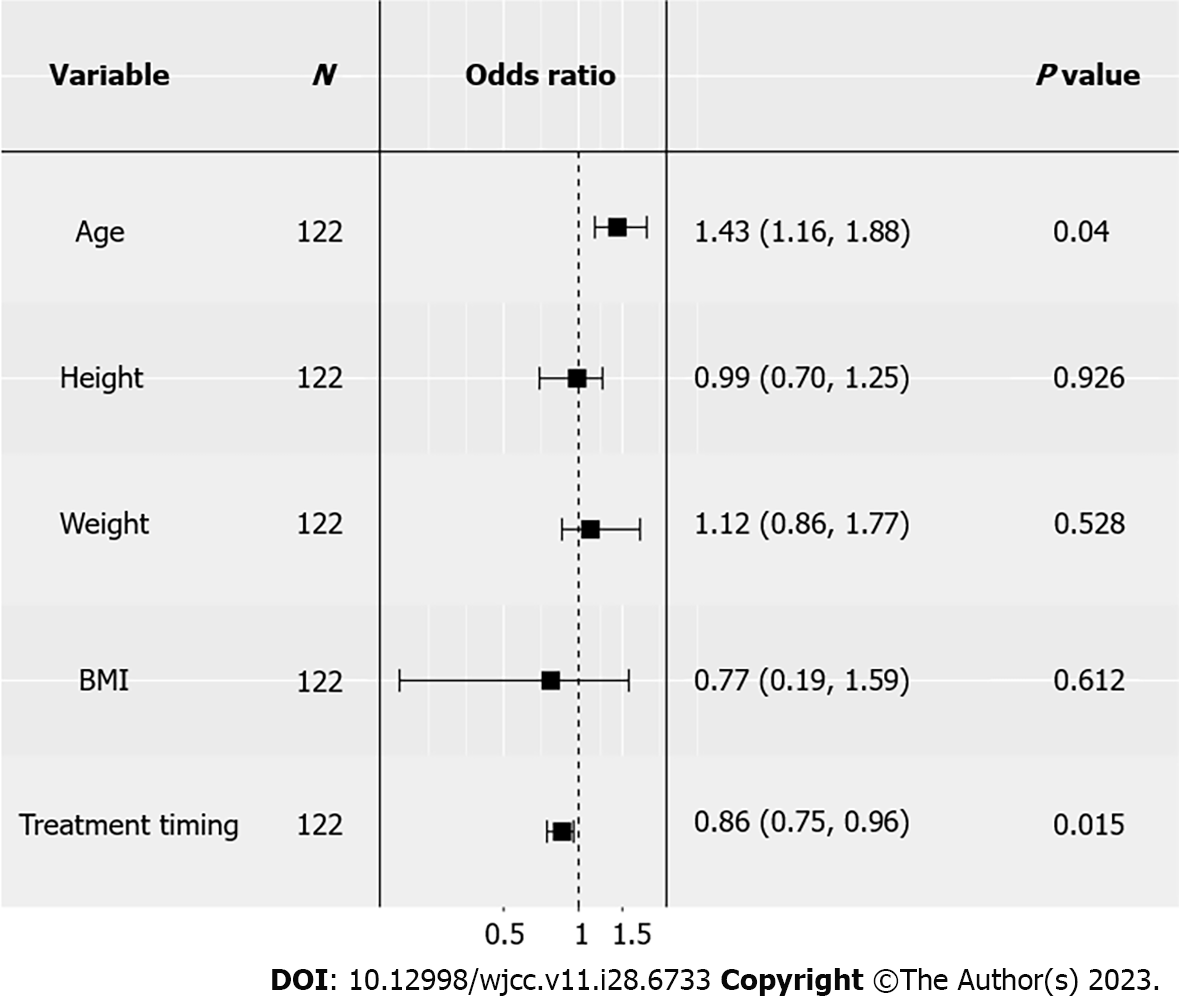
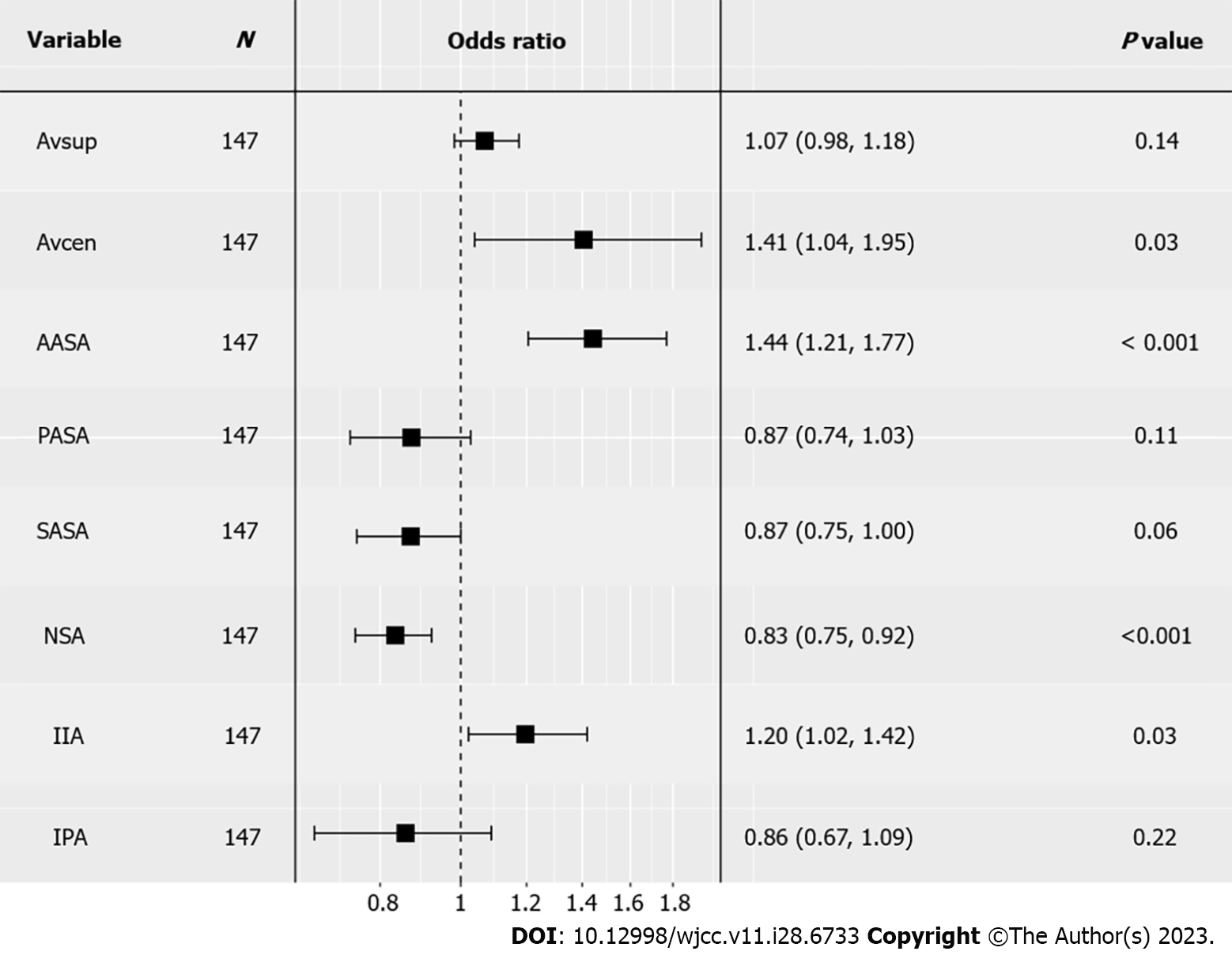
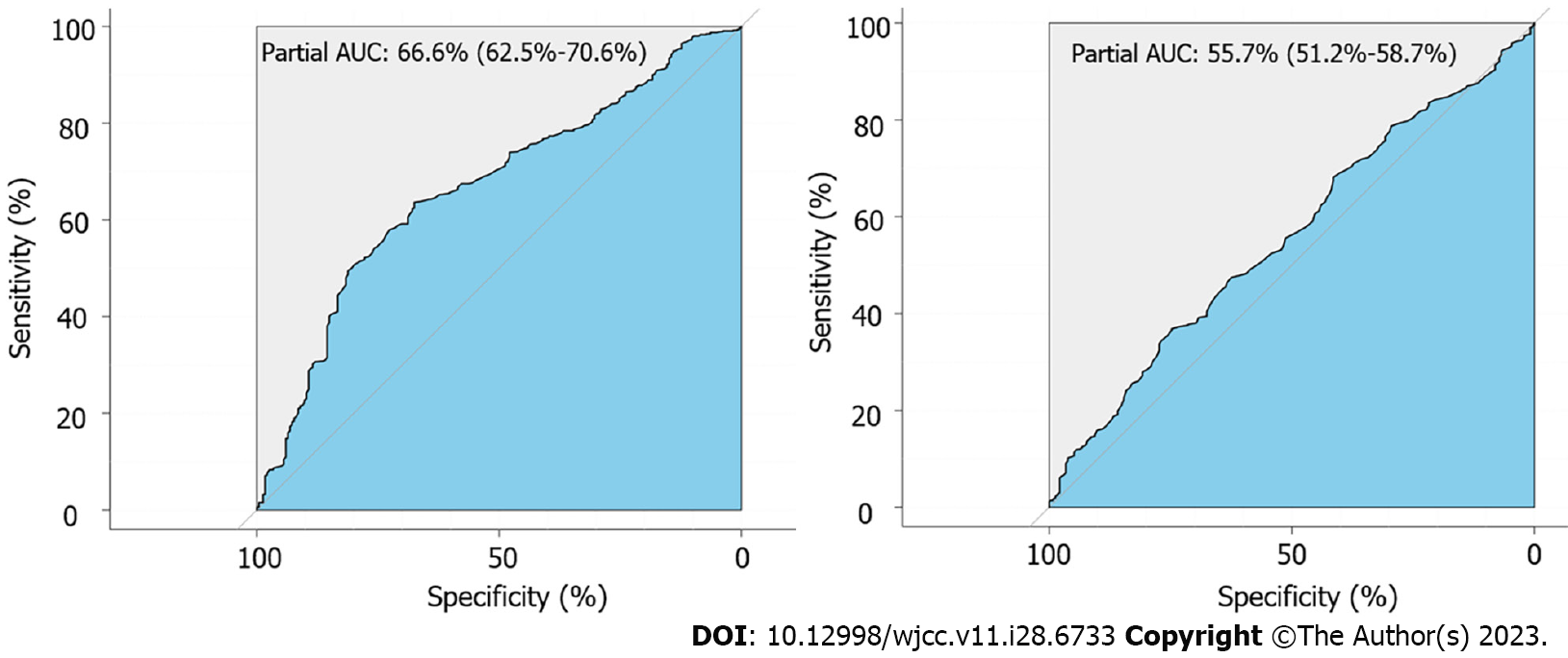
Based on the results of logistic regression, age [odds ratio (OR): 1.33; 95% confidence interval (95%CI): 1.12-1.65; P = 0.0031] and treatment timing (OR: 0.86; 95%CI: 0.75-0.96; P = 0.015) could be considered as the indicators for SFFFH. AVcen (P = 0.0334), AASA (P = 0.0002), NSA (P = 0.0007), and IIA (P = 0.0316) were considered to have statistical significance. Further, AVcen (OR: 1.41; 95%CI: 1.04-1.95) and AASA (OR: 1.44; 95%CI: 1.21-1.77), especially AASA (area under curve: 66.6%), should be paid much more attention due to the higher OR than other indicators.
We have for the first time unveiled that AASA and age could be key risk factors for SFFFH, which further verifies that deficient anterior coverage of the acetabulum might be the main cause of SFFFH.
Core Tip: Our findings indicate that a small anterior acetabular sector angle (AASA) indicates poor anterior coverage of the femoral head and can increase the risk of subchondral fatigue fracture of the femoral head (SFFFH) in young patients. Since patients with a history of intense military training may be at higher risk for SFFFH, early detection and appropriate management are crucial to prevent further deterioration of the femoral head and preserve joint function. Based on these findings, we, therefore, recommend orthopedic surgeons not to exclude the possibility of SFFFH in patients who present with hip pain and have a history of intense military training, particularly if they have a small AASA.
- Citation: Yang JZ, Chen P, Chen BH, Zhao B. Subchondral fatigue fracture of the femoral head in young military recruits: Potential risk factors. World J Clin Cases 2023; 11(28): 6733-6743
- URL: https://www.wjgnet.com/2307-8960/full/v11/i28/6733.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i28.6733
Subchondral fatigue fracture of the femoral head (SFFFH) is rare but occurs in people with vigorous exercise including soldiers and athletes[1,2]. Apart from subchondral insufficiency fracture of the femoral head (SIFFH) secondary to osteoporosis, SFFFH occurs in healthy adults with normal bone quality after repeated abnormal stress or sudden increases in activity[2-4]. SFFFH is characterized by hip pain, limited range of motion, and collapse of the femoral head, similar to the manifestation of osteonecrosis of the femoral head (ONFH)[2,5,6]. At the onset of hip pain, magnetic resonance imaging (MRI) but not X-ray should be performed to detect the lesion[7]. However, there is little research on risk factors related to the occurrence of SFFFH.
Some studies indicated that intrinsic factors are related to SFFFH. Kim DK and Kim TH[8] indicated that the femoral neck-shaft angle (NSA) is associated with the location of the femoral stress fracture after retrospectively studying 37 patients with femoral stress fractures. Iwasaki et al[9] found that both the acetabular head index and band length ratio are important factors in the progression of SIFFH after reviewing 29 patients with this condition. According to the previous observation, we believed that some hip geometry indicators play crucial roles in the development of SFFFH.
In this study, we reviewed 122 patients from the Chinese People's Liberation Army who complained of hip pain to find some characteristics of SFFFH. Furthermore, we aimed to discover some new risk factors for SFFFH by comparing SFFFH with ONFH patients.
The retrospective study was approved by the Ethics Review Board of PLA General Hospital. Patients who underwent hip MRI due to hip pain from June 2013 to June 2019 (n = 2463) in a military tertiary care hospital were identified. These patients were diagnosed with either ONFH (n = 24) or SFFFH (n = 98) based on hip MRI and X-ray. The diagnostic criteria for SFFFH were according to the previous study while those for ONFH were based on the Association Research Circulation Osseous staging system of ONFH[10,11]. All of the clinical records including age, height, weight, and body mass index were extracted from the patient chart.
MRI examinations were performed with a 1.5-T or 3.0-T MR scanner. The standard MRI protocol was used according to a previous study[8]. 1.5-T MRI consisted of axial T1-weighted [repetition time (TR)/echo time (TE) 632/9 ms, 4-mm slice thickness, 0.5-mm gap], axial and coronal T2-weighted (TR/TE 3102/77 ms, 4-mm slice thickness, 0.5-mm gap), and T2-weighted fat saturation (TR/TE 4500/77 ms, 4-mm slice thickness, 0.5-mm gap) sequences through the entire pelvis using a 32-channel body coil. Each sequential field of view (FOV) was 42 cm × 42 cm with a 384 cm × 256 matrix. The protocol of 3.0-T MRI consisted of axial T1-weighted (TR/TE 455/8 ms, 4-mm slice thickness, 0.5-mm gap), axial and coronal T2-weighted fat saturation (TR/TE 4287/81 ms, 4-mm slice thickness, 0.5-mm gap), and coronal short tau inversion recovery sequence (TR/TE 8291/47 ms, inversion time 150 ms, 4-mm slice thickness, 0.5-mm gap) using a 23-channel body coil with a FOV of 41 cm × 41 cm and 416 cm × 288 cm acquisition matrix.
MRI image evaluation was mainly based on bone marrow edema, joint effusion, and cartilage collapse. Besides, acetabular coverage indicators including acetabular anteversion of the superior acetabulum, acetabular anteversion of the center of the acetabulum (AVcen), anterior acetabular sector angle (AASA), posterior acetabular sector angle (PASA), superior acetabular sector angle (SASA), NSA, inferior iliac angle (IIA), and ischiopubic angle were measured three times by two observers independently and blindly (Figure 1).
ONFH and SFFFH were defined as two elements. Then, binary logistic regression was performed to obtain the odds ratio (OR). Independent samples t-test was also performed. The statistical analyses and visualization were performed using the ‘rms’, ‘ggplot2’, ‘ggpubr’, ‘pROC’ packages of R studio (version 1.3.1093).
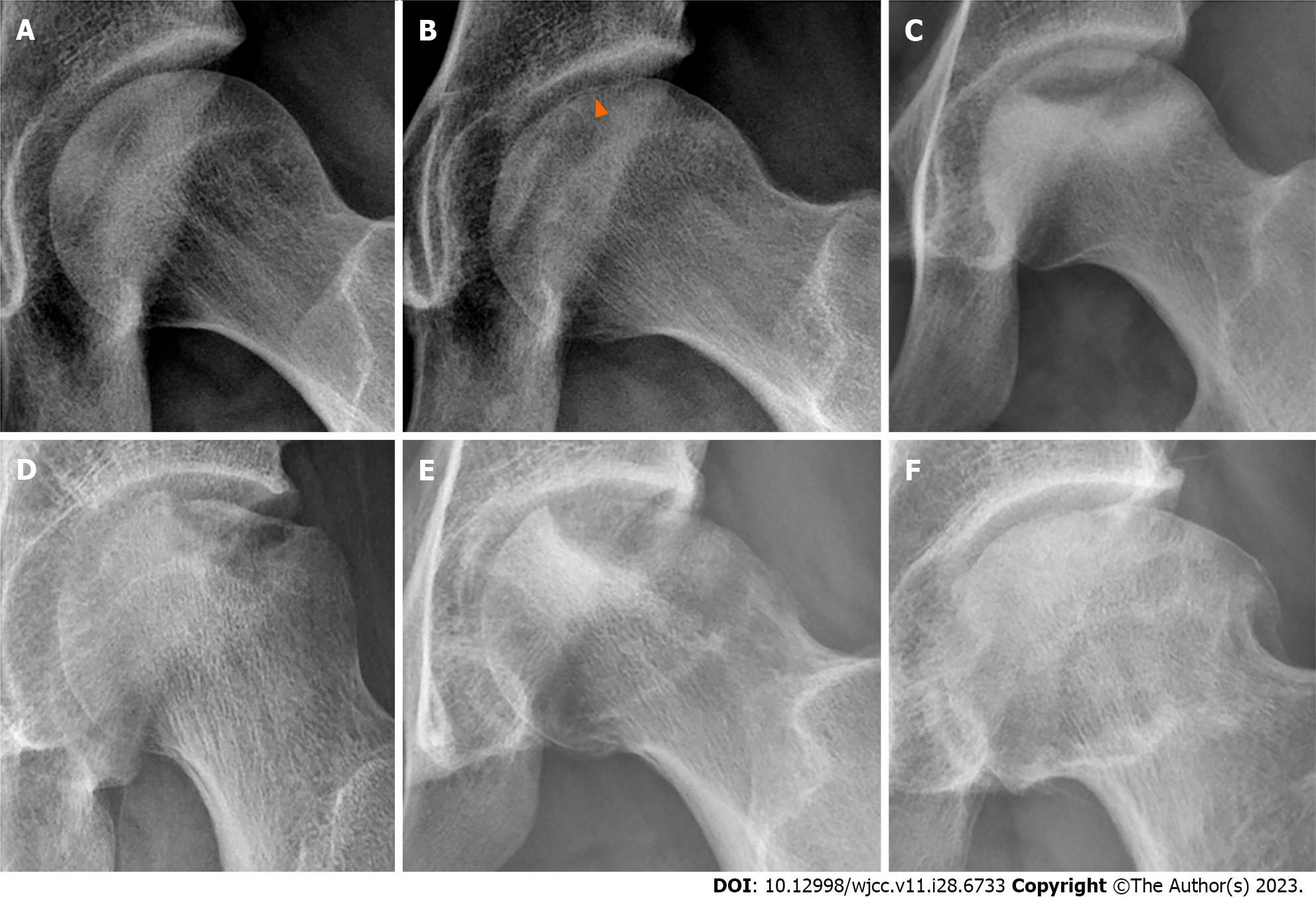
Based on the radiographs of 98 SFFFH patients (108 hips), subchondral fracture lines could be found in 95 hips (88.0%), collapsed bone loss could be found in 52 (48.1%), and sclerotic margin below the fracture lines could be seen in 61 (56.5%). Furthermore, there were 41 hips (38.0%) with mismatched head and mortar and 19 (17.6%) with degenerative change. Figure 2 shows the radiographs of SFFFH patients at different stages. According to the results of MRI, all hips had bone marrow edema, and 96 (88.9%) had joint effusion. All hips were identified with low signal and 94 (87.0%) with discontinued cartilage in T2 weighted images.
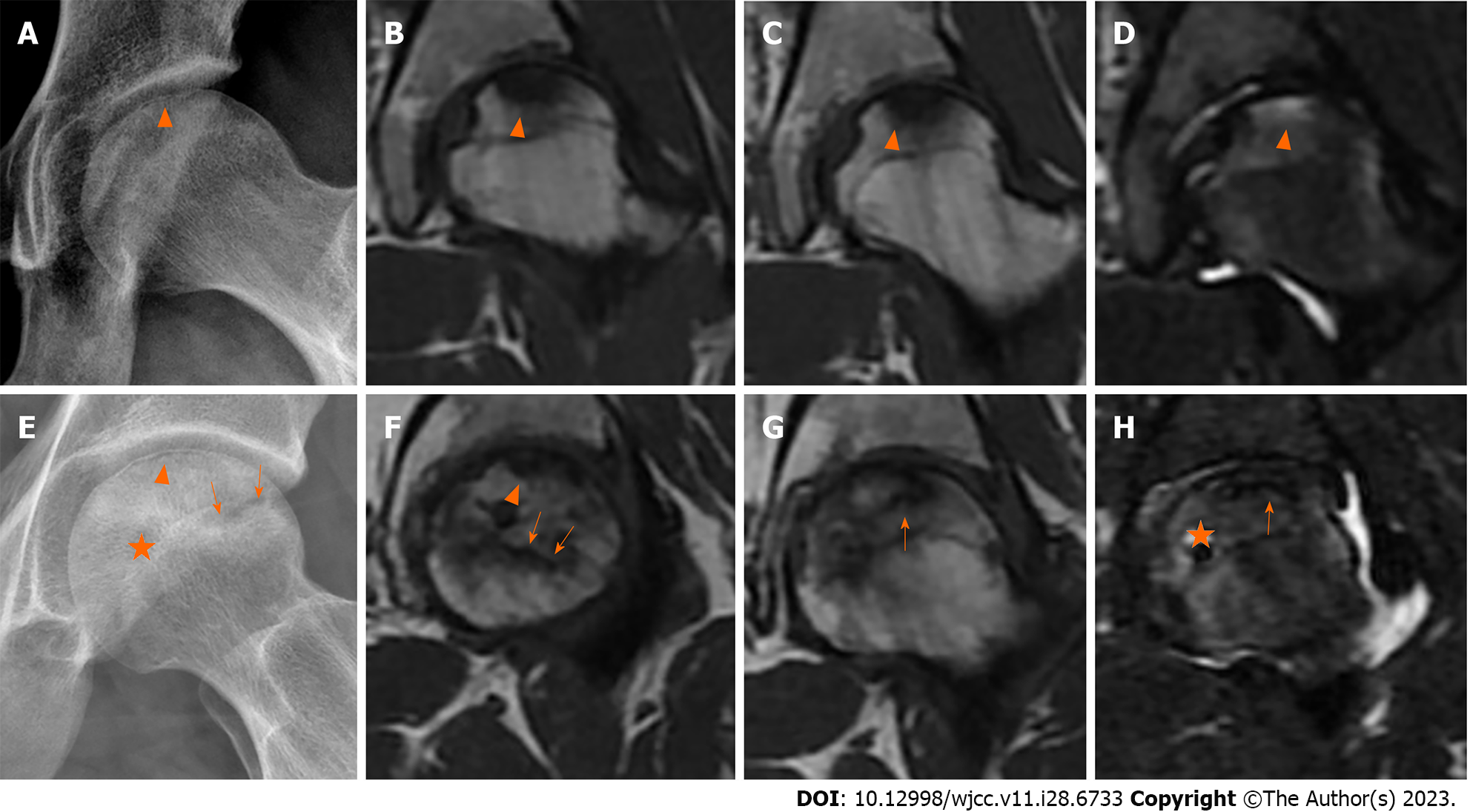
According to the baseline characteristics of 122 patients, we could find that SFFFH patients were younger and they got treatment much later than ONFH patients (Table 1). Most patients with SFFFH were treated later than those with ONFH. And most ONFH patients but none of the SFFFH patients had a history of glucocorticoid or alcoholism. Besides, unlike ONFH that mostly affects bilateral hip joints, SFFFH often involves unilateral hip joints. And SFFFH was more likely to have collapse of the femoral head than ONFH. We show a 19-year-old SFFFH soldier who complained of right hip pain for 3 wk (Figure 3A-D) and a 35-year-old ONFH patient who complained of left hip pain for 6 mo (Figure 3E-H). There was a resemblance between SFFFH and ONFH in the radiographs. Subchondral fracture lines could be found on both patients’ femoral heads (Figure 3A and E). The necrotic zone could be vaguely found on the second patient’s femoral head (Figure 3E). More different appearances could be seen from MRI images. T1-weighted images showed that the hypointense signal was found on the SFFFH patient’s femoral head while an uneven signal was found on the ONFH patient’s whole femoral head (Figure 3B, C, F, and G). T2-weighted images demonstrated that effusion appeared around the fracture line of the SFFFH patient while double line sign and cystic lesions arose on the ONFH patient’s femoral head (Figure 3D and H).
| SFFFH (n = 98) | ONFH (n = 24) | P value | t-value | |
| Age (yr) | 20.3 (17.0-25.0) | 23.0 (18.0-35.0) | 0.0201 | -2.495 |
| Height (cm) | 173.6 (160.0-184.0) | 175.5 (167.0-183.0) | 0.102 | -1.674 |
| Weight (kg) | 65.5 (50.0-90.0) | 68.8 (52.0-90.0) | 0.171 | -1.400 |
| BMI (kg/m2) | 21.7 (17.5-34.5) | 22.3 (16.6-28.4) | 0.436 | -0.790 |
| Treatment timing (mo) | 9.6 (0.6-21.0) | 6.3 (1-36) | 0.0021 | 3.175 |
| History of glucocorticoid use or alcoholism (%) | 0 | 66.7 | / | / |
| Bilateral lesions (%) | 10.2 | 62.5 | / | / |
| Collapse of femoral head (%) | 69.4 | 25 | / | / |
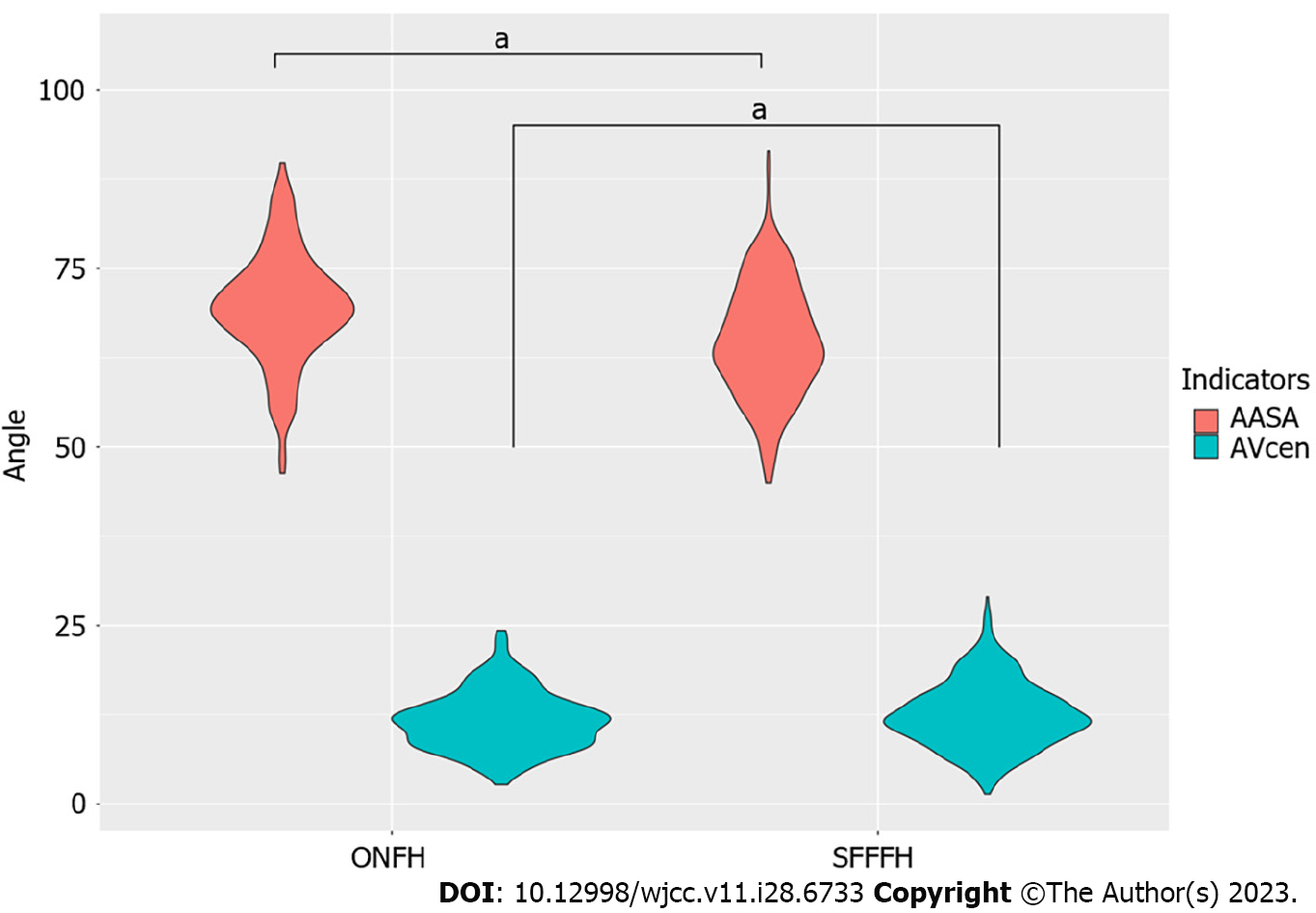
A total of 98 SFFFH patients (108 hips) and 24 ONFH patients (39 hips) were included. All patients participated in a basic-training program that included forced marching with a back-pack, double-time marching, and martial arts. No patient had a history of trauma. Based on the results of logistic regression, we found that age [OR: 1.33; 95% confidence interval (95%CI): 1.12-1.65; P = 0.0031] and treatment timing (OR: 0.86; 95%CI: 0.75-0.96; P = 0.015) could be considered as the indicators for SFFFH (Figure 4). Besides, AVcen (P = 0.0334), AASA (P = 0.0002), NSA (P = 0.0007), and IIA (P = 0.0316) were considered to have statistical significance (Figure 5). Further, AVcen (OR: 1.41; 95%CI: 1.04-1.95) and AASA (OR: 1.44; 95%CI: 1.21-1.77) should be paid much more attention due to the higher OR than other indicators. We constructed receiver operating characteristic curves to assess the predictive performance of AVcen and AASA and found that the area under the curve was 66.6% and 55.7%, respectively, which means that AASA had more predictive significance (Figure 6). Combined with the results of independent samples t-test, we indicated that the AASA of SFFFH was smaller than that of ONFH (Figure 7, Table 2).
| SFFFH (n = 98) | ONFH (n = 24) | P value | t-value | |
| AVsup (°) | 11.7 (11.2-12.3) | 11.4 (10.8-12.1) | 0.498 | 0.678 |
| AVcen (°) | 12.5 (12.2-12.9) | 11.6 (11.1-12.1) | 0.005 | 2.813 |
| AASA (°) | 65.0 (64.3-65.6) | 69.5 (68.5-70.5) | 1.469e-131 | -7.639 |
| PASA (°) | 89.9 (89.3-90.5) | 91.1 (90.0-92.2) | 0.063 | -1.863 |
| SASA (°) | 122.8 (122.4-123.2) | 122.3 (121.5-123.0) | 0.234 | 1.192 |
| NSA (°) | 134.8 (134.4-135.2) | 131.4 (130.9-131.9) | 2.2e-161 | 10.128 |
| IIA (°) | 63.9 (63.5-64.2) | 64.5 (64.0-65.0) | 0.0401 | -2.064 |
| IPA (°) | 31.1 (30.9-31.3) | 30.7 (30.3-31.1) | 0.068 | 1.829 |
SIFFH was considered a kind of pathological fracture due to poor bone quality, which is a disease predominantly affecting elderly patients. Currently, labral tears[12], acetabular over-coverage[13,14], and deficient anterior coverage of the acetabulum[15,16] were considered the risk factors for SIFFH. Uchida et al[12] observed that the acetabular labrum of all nine SIFFH patients were torn via hip arthroscopy. Acetabular over-coverage is one of the manifestations of pincer impingement[17] and usually thought to have high morbidity of femoral acetabular impingement in youth[18]. However, Kimura et al[13] first reported a case of a 53-year-old woman with SIFFH due to acetabular over-coverage. The patient’s bone mineral density was relatively low (T-score: −1.3)[13]. The above previous studies were all based on insufficiency-type fractures but few studies reported that hip geometry could also serve as an intrinsic factor related to fatigue-type fracture in young people, especially in young military recruits.
In 2021, Kim DK and Kim TH[8] first found that NSA is a risk factor associated with SFFFH. The NSA of SFFFH was higher than that of the femoral neck stress fracture (FNSF), which means that a higher NSA might increase the morbidity and severity of SFFFH. On the other hand, previous data by Kuhn et al[19] confirmed that acetabular retroversion is associated with an increased risk of sustaining an FNSF. Franken et al[20] also found that impingement-associated deformities of the hip may cause FNSF. Tokyay et al[21] pointed out that acetabular morphology can predict the types of proximal femoral fractures among elderly patients. NSA of trochanteric fracture was found to be less than that of the femoral neck fracture, but there was no statistically significant difference between them. In our study, the NSA of SFFFH was significantly higher than that of ONFH. However, we cannot identify the clinical significance from the results of logistic regression. Above all, we believe that NSA might be related to SFFFH but NSA cannot cause SFFFH directly.
The acetabular morphology is believed to provide mechanical stability to the hip joint. The morphology of the acetabulum distinctly differs from skeletal maturity. Albers et al[22] found distinct differences of the acetabular version related to skeletal maturity. Version, assessed by MRI, was decreased in hips with open triradiate cartilage complex and increased during skeletal maturation. By contrast, Monazzam et al[23] found that there were no substantial differences in the acetabular version in children younger than 11 years, but a progressive increase of anteversion was noted in patients older than 12 years of age. Hingsammer et al[24] reported decreased anteversion in skeletally immature compared with skeletally mature subjects. However, it should be noted that the data of both studies were derived from computed tomography (CT). CT cannot measure the true dimensions of the acetabulum, while MRI is suitable for accurately measuring the margins of the acetabular wall in both skeletally mature and immature subjects. In our study, clinical data from the new recruits were analyzed by MRI and the age of SFFFH patients was significantly younger than that of ONFH ones. We identified that age was a risk factor for SFFFH based on logistic regression. Younger people are more susceptible to SFFFH. Besides, patients with SFFFH tend to ignore the disease, leading to delayed treatment. Therefore, encouraging high-risk groups to promptly seek medical attention upon the detection of symptoms has been shown to be conducive to a shortened duration of the disease.
We classified the acetabular morphology with a focus on acetabular coverage parameters such as the SASA, AASA, and PASA. None of the patients with SFFFH or ONFH had severe acetabular dysplasia (SASA < 110°). Therefore, the lateral coverage was normal in patients with SFFFH and ONFH. In addition, a PASA of less than 86° is associated with sports-related posterior hip dislocation[25]. In our study, none of the patients with SFFFH or ONFH was found to have a posterior wall defect. Although both the lateral coverage and posterior wall were normal, the AASA of SFFFH patients was smaller than the AASA of ONFH patients, which verified that deficient anterior coverage of the acetabulum should be a risk factor for SFFFH. Deficient anterior coverage of the acetabulum causes SFFFH possibly due to the abnormal stress distributions on the articular weight-bearing area[26]. Hip dysplasia is characterized by shallow acetabulum leading to increased mechanical load on the femoral head and labrum[27]. Henak et al[26] indicated that the labrum under poor coverage supported 2%-10% of the applied load more than the normal labrum by performing subject-specific finite element modeling. However, there is no further study about how poor coverage induces SFFFH. Combining activities beyond the physiologic tolerance level with abnormal mechanical properties of the hip joint, SFFFH might be triggered easily. In the future, more research should focus on the mechanism of deficient anterior coverage causing SFFFH.
MRI is the most essential imaging modality for both patients with SFFFH and ONFH, so the comprehensiveness and accuracy of the retrospective study were guaranteed. We found some evidence about distinguishing SFFFH and ONFH mainly based on MRI findings. First, reactive interface (RI), surrounding the necrotic area, could be mainly seen in ONFH but not in SFFFH. RI, also named sclerosis rim in X-ray or CT, had a protective effect on femoral head collapse[28,29]. Yu et al[30] found that there was a negative correlation between the collapse rate and the proportion of proximal RI. When the proportion is > 30%, the collapse risk is low, whereas at < 30%, the risk is high. Second, cystic lesions, often close to RI in viable areas of the femoral head, could be a common pathologic feature in ONFH but not in SFFFH[31]. Gao et al[32] also observed that the predilection locations of cystic lesions were mainly close to RI in ONFH and the main factor inducing the formation of cystic lesions may be the peak stress at RI edge via an osteoarthritis-like mechanism. Third, the femoral head of SFFFH patients collapses rapidly due to a large amount of joint fluid flowing into the cancellous bone, causing osteocyte death once the cartilage is destroyed. The above three points could explain the observation that the collapse ratio of the femoral head of SFFFH (69.4%) was higher than that of ONFH (25%) in our study. Fourth, SFFFH, unlike ONFH, usually involves the unilateral femoral head.
For those SFFFH patients with pre-collapse lesions, conservative treatment including non-weight bearing with crutches and non-steroidal anti-inflammatory agents should be performed[33]. Patients with collapse lesions can be divided into two groups: Non-progression of collapse and progressive collapse with a diversity of etiologies. It is difficult to highlight reasons for collapse of the femoral head on imaging in some patients. Besides, variation of recovery or worsening could be found even among similar etiological cohorts[34]. Once the femoral head progressed to collapse following the loss of the articular bony margin or arthritic change, their prognosis seemed to be the radiological findings in rapidly destructive arthrosis of the hip joint (RDA)[7,35]. Kubo et al[36] found that tartrate-resistant acid phosphatase 5b, a specific bone resorption marker associated with osteoclast cells, reflects the condition of progressive collapse in SIFFH as well as RDA. Due to high activity levels in SFFFH patients, hip preservation techniques, such as transtrochanteric anterior rotational osteotomy, have been recommended by many previous studies[37,38].
Taken together, we have, for the first time, identified AASA as a risk factor for SFFFH, which means that deficient anterior coverage of the acetabulum could induce SFFFH directly. Besides, young people, especially those with a history of intense training, are at higher risk for SFFFH. We advocate for the dissemination of scientific knowledge amongst high-risk populations in order to promote timely intervention in cases of SFFFH. However, we only compared the indicators of SFFFH and ONFH, and healthy people need to be included to solidify the results.
Osteoporosis was considered the main risk factor for hip fracture. However, hip fractures can also occur in young patients with no osteoporosis. Although several studies have reported on insufficiency-type fractures of the femur, there are limited reports on the impact of hip geometry on fatigue-type femoral fractures in young individuals, particularly in young military recruits.
Subchondral fatigue fracture of the femoral head (SFFFH) mainly occurs in young military recruits and might be confused with osteonecrosis of the femoral head. However, less research focuses on the risk factor for SFFFH.
Our study aimed to identify the intrinsic risk factors for SFFFH in young Chinese military recruits.
X-ray and magnetic resonance imaging data were used for analysis. And logistic regression, receiver operating characteristic curve analysis, and independent samples t-test were performed to identify the risk factors for SFFFH.
Overall, our findings indicate that a small anterior acetabular sector angle (AASA) indicates poor anterior coverage of the femoral head and can increase the risk of SFFFH in young patients. Since patients with a history of intense military training may be at higher risk for SFFFH, early detection and appropriate management are crucial to prevent further deterioration of the femoral head and preserve joint function.
Based on the findings of the study, we recommend orthopedic surgeons not to exclude the possibility of SFFFH in patients who present with hip pain and have a history of intense military training, particularly if they have a small AASA.
We advocate for the dissemination of scientific knowledge amongst high-risk populations in order to promote timely intervention in cases of SFFFH.
| 1. | Lee S, Kim HJ, Yoo JJ. Factors Affecting the Clinical Course of Subchondral Fatigue Fracture of the Femoral Head. Clin Orthop Surg. 2023;15:203-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 2. | Yoon HK, Choi MH, Lee H, Park J, Ahn J. Subchondral stress fracture of the femoral head (SSFFH) in young and healthy military recruits: clinical recommendations and fracture configurations on MRI. Int Orthop. 2023;47:1315-1321. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Lee YK, Won SH, Park JW, Im JW, Ha YC, Koo KH. Cementless Hip Arthroplasty in Patients with Subchondral Insufficiency Fracture of the Femoral Head. J Bone Joint Surg Am. 2022;104:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 4. | Lee YJ, Kim YG. Subchondral insufficiency fracture of the femoral head in a patient with ankylosing spondylitis: Case report and literature review. Int J Rheum Dis. 2023;26:1599-1602. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Kawano K, Motomura G, Ikemura S, Yamaguchi R, Baba S, Xu M, Nakashima Y. Differences in the microarchitectural features of the lateral collapsed lesion between osteonecrosis and subchondral insufficiency fracture of the femoral head. Bone. 2020;141:115585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Chen M, Wang X, Takahashi E, Kaneuji A, Zhou Y, Kawahara N. Current Research on Subchondral Insufficiency Fracture of the Femoral Head. Clin Orthop Surg. 2022;14:477-485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Yamamoto T, Schneider R, Bullough PG. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol. 2001;30:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 106] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Kim DK, Kim TH. Femoral neck shaft angle in relation to the location of femoral stress fracture in young military recruits: femoral head vs femoral neck stress fracture. Skeletal Radiol. 2021;50:1163-1168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Iwasaki K, Yamamoto T, Motomura G, Ikemura S, Yamaguchi R, Iwamoto Y. Radiologic measurements associated with the prognosis and need for surgery in patients with subchondral insufficiency fractures of the femoral head. AJR Am J Roentgenol. 2013;201:W97-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Song WS, Yoo JJ, Koo KH, Yoon KS, Kim YM, Kim HJ. Subchondral fatigue fracture of the femoral head in military recruits. J Bone Joint Surg Am. 2004;86:1917-1924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Yoon BH, Mont MA, Koo KH, Chen CH, Cheng EY, Cui Q, Drescher W, Gangji V, Goodman SB, Ha YC, Hernigou P, Hungerford MW, Iorio R, Jo WL, Jones LC, Khanduja V, Kim HKW, Kim SY, Kim TY, Lee HY, Lee MS, Lee YK, Lee YJ, Nakamura J, Parvizi J, Sakai T, Sugano N, Takao M, Yamamoto T, Zhao DW. The 2019 Revised Version of Association Research Circulation Osseous Staging System of Osteonecrosis of the Femoral Head. J Arthroplasty. 2020;35:933-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 202] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 12. | Uchida S, Noguchi M, Utsunomiya H, Kanezaki S, Mori T, Matsuda DK, Sakai A. Hip arthroscopy enables classification and treatment of precollapse subchondral insufficiency fracture of the femoral head associated intra-articular pathology. Knee Surg Sports Traumatol Arthrosc. 2018;26:2527-2535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Kimura T, Goto T, Hamada D, Tsutsui T, Wada K, Fukuta S, Nagamachi A, Sairyo K. Subchondral Insufficiency Fracture of the Femoral Head Caused by Excessive Lateralization of the Acetabular Rim. Case Rep Orthop. 2016;2016:4371679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Sutter R, Pfirrmann CW. Atypical hip impingement. AJR Am J Roentgenol. 2013;201:W437-W442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 15. | Jo WL, Lee WS, Chae DS, Yang IH, Lee KM, Koo KH. Decreased Lumbar Lordosis and Deficient Acetabular Coverage Are Risk Factors for Subchondral Insufficiency Fracture. J Korean Med Sci. 2016;31:1650-1655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Kubo Y, Motomura G, Utsunomiya T, Fujii M, Ikemura S, Sonoda K, Nakashima Y. Distribution of Femoral Head Subchondral Fracture Site Relates to Contact Pressures, Age, and Acetabular Structure. AJR Am J Roentgenol. 2020;215:448-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Tannenbaum EP, Zhang P, Maratt JD, Gombera MM, Holcombe SA, Wang SC, Bedi A, Goulet JA. A Computed Tomography Study of Gender Differences in Acetabular Version and Morphology: Implications for Femoroacetabular Impingement. Arthroscopy. 2015;31:1247-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Kapron AL, Anderson AE, Aoki SK, Phillips LG, Petron DJ, Toth R, Peters CL. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93:e111(1-e1110). [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 173] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 19. | Kuhn KM, Riccio AI, Saldua NS, Cassidy J. Acetabular retroversion in military recruits with femoral neck stress fractures. Clin Orthop Relat Res. 2010;468:846-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Franken L, Goronzy J, Olusile OO, Slullitel PA, Blum S, Nowotny J, Hartmann A, Thielemann F, Günther KP. [Femoral neck stress fractures and femoroacetabular impingement : A retrospective case study and literature review]. Orthopade. 2021;50:224-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Tokyay A, Güven M, Encan ME, Okay E, Akbaba O. The influence of acetabular morphology on prediction of proximal femur fractures types in an elderly population. Hip Int. 2017;27:489-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Albers CE, Schwarz A, Hanke MS, Kienle KP, Werlen S, Siebenrock KA. Acetabular Version Increases After Closure of the Triradiate Cartilage Complex. Clin Orthop Relat Res. 2017;475:983-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Monazzam S, Bomar JD, Dwek JR, Hosalkar HS, Pennock AT. Development and prevalence of femoroacetabular impingement-associated morphology in a paediatric and adolescent population: a CT study of 225 patients. Bone Joint J. 2013;95-B:598-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 24. | Hingsammer AM, Bixby S, Zurakowski D, Yen YM, Kim YJ. How do acetabular version and femoral head coverage change with skeletal maturity? Clin Orthop Relat Res. 2015;473:1224-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 25. | Novais EN, Ferrer MG, Williams KA, Bixby SD. Acetabular Retroversion and Decreased Posterior Coverage Are Associated With Sports-related Posterior Hip Dislocation in Adolescents. Clin Orthop Relat Res. 2019;477:1101-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Henak CR, Ellis BJ, Harris MD, Anderson AE, Peters CL, Weiss JA. Role of the acetabular labrum in load support across the hip joint. J Biomech. 2011;44:2201-2206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 142] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 27. | Gala L, Clohisy JC, Beaulé PE. Hip Dysplasia in the Young Adult. J Bone Joint Surg Am. 2016;98:63-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 201] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 28. | Yu T, Xie L, Chu F. A sclerotic rim provides mechanical support for the femoral head in osteonecrosis. Orthopedics. 2015;38:e374-e379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Chen Y, Miao Y, Liu K, Zhu B, Xue F, Yin J, Zou J, Li G, Zhang C, Feng Y. Less sclerotic microarchitecture pattern with increased bone resorption in glucocorticoid-associated osteonecrosis of femoral head as compared to alcohol-associated osteonecrosis of femoral head. Front Endocrinol (Lausanne). 2023;14:1133674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 30. | Yu T, Xie L, Zhang Z, Ke X, Liu Y. Prediction of osteonecrosis collapse of the femoral head based on the proportion of the proximal sclerotic rim. Int Orthop. 2015;39:1045-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Kim J, Lee SK, Kim JY, Kim JH. CT and MRI findings beyond the subchondral bone in osteonecrosis of the femoral head to distinguish between ARCO stages 2 and 3A. Eur Radiol. 2023;33:4789-4800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 32. | Gao F, Han J, He Z, Li Z. Radiological analysis of cystic lesion in osteonecrosis of the femoral head. Int Orthop. 2018;42:1615-1621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 33. | Di Martino A, Brunello M, Villari E, Cataldi P, D'Agostino C, Faldini C. Bone marrow edema of the hip: a narrative review. Arch Orthop Trauma Surg. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 34. | Gaudiani MA, Samuel LT, Mahmood B, Sultan AA, Kamath AF. Subchondral insufficiency fractures of the femoral head: systematic review of diagnosis, treatment and outcomes. J Hip Preserv Surg. 2020;7:85-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Kim SM, Oh SM, Cho CH, Lim SJ, Moon YW, Choi SH, Park YS. Fate of subchondral fatigue fractures of femoral head in young adults differs from general outcome of fracture healing. Injury. 2016;47:2789-2794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Kubo Y, Motomura G, Ikemura S, Hatanaka H, Fukushi JI, Hamai S, Yamamoto T, Nakashima Y. Osteoclast-related markers in the hip joint fluid with subchondral insufficiency fracture of the femoral head. J Orthop Res. 2018;36:2987-2995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Sonoda K, Motomura G, Ikemura S, Kubo Y, Yamamoto T, Nakashima Y. Favorable Clinical and Radiographic Results of Transtrochanteric Anterior Rotational Osteotomy for Collapsed Subchondral Insufficiency Fracture of the Femoral Head in Young Adults. JB JS Open Access. 2017;2:e0013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | Miyake Y, Mitani S. Subchondral fatigue fracture of the femoral head with acetabular dysplasia treated by transposition osteotomy of the acetabulum: a case report. J Orthop Case Rep. 2023;13:82-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mahmoud MZ, Saudi Arabia S-Editor: Lin C L-Editor: Wang TQ P-Editor: Yu HG