Published online Sep 26, 2023. doi: 10.12998/wjcc.v11.i27.6573
Peer-review started: June 30, 2023
First decision: August 9, 2023
Revised: August 23, 2023
Accepted: September 4, 2023
Article in press: September 4, 2023
Published online: September 26, 2023
Processing time: 82 Days and 7.3 Hours
Overhanging filtering bleb is a common complication after trabeculectomy and surgical repair is an effective treatment when the patient presents with apparent symptoms. Filtering bleb relevant infection including in the filtering bleb itself and even endophthalmitis in some severe cases has been reported. However, cor
A 57-year-old Chinese man who had sensations of redness and foreign body sen
In addition to avoiding the development of overhanging filtering bleb after tra
Core Tip: Overhanging filtering bleb is a common complication after trabeculectomy. Filtering bleb relevant infection inclu
- Citation: Zhao J, Xu HT, Yin Y, Li YX, Zheng YJ. Fungal corneal ulcer after repair of an overhanging filtering bleb: A case report. World J Clin Cases 2023; 11(27): 6573-6578
- URL: https://www.wjgnet.com/2307-8960/full/v11/i27/6573.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i27.6573
An overhanging filtering bleb is a common complication after trabeculectomy, and surgical repair is an effective trea
A 57-year-old Chinese man was admitted to the Second Hospital of Jilin University due to sensations of redness and foreign body sensations in the left eye.
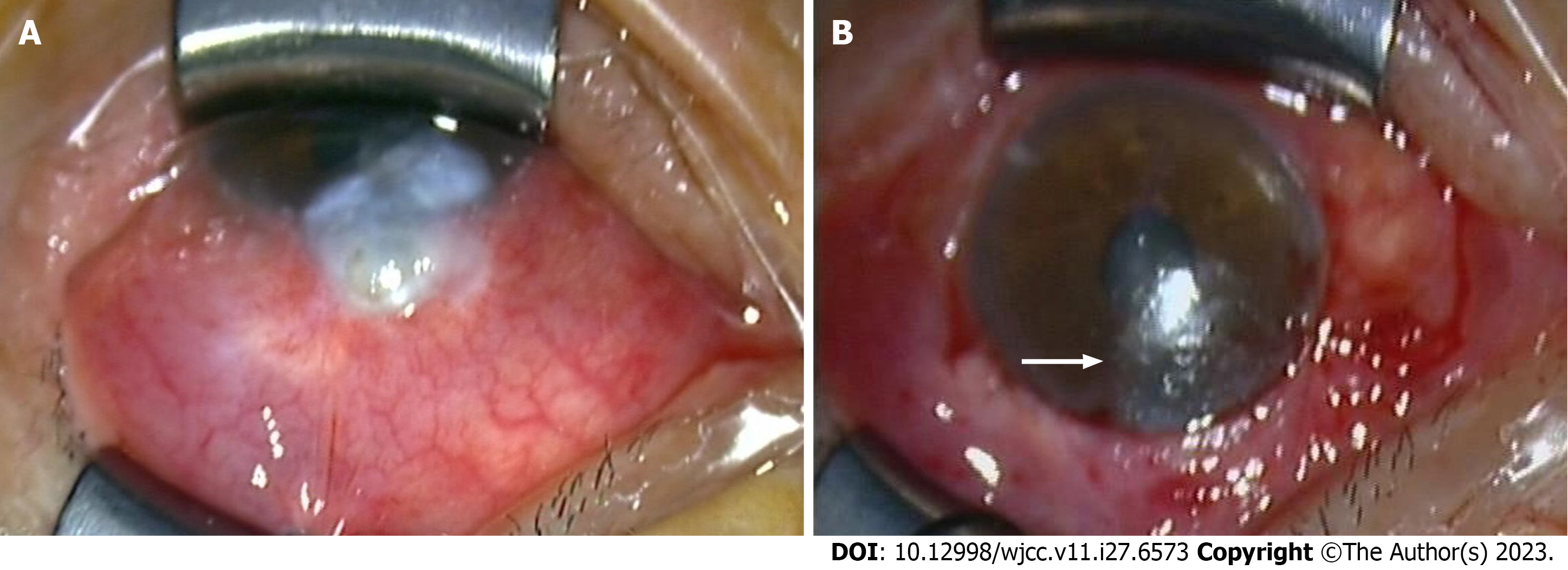
The patient was came to our hospital 3 wk ago due to sensations of a foreign body in the left eye for 3 years with wor
Six years earlier, he had been diagnosed with chronic angle-closure glaucoma of the left eye, which resulted in optic atrophy. He underwent trabeculectomy of the left eye under local anaesthesia without complications. After surgery, the patient was examined every 3 mo for 1 year. His intraocular pressure (IOP) was normal (11-16 mmHg in the left eye), and the mean area of visual field damage remained stable.
There is none history of personal and family.
Slit lamp examination revealed mild conjunctival hyperaemia and rough upper corneal surfaces. However, the repaired filtering bleb was formed well, flat and diffuse with no remarkable changes be observed, and the IOP remained normal (13 mmHg). Therefore, the patient was instructed to apply topical antibiotic eye drops. One week later, the patient presented with redness, pain accompanied by severely deterioration in vision. His best-corrected visual acuity in the left eye was reduced to finger count. Slit lamp examination revealed a grey infiltrate of the cornea.
A routine haematology examination was performed before overhanging filtering bleb repair surgery, including routine blood tests, routine urine tests, liver and kidney function tests, coagulation tests and immune tests. The results were almost normal. On ophthalmic examination, a large amount of mycelium was visible under confocal microscopy.
There is none imaging examination.
Fungal keratitis.
An anti-fungal treatment was administered immediately (natamycin eye drops every hour, levofloxacin eye drops every 2 h, and compound tropicamide eye drops four times daily).
At this time, the patient disclosed that he had been using glucocorticoid eye drops (tobramycin dexamethasone) for the past 3 years to relieve foreign body sensation in the left eye. Because the glucocorticoid eye drops he had used 6 years prior (after the trabeculectomy) provided normal sensation to the eye.
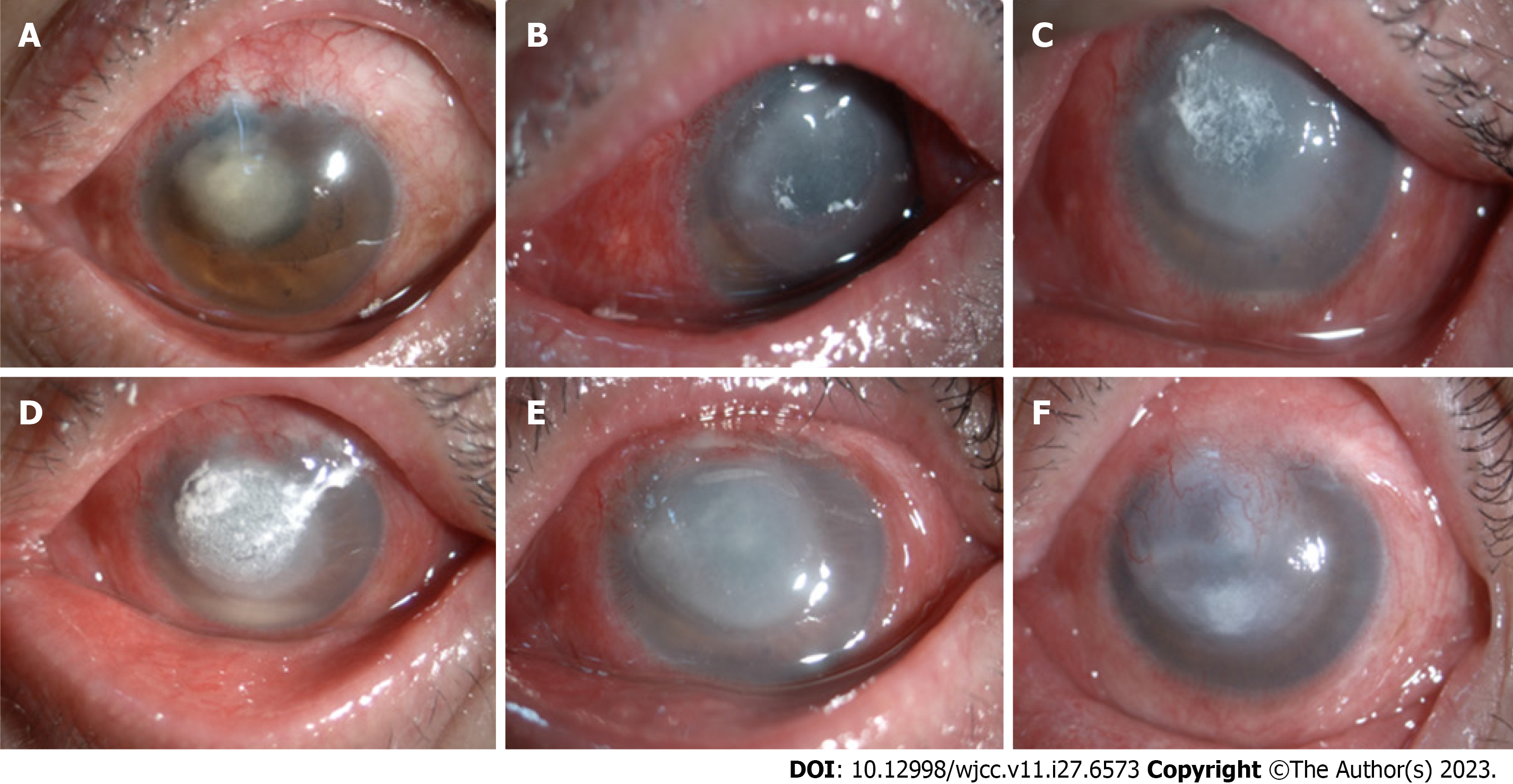
The course of the fungal corneal infection is shown in Figure 2. The infection started with a grey infiltrate with irregular white edges, and then corneal ulcers formed, and hypopyon appeared. The corneal ulcer and hypopyon lasted for a long time, until the 10th wk after the operation. The corneal ulcer began to improve, and the hypopyon was gradually absorbed. After 3 mo of anti-fungal treatment, the inflammation was well controlled and the ulcers had healed. Corneal neovascularization and leucoma were also observed. The patient’s best-corrected visual acuity was decreased to hand movements. However, the filtering bleb is still flat and diffuse with no signs of infection, and the IOP in the left eye was stable.
Overhanging filtering bleb is primarily caused by excessive filtration. The filtering bleb is too large, especially in patients with a thin conjunctiva. Gravity may cause the bleb to droop and invade the cornea (epidermal to Bowman membrane). In cases of mild overhang, the bleb does not leak, and patients present with few to no symptoms. In such cases, conservative treatment is generally recommended in the form of lubricating eye drops (i.e., artificial tears). However, surgical treatment should be considered when a risk of leakage exists or when patients experiences bleb dysesthesia[3].
Several studies have reported that filtering bleb infection may occur after anti-glaucoma surgery[4,5]. Intraocular inflammation has been observed in some severe cases. However, no previous studies have reported the occurrence of a fungal infection of the cornea after filtering bleb repair. Moreover, changes in the morphology and filtration are expected to occur after a filter bleb-related infection; however, no such changes were observed in the present case and the IOP remained stable in the affected eye. The patient’s symptoms began during the 3rd wk after filtering bleb repair, which was consistent with the common incubation period for postoperative fungal infections[6]. Therefore, we speculated that the fungal infection was not directly caused by surgery, but by the creation of a corneal epithelial defect during the removal of the prolapsed filtering bleb tissue, thereby providing the conditions necessary for the growth and expansion of a fungal infection.
In addition to the above reasons of excessive filtration, thinning of the conjunctiva and effects of gravity, the etiology of filtering bleb invasion of the cornea also includes the use of mitomycin C during trabeculectomy which could injury the conjunctival tissue and corneal limbus[3,7]. Dissolution of the aqueous humour from the overhanging filtering bleb to the corneal surface may result in corneal epithelium loss, matrix degeneration[8,9], and chronic and persistent weak inflammatory responses[10,11], which potentially lead to corneal tissue degeneration, hyperplasia, and fusion[12].
Regarding fungal infection of the cornea, although we do not have direct evidence of the reason for the infection, which is the biggest limitation of this study, all the evidence suggests that the main reason for infection is the long-term use of glucocorticoid eye drops. Surgically induced corneal epithelial defects provide the necessary conditions for the fungal infections. Even in healthy people, parasitic fungi have been observed in the conjunctival sac, with carrier rates for the 42 known strains ranging from 5%-83%[13,14]. However, fungal eye infections are rarely primary infections because organic and environmental factors affect the occurrence and development of infections to varying degrees[15]. Imba
Glucocorticoids may promote fungal growth by exerting inhibitory effects on multiple immune-related processes, and their long-term use inhibits neutrophil chemotaxis and macrophage phagocytosis. In addition, glucocorticoids inhibit protein synthesis, promote protein degradation, delay granulation tissue formation, prolong the repair cycle of corneal epithelial cells, and promote the growth and reproduction of fungi[16]. The thickness of the mycelial wall of the fungus invading the corneal stroma has been shown to increase by 2-3-fold, and the mycelial structure of the mycelium sheath appears after the application of dexamethasone[17]. Moreover, conjunctival sac cultures were positive for fungi in 67% of 63 eyes treated with corticosteroid eye drops compared to 18% in the control group[18].
Glucocorticoid eye drops comprise one of the most commonly used and effective treatments for ocular inflammation. However, long-term use can cause serious side effects. When the side effects of the long-term use of glucocorticoids are mentioned, we usually focus on their ability to increase the intraocular pressure or induction of the formation of se
In addition to avoiding the development of overhanging filtering bleb after trabeculectomy, the present case report also suggests that clinicians should pay more attention to the patient’s preoperative history of ocular self-medication, particularly in patients with a history of glaucoma or eye surgery. Because these patients may be exposed to more types of eye drops than other individuals, they may select the wrong medications for long-term use based on their previous expe
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rotondo JC, Italy S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Mac I, Soltau JB. Glaucoma-filtering bleb infections. Curr Opin Ophthalmol. 2003;14:91-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Yamamoto T, Sawada A, Mayama C, Araie M, Ohkubo S, Sugiyama K, Kuwayama Y; Collaborative Bleb-Related Infection Incidence and Treatment Study Group. The 5-year incidence of bleb-related infection and its risk factors after filtering surgeries with adjunctive mitomycin C: collaborative bleb-related infection incidence and treatment study 2. Ophthalmology. 2014;121:1001-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 99] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Lanzl IM, Katz LJ, Shindler RL, Spaeth GL. Surgical management of the symptomatic overhanging filtering bleb. J Glaucoma. 1999;8:247-249. [PubMed] |
| 4. | Sawada A, Kuwayama Y, Yamamoto T. Changes in filtering bleb morphology after bleb-related infection. Jpn J Ophthalmol. 2015;59:312-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Yamamoto T, Kuwayama Y; Collaborative Bleb-related Infection Incidence and Treatment Study Group. Interim clinical outcomes in the collaborative bleb-related infection incidence and treatment study. Ophthalmology. 2011;118:453-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Henry MW, Miller AO, Walsh TJ, Brause BD. Fungal Musculoskeletal Infections. Infect Dis Clin North Am. 2017;31:353-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | Peng YJ, Pan CY, Hsieh YT, Wu S, Chu HN, Hsu WC. The application of tissue engineering in reversing mitomycin C-induced ischemic conjunctiva. J Biomed Mater Res A. 2012;100:1126-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Lim SH, Unoki N, Cha SC. Immunohistopathologic features of surgically excised overhanging filtering bleb: myofibroblasts after filtration surgery--a case report. Graefes Arch Clin Exp Ophthalmol. 2014;252:1171-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 9. | Ulrich GG, Proia AD, Shields MB. Clinicopathologic features and surgical management of dissecting glaucoma filtering blebs. Ophthalmic Surg Lasers. 1997;28:151-155. [PubMed] |
| 10. | Rotondo JC, Mazziotta C, Lanzillotti C, Stefani C, Badiale G, Campione G, Martini F, Tognon M. The Role of Purinergic P2X7 Receptor in Inflammation and Cancer: Novel Molecular Insights and Clinical Applications. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 72] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 11. | Suzuki K. Chronic Inflammation as an Immunological Abnormality and Effectiveness of Exercise. Biomolecules. 2019;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 209] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 12. | Ou-Yang PB, Qi X, Duan XC. Histopathology and treatment of a huge overhanging filtering bleb. BMC Ophthalmol. 2016;16:175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Klotz SA, Penn CC, Negvesky GJ, Butrus SI. Fungal and parasitic infections of the eye. Clin Microbiol Rev. 2000;13:662-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 120] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Ando N, Takatori K. Fungal flora of the conjunctival sac. Am J Ophthalmol. 1982;94:67-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Segal E, Romano A, Eylan E, Stein R. Fungal flora of the normal conjunctival sac. Mykosen. 1977;20:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Hasany SM, Basu PK, Kazdan JJ. Production of corneal ulcer by opportunistic and saprophytic fungi. 1. The effect of pretreatment of fungi with steroid. Can J Ophthalmol. 1973;8:119-131. [PubMed] |
| 17. | Kiryu H, Yoshida S, Suenaga Y, Asahi M. Invasion and survival of Fusarium solani in the dexamethasone-treated cornea of rabbits. J Med Vet Mycol. 1991;29:395-406. [PubMed] |
| 18. | Mitsui Y, Hanabusa J. Corneal infections after cortisone therapy. Br J Ophthalmol. 1955;39:244-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 94] [Article Influence: 4.1] [Reference Citation Analysis (0)] |