Published online Sep 6, 2023. doi: 10.12998/wjcc.v11.i25.5863
Peer-review started: March 30, 2023
First decision: July 3, 2023
Revised: July 5, 2023
Accepted: August 3, 2023
Article in press: August 3, 2023
Published online: September 6, 2023
Processing time: 154 Days and 19.2 Hours
Closed reduction and internal fixation with intramedullary nails has been widely accepted for treating intertrochanteric fractures.
To focus on how to avoid displacement of the lesser trochanter in unstable in
We developed a lesser trochanteric reduction fixator for treating intertrochanteric fractures through fixing the lesser trochanter by combining the loop plate through the fixator after reduction by the reducer. Five patients with intertrochanteric fractures treated with the newly developed lesser trochanteric reduction fixator and loop plate combined with intramedullary nails, and 20 patients with in
The postoperative Harris hip score was significantly higher in patients treated with the lesser trochanteric reduction fixator than in patients treated without the lesser trochanteric reduction fixator, which indicated that this lesser trochanteric reduction fixator had a positive impact on rehabilitation of the hip joint after surgery and could significantly improve the quality of life of patients.
We fully realize the significance of trochanteric reduction and fixation, namely, reconstruction of structures under pressure, in the treatment of intertrochanteric fractures. As long as the general condition of patients is favorable and they are willing to undergo surgery, fixation of the main fracture end should be performed and the lesser trochanter should be reduced and fixed at the same time.
Core Tip: After reliable reduction and fixation, a newly developed lesser trochanteric reduction fixator can be introduced into the loop plate through the customized holes, and the loop plate can pass through the muscle space of the lesser trochanter, which can achieve the reduction and fixation of the lesser trochanter. This fixator can improve the quality of reducing the lesser trochanter, and the loop plate can achieve elastic fixation. There is no risk of nail breakage caused by nail fixation.
- Citation: Hui YM, Zeng G, Liu PY, Chai B. Application of lesser trochanteric reduction fixator in the treatment of unstable intertrochanteric fractures. World J Clin Cases 2023; 11(25): 5863-5869
- URL: https://www.wjgnet.com/2307-8960/full/v11/i25/5863.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i25.5863
As the population ages, an increase in the incidence of low-energy injuries, such as intertrochanteric fractures induced by trauma-related osteoporosis, has been reported. Based on the Evans classification system, an intertrochanteric fracture can be categorized into the following five types[1]: (1) Type I: Syn-intertrochanteric fractures; non-displaced, stable fractures that account for 11.1% of all intertrochanteric fractures; (2) Type II: Lesser trochanteric fractures, showing mild displacement and stable reduction; stable fractures that account for 17.4% of all intertrochanteric fractures; (3) Type III: Lesser trochanteric comminuted fractures, with the absence of stable reduction; unstable fractures that account for 45.1% of all intertrochanteric fractures; (4) Type IV: Type III combined with greater trochanteric fractures; unstable fractures that account for 20.1% of all intertrochanteric fractures; and (5) Type V: Reverse intertrochanteric fractures, showing a tendency for displacement due to traction of the adductor; unstable fractures which account for 6.3% of all inter
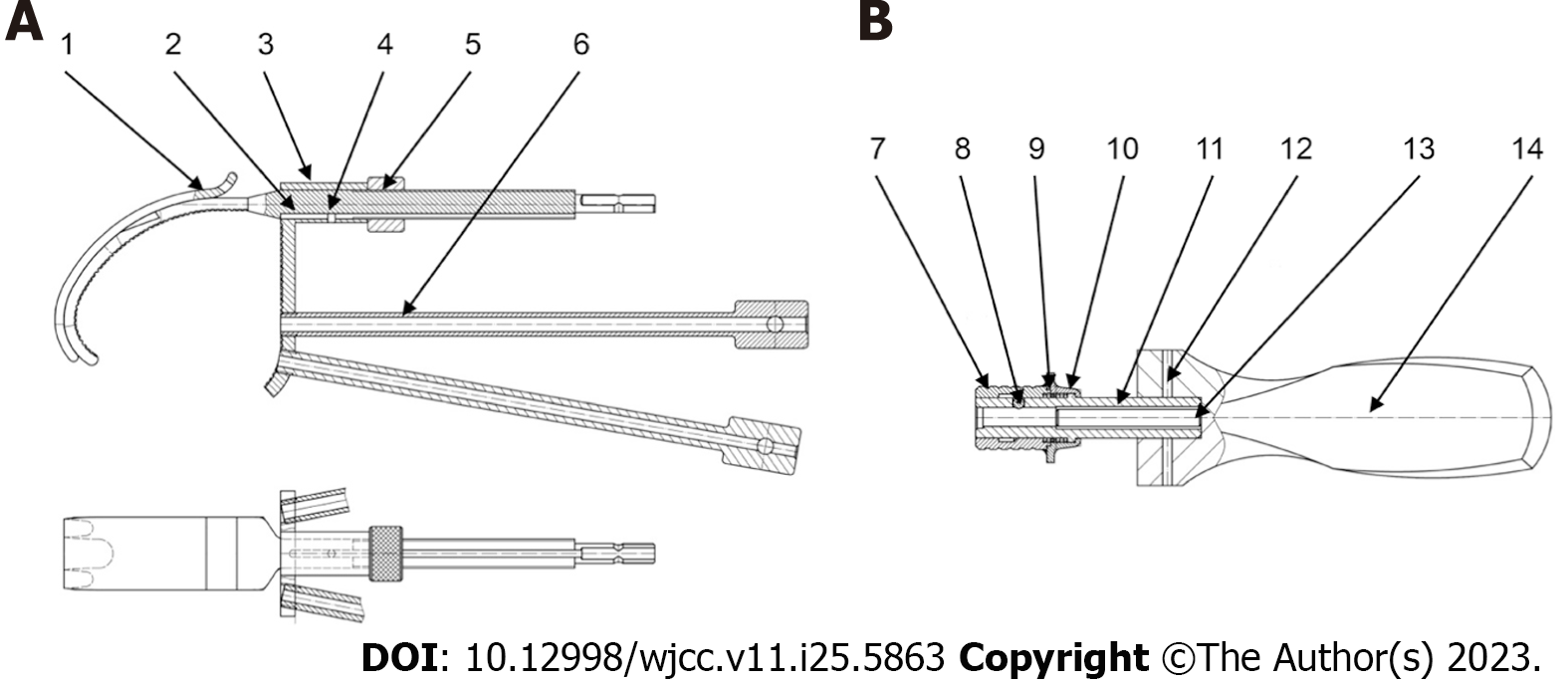
After consulting the relevant literature and conducting explorations in clinical practice, we developed a lesser trochanteric reduction fixator for treating intertrochanteric fractures through fixing the lesser trochanter by combining the loop plate through the fixator after reduction by the reducer (Figure 1A and B).
We have applied for a patent for the lesser trochanteric reduction fixator for intertrochanteric fractures to the China National Intellectual Property Administration (No. 202122899022.4).
Five patients with intertrochanteric fractures treated with the newly developed lesser trochanteric reduction fixator and loop plate combined with intramedullary nails, and 20 patients with intertrochanteric fractures treated with simple intramedullary nails were selected from December 2020 to March 2021 for a 6-mo follow-up comparison.
Preoperative preparation: Before surgery, all patients underwent complete routine auxiliary examinations. Data collection, measurement, and classification of X-ray and computed tomography imaging of the hip joint were performed. Besides, the diagnosis and treatment of patients complicated with internal medicine diseases were also conducted whenever necessary.
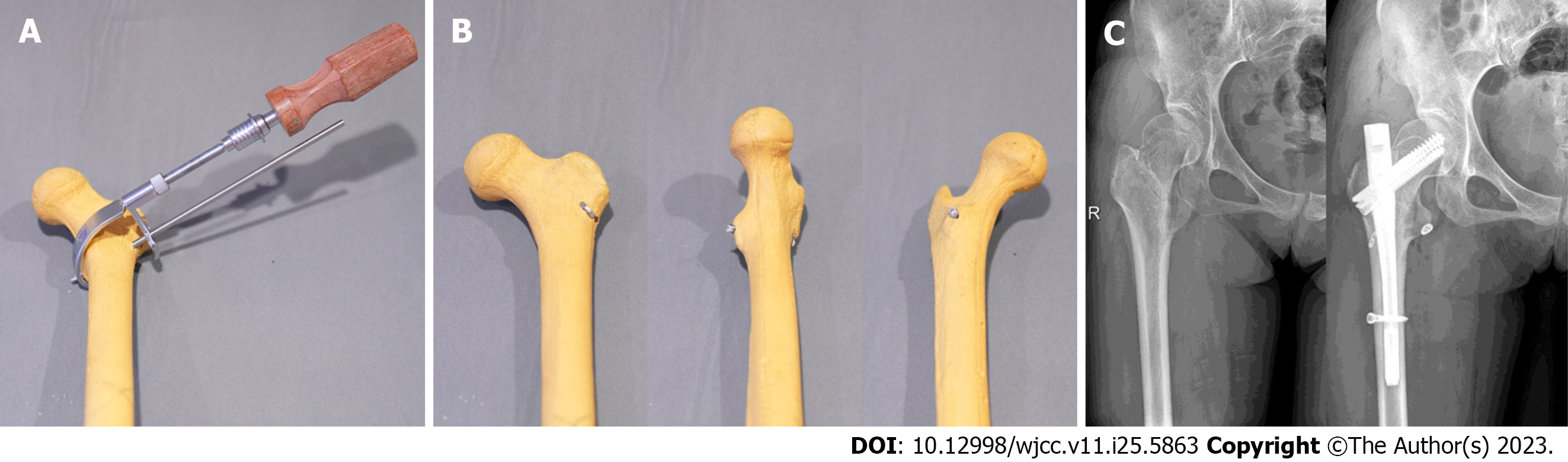
Surgical methods: Surgery was performed under general anesthesia. The patient was placed in a supine position. After being anesthetized, the patient was placed on an orthopedic traction bed. Manual traction reduction was performed, followed by fluoroscopy under a C-arm machine. After at least two qualified doctors confirmed that reduction was achieved, routine disinfection and draping were performed. An opening of about 4-5 cm was made on the proximal femur, and the lesser trochanteric reduction fixator was placed to reduce the lesser trochanter and maintain the fixed state (Figure 2). Proximal femoral nail-anti-rotation Asia II or integrated cephalomedullary nail placement was completed by routine opening at fixed points of the femur. The lesser trochanteric reduction fixator was introduced into the loop plate through a guiding hole. Subsequently, the button end of the loop plate was placed at the apex of the lesser trochanter and was tightened. Then, the newly developed lesser trochanteric reduction fixator was gradually loosened to observe whether there was any displacement of the lesser trochanter. After the position was stable, the loop plate was fixed to complete the surgery.
Postoperative treatment: After surgery, antibiotics were administered as per the requirements, and anticoagulants were administered as appropriate based on venous thromboembolism scores. Physiatrists guided the patients to conduct passive movement 6-8 h after surgery, and to actively move the knee joint and conduct quadriceps femoris function exercise 24 h after surgery. From four weeks after surgery, patients walked with a partial weight-bearing walking aid with the permission of the attending physician, who judged the timing to walk with full weight-bearing according to the postoperative image data.
IBM SPSS 26 was used for data analyses. An independent samples t-test was used for comparison of means between groups. A P value of < 0.05 was considered statistically significant.
The patients were divided into either an experimental group or a control group. The experimental group comprised five patients (two males and three females; age range, 51-70 years, with an average age of 60.2 years) who experienced intertrochanteric fractures and were treated using the lesser trochanteric reduction fixator, loop plates, and intra
The control group comprised 20 patients (4 males and 16 females; age range, 51-95 years, with an average age of 83.9 years) who experienced intertrochanteric fractures and were treated using simple intramedullary nails. These 20 cases included 13 cases with the left side affected and 7 cases with the right side affected.
Bone mineral density, age, fracture type, preoperative duration, operative duration, intraoperative blood loss, hospital stay, Harris hip score[2], and proximal incision length were compared between patients who were treated with and without the lesser trochanteric reduction fixator.
No significant difference was noted in age, fracture type, bone mineral density, preoperative duration, operative duration, or hospital stay between the two groups (P > 0.05). The postoperative Harris hip score in patients who were treated with the lesser trochanteric reduction fixator was significantly higher than that in patients who were treated without the lesser trochanteric reduction fixator (P < 0.05), which suggested that the lesser trochanteric reduction fixator had a positive impact on rehabilitation of the hip joint after surgery and could significantly enhance the quality of life of patients. In addition, the proximal incision in patients who were treated with the lesser trochanteric reduction fixator was larger than that in patients who were treated without the lesser trochanteric reduction fixator (P < 0.05). However, no significant difference was noted in the intraoperative blood loss between the two groups (P > 0.05) (Table 1).
| Simple intramedullary nails | Lesser trochanteric reduction fixators | P value | |
| Sex | |||
| Male | 4 | 3 | |
| Female | 16 | 2 | |
| Age (yr) | 83.95 ± 9.539 | 60.2 ± 7.463 | 0.066 |
| Fracture location | |||
| Left | 13 | 3 | |
| Right | 7 | 2 | |
| Bone mineral density | -1.635 ± 1.214 | -1.6 ± 1.474 | 0.956 |
| Preoperative duration (d) | 3.6 ± 2.414 | 2.6 ± 0.894 | 0.378 |
| Operation method | |||
| interTAN | 6 | 5 | |
| PFNA | 14 | 0 | |
| Operative duration (min) | 43.95 ± 17.251 | 69.4 ± 37.031 | 0.202 |
| Intraoperative blood loss (mL) | 81.5 ± 81.517 | 160 ± 54.772 | 0.055 |
| Hospital stay (d) | 12.85 ± 7.050 | 11.2 ± 3.768 | 0.622 |
| Harris hip score | 86.865 ± 5.653 | 91.94 ± 2.639 | 0.011 |
| Proximal incision length (cm) | 4.925 ± 0.293 | 6 ± 0.3536 | 0.000 |
From the perspective of mechanics, the biomechanical structure of the proximal femur is similar to that of a truss, and the calcar femorale receives support from the bony trabeculae in the posterior medial cortex of the upper femur, which is mainly the trochanter. The calcar femorale, the upper part of the femur, and three bundles of bony trabeculae form a reasonable weight-bearing system. From the biomechanical perspective, this system is the most important part to resist buckling and varus stress.
A defect in the lesser trochanter significantly compromises the biomechanical properties of the upper part of the femur. Biomechanical experiments have shown that defects in the lesser trochanter and extensive defects in the femur could induce obvious stress concentration in the upper part of the femur, increase the load strain and load displacement of the femoral head, reduce the stiffness of the femur, and impair the torsional strength and stiffness, which could decrease the mechanical performance of the femur significantly to resist external load and torsion. Severe torsional instability and failure of anti-deformation ability may cause hip instability. Defects in the lesser trochanter and extensive defects in the femur could induce femoral stress concentration. The strength could increase by 31% and 37%, respectively; femoral stiffness could decrease by 29% and 51%, respectively; and torsional strength of the femur could decrease by 33% and 54%, respectively. After fixing the lesser trochanter, stress concentration could decrease by 25% and 28%, respectively; stiffness could increase by 20% and 31%, respectively; and torsional strength could increase by 23% and 29%, respectively. Thus, significant restoration of the mechanical properties could be achieved.
Chen et al[3] conducted a mechanical analysis and test of type III fractures. The results showed that the average maximum load on the upper part of the femur was increased by 57% after anatomical reduction and fixation of a larger posterior medial bone block; however, the increase in the average maximum load on the upper part of the femur was 17% after anatomical reduction and fixation of a smaller posterior medial bone block. Therefore, reduction and fixation of the lesser trochanter is the key to mechanical stability of fractures. Domingo et al[4] simulated the femoral head under vertical compression by performing relevant experimental analysis. Besides, they measured the change in the force on the medial side of the lesser trochanter. Results showed that tensile stress on the medial side of the femoral head was obviously increased, and it reached 60% after the lesser trochanter was obviously displaced or defective. Therefore, they stated that displacement of the lesser trochanter could have a significant impact on surgical efficacy. Liu et al[5] suggested that the lesser trochanter is located under the calcar femorale, which is the medial cortex extending downwards from the femoral neck to the lesser trochanter. Its main function comprised ensuring that the local composition could bear a higher pressure and could transmit the force evenly to the medial femur. If the fracture affected the lesser trochanter or calcar femorale, displacement of local fracture blocks could occur, which may cause disruption of the normal physiological structure of the medial side, thus inducing coxa vara after surgery. Park et al[6] believed that if there was a defect in the lesser trochanter, the contralateral tension could significantly increase. In case of type II intertrochanteric fractures with lesser trochanteric defects, the contralateral tension could increase by 60%, and in case of type IV intertrochanteric fractures with lesser trochanteric defects, the contralateral tension could increase by 370%. Therefore, there may be an increase in the risk of fracture displacement, internal fixation loosening, rupture, femoral head cutting, and coxa vara as a result of only using internal fixation materials to maintain the weight load.
Reduction of the lesser trochanter is one of the most important key factors affecting fracture healing. Currently, many scholars believe that performing reduction of the lesser trochanter and restoring its anatomical function and shape are an optimal option.
Reduction of the lesser trochanter and reconstruction of calcar femorale are important for the treatment of intertrochanteric fractures. If reduction of the lesser trochanter is achieved by extensive soft tissue stripping, there will be disruption of the local blood supply to a certain extent, which would increase the fracture healing time. Although damage to the local blood supply will be reduced if the intertrochanteric fracture is fixed with a steel wire, the steel wire will affect the growth of the callus and the stability will not be favorable[7-8]. If the intertrochanteric fracture is fixed with the newly developed lesser trochanteric reduction fixator combined with loop plates, damage to the blood supply will be avoided and reliable fixation will also be achieved, which will not hamper the growth of the callus and can provide certain biological tension for elastic fixation.
There are some advantages of the newly developed lesser trochanteric reduction fixator: (1) After reliable reduction and fixation, the fixator can be introduced into the loop plate through customized holes, and the loop plate can pass through the muscle space of the lesser trochanter, which can achieve reduction and fixation of the lesser trochanter; (2) This fixator can improve the quality of reduction of the lesser trochanter, and the loop plate can achieve elastic fixation; and (3) The risk of nail breakage caused by nail fixation is minimized.
We fully realize the significance of trochanteric reduction and fixation, namely, reconstruction of structures under pressure, in the treatment of intertrochanteric fractures. As long as the general condition of patients is favorable and they are willing to undergo surgery, fixation should be carried out at the main fracture end and the lesser trochanter should be reduced and fixed at the same time. Some foreign scholars have proposed another method for performing nail fixation through a medial incision. However, as a medial incision causes greater trauma, we advocate that the lateral intra
We invented a new device for better treatment of femoral intertrochanteric fractures. During the treatment of intertrochanteric fractures, we fully realize the significance of trochanteric reduction and fixation, namely, reconstruction of structures under pressure.
As long as the general condition of patients is suitable and they are willing to undergo surgery, fixation should be carried out at the main fracture end and the lesser trochanter should be reduced and fixed at the same time. Some foreign scholars have proposed another method for performing nail fixation through a medial incision. However, as a medial incision causes larger trauma, we advocate that the lateral intramedullary nail incision shall be appropriately lengthened and the soft tissue shall be properly stripped from the anterior and posterior aspects of the greater trochanter, followed by placement of the newly developed lesser trochanteric reduction fixator.
We aimed to focus on how to avoid displacement of the lesser trochanter in unstable intertrochanteric fractures.
IBM SPSS 26 was used for data analyses. An independent samples t-test was used for comparison of means between groups. A P value of < 0.05 was considered statistically significant.
The postoperative Harris hip score in patients who were treated with the lesser trochanteric reduction fixator was significantly higher than that in patients who were treated without the lesser trochanteric reduction fixator (P < 0.05), which indicated that the lesser trochanteric reduction fixator had a positive impact on rehabilitation of the hip joint after surgery and could significantly improve the quality of life of patients. In addition, the proximal incision in patients who were treated with the lesser trochanteric reduction fixator was larger than that in patients who were treated without the lesser trochanteric reduction fixator (P < 0.05).
We fully realize the significance of trochanteric reduction and fixation, namely, reconstruction of structures under pressure, in the treatment of intertrochanteric fractures. As long as the general condition of patients is favorable and they are willing to undergo surgery, fixation should be carried out at the main fracture end and the lesser trochanter should be reduced and fixed at the same time. Some foreign scholars have proposed another method for performing nail fixation through a medial incision. However, as a medial incision causes greater trauma, we advocate that the lateral intra
This newly developed lesser trochanteric reduction fixator has some advantages: (1) After reliable reduction and fixation, this fixator can be introduced into the loop plate through the customized holes, and the loop plate can pass through the muscle space of the lesser trochanter, which can achieve reduction and fixation of the lesser trochanter; and (2) This fixator can improve the quality of reduction of the lesser trochanter, and the loop plate can achieve elastic fixation. There is no risk of nail breakage caused by nail fixation.
We thank Medjaden Inc. for scientific editing of this manuscript.
| 1. | Evans EM. The treatment of trochanteric fractures of the femur. J Bone Joint Surg Br. 1949;31B:190-203. [PubMed] |
| 2. | Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737-755. [PubMed] |
| 3. | Chen WH, Guo WX, Gao SH, Wei QS, Li ZQ, He W. Arthroplasty vs proximal femoral nails for unstable intertrochanteric femoral fractures in elderly patients: A systematic review and meta-analysis. World J Clin Cases. 2021;9:9878-9888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Domingo LJ, Cecilia D, Herrera A, Resines C. Trochanteric fractures treated with a proximal femoral nail. Int Orthop. 2001;25:298-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Liu X, Liu Y, Pan S, Cao H, Yu D. Does integrity of the lesser trochanter influence the surgical outcome of intertrochanteric fracture in elderly patients? BMC Musculoskelet Disord. 2015;16:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Park SY, Yang KH, Yoo JH, Yoon HK, Park HW. The treatment of reverse obliquity intertrochanteric fractures with the intramedullary hip nail. J Trauma. 2008;65:852-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Kim GM, Nam KW, Seo KB, Lim C, Kim J, Park YG. Wiring technique for lesser trochanter fixation in proximal IM nailing of unstable intertrochanteric fractures: A modified candy-package wiring technique. Injury. 2017;48:406-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Cho SH, Lee SH, Cho HL, Ku JH, Choi JH, Lee AJ. Additional fixations for sliding hip screws in treating unstable pertrochanteric femoral fractures (AO Type 31-A2): short-term clinical results. Clin Orthop Surg. 2011;3:107-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghimire R, Nepal S-Editor: Lin C L-Editor: Wang TQ P-Editor: Zhang YL