Published online Aug 26, 2023. doi: 10.12998/wjcc.v11.i24.5736
Peer-review started: April 8, 2023
First decision: May 12, 2023
Revised: June 19, 2023
Accepted: July 21, 2023
Article in press: July 21, 2023
Published online: August 26, 2023
Processing time: 139 Days and 1.6 Hours
Walled-off necrosis (WON) is a late complication of acute pancreatitis possibly with a fatal outcome. Even for WON spreading to the retroperitoneal space, percutaneous endoscopic necrosectomy (PEN) can be an alternate approach to surgical necrosectomy, particularly for the older individuals or patients with poor condition because of WON.
An 88-year-old man was admitted to our hospital with a jaundice. Endoscopic retrograde cholangiopancreatography (ERCP) was performed to improve jaun
PEN for WON occurring in the retroperitoneal space was safe and effective for very old individuals.
Core Tip: Percutaneous endoscopic necrosectomy (PEN) is an approach for the walled-off necrosis (WON) developing in the retroperitoneal space distant from the stomach or duodenum. Surgical necrosectomy is at high risk for older and frail patients, and less invasive drainage methods are ideal. We performed PEN for elderly with WON and were able to complete the treatment safely without complications.
- Citation: Sato K, Shibukawa G, Ueda K, Nakajima Y, Togashi K, Ohira H. Percutaneous endoscopic necrosectomy for walled-off necrosis in the retroperitoneal space of the elderly: A case report. World J Clin Cases 2023; 11(24): 5736-5741
- URL: https://www.wjgnet.com/2307-8960/full/v11/i24/5736.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i24.5736
Walled-off necrosis (WON) is a late complication of acute pancreatitis. The Atlanta Classification in 2012 defined WON as a necrotic reservoir > 4 wk after the onset of necrotizing pancreatitis[1]. Approximately 15% of severe acute pancreatitis patients are complicated by WON[2]. Moreover, 40% of patients with WON are complicated by organ failure, associated with longer hospital stays and high mortality rate[2].
Recently, endoscopic transluminal drainage and necrosectomy for WON have been widely accepted because of its clinical success rate of 80%-94%, an adverse event rate of 8%-25%, and a mortality rate of < 10%[3]. However, transluminal drainage is technically difficult when WON is located away from the stomach and duodenum, such as in the retroperitoneal space or paracolic gutters.
Percutaneous endoscopic necrosectomy (PEN) is one of the drainage methods for such cases. Herein, we report a very old patient with the WON widely spreading from the right retroperitoneal cavity to the pelvis, and the PEN was effective as a minimally invasive treatment method.
The patient mainly complained of jaundice.
An 88-year-old man was admitted to our hospital with jaundice. Computed tomography (CT) revealed stenosis in the lower bile duct and dilation of a common bile duct. Endoscopic retrograde cholangiopancreatography (ERCP) was performed to reduce the jaundice. However, abdominal pain manifested on the next day and post-ERCP pancreatitis developed.
The patient had a history of hypertension.
The patient’s personal and family history was unremarkable.
Abdominal pain was present at the onset of post-ERCP pancreatitis. It gradually subsided. However, fever and malaise persisted.
Blood tests showed persistently high C-reactive protein level.
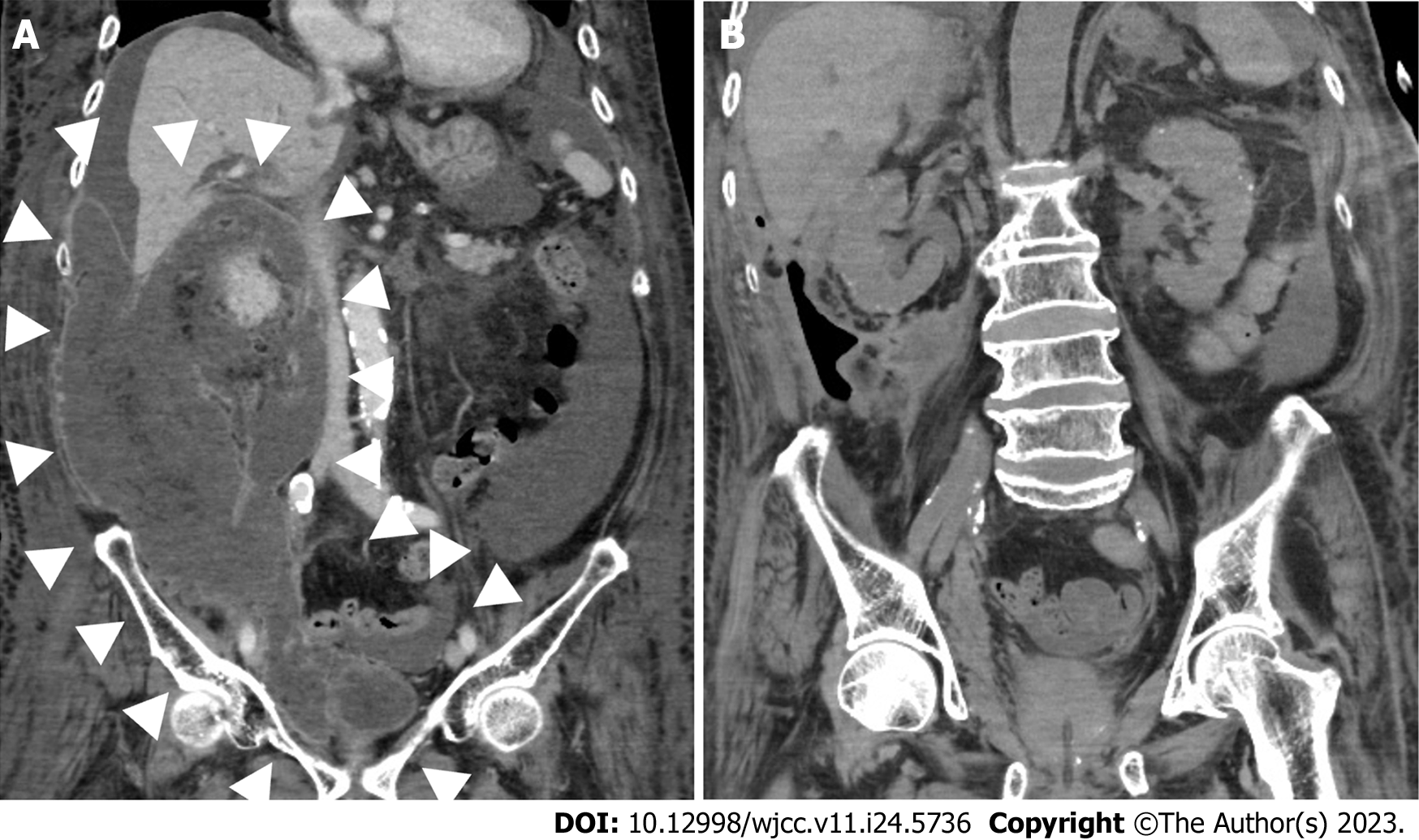
A CT performed 4 wk after ERCP revealed WON in the right perinephric space spreading to a bladder rectal fossa (Figure 1A). The major axis of WON was about 31 cm.
The patient was diagnosed with WON.
An 8-Fr percutaneous drainage tube was placed toward the WON under CT guidance. However, drainage tube placement alone did not improve the inflammatory response, requiring a necrosectomy. However, surgical necrosectomy under general anesthesia was a high risk of perioperative complications because of malnutrition and large pleural effusions. So, he was proposed for PEN of the WON. Eight weeks after ERCP, the percutaneous drainage tube was removed and the fistula was extended to 18 mm with a dilation balloon catheter (CRE PRO GI Wireguided Balloon Dilation Catheter; Boston Scientific, Co., Ltd., MA, United States). A 20 mm diameter gastroduodenal partially covered metallic stent (Niti-S; Taewoong Medical Co., Ltd., Gimpo, South Korea) was placed from the percutaneous drainage route. Immediately after the placement of metallic stent, the lumen was poorly dilated and expanded gradually. Moreover, because the stent was partially covered, there was a possibility that the position of the stent would be displaced if the endoscope was inserted immediately after the placement of the stent. For these reasons, PEN was performed 3 days after stenting. The endoscope was GIF-XZ1200 (Olympus, Co., Ltd., Tokyo, Japan) and snare forceps (SnareMaster Plus 25mm; Olympus) were used to bluntly remove the necrotic materials. A total of 10 necrosectomies were performed over 2 mo. Most of the necrotic material could be removed in about 3 wk; however, its removal from in the ventral side of the kidney and pelvic cavity was time-consuming.
CT revealed a small amount of residual WON in a ventral aorta and near a bladder; however, the necrotic tissues in the right retroperitoneal space were apparently reduced (Figure 1B). Occasional low-grade fever appeared, but improved conservatively. The stent was removed 12 wk after placement. Granulation tissue grew inside the stent and manual removal was difficult. It was bluntly removed under general anesthesia and cauterization of the dissected surface was performed. The fistula spontaneously shrunk after stent removal. Although rehabilitation was continued, he was transferred to another hospital 6 mo after admission because he was old and had limited ability to improve muscle strength.
A surgical step-up approach is proposed as a percutaneous drainage method. In this method, a percutaneous drainage tube is placed first, and if there is no improvement, a surgical necrosectomy is performed[4]. In a comparative study with endoscopic step-up approach that consisted of endoscopic ultrasound-guided transluminal drainage followed by endoscopic necrosectomy, if necessary, rates of major complications and death did not differ between surgical and endoscopic step-up approach[4]. However, pancreatic cutaneous fistula formation occurred more frequently in the surgical step-up approach group. Moreover, surgical necrosectomy must be performed under general anesthesia, making it difficult to perform in patients with poor general condition or elderly patients with many complications. However, PEN can be performed without general anesthesia.
PEN has been reported in a small number of cases, however, Jagielski summarized the outcomes of previous reports[5]. In this report, percutaneous esophageal self-expandable metallic stent (SEMS) was placed in 52 patients with WON, with a procedural success rate of 100% and clinical success rate of 80.8% (Table 1)[6-19]. Complications were observed in 34.6% of the patients, including complications unrelated to the procedure such as organ failure associated with acute pancreatitis and recurrence of fluid collection. No procedure-related deaths occurred. Hemorrhage requiring radiological or surgical intervention occurred in 10 patients, however they were unrelated to percutaneous SEMS placement and necrosectomy procedures. Cutaneous fistulas developed in two patients after SEMS removal, and one of which required surgery. A previous study reported that cutaneous fistula never occurred when percutaneous and transluminal endoscopic necrosectomy were performed at the same time[20].
| Ref. | Patients, n | Mean age, yr | Oldest age, yr | Size of collection, mean, cm | Previous endoscopic/surgical treatment attempt (n) | Mean number of PEN sessions performed | Devices used for necrosectomy | Length of time stent in place, mean, days | Clinical success, n (%) |
| Bakken et al[6], 2011 | 1 | 75 | 75 | NA | PCD | NA | Snares, rat toothed forceps | NA | 1/1 (100) |
| Bakken et al[7], 2011 | 2 | 70 | 74 | NA | NA | 2.5 | NA | 25 | 2/2 (100) |
| Patil et al[8], 2021 | 1 | 59 | 59 | 14 | PCD | 4 | Snares, stone retrieval baskets | 28 | 1/1 (100) |
| Binda et al[9], 2021 | 1 | 61 | 61 | NA | PCD, ETN | 4 | Snares | 14 | 1/1 (100) |
| Ke et al[10], 2019 | 23 | 43 | 54 | NA | PCD | 2 | Snares, grasping forceps | 7 | 16/23 (69.57) |
| Thorsen et al[11], 2018 | 5 | 44 | 72 | 33.4 | PCD (3), ETN (2) | 5.75 | Snares, tripod forceps, stone retrieval baskets | 37.5 | 4/5 (80) |
| Tringali et al[12], 2018 | 3 | 45 | 64 | 15 | PCD (3) | 3 | Dormia baskets | 12.7 | 2/3 (66.67) |
| Saumoy et al[13], 2017 | 9 | 62 | 81 | 11.2 | PCD (9) | 3 | Snares, stone retrieval baskets | 14.7 | 8/9 (88.89) |
| D'Souza et al[14], 2017 | 1 | 32 | 32 | NA | PCD | 1 | Snares | NA | 1/1 (100) |
| Sato et al[15], 2016 | 1 | 13 | 13 | NA | PCD | 3 | NA | 17 | 1/1 (100) |
| Kedia et al[16], 2015 | 1 | 56 | 56 | 17 | PCD, ETN | 2 | NA | NA | 1/1 (100) |
| Cerecedo-Rodriguez et al[17], 2014 | 1 | 46 | 46 | NA | PCD, surgical lavages | 7 | NA | NA | 1/1 (100) |
| Navarrete et al[18], 2011 | 1 | 37 | 37 | NA | PCD | 4 | NA | 12 | 1/1 (100) |
| Laopeamthong et al[19], 2019 | 1 | 48 | 48 | NA | PCD | 4 | Snares | NA | 1/1 (100) |
| Our case | 1 | 88 | 88 | 31 | PCD | 10 | Snares, grasping forceps | 84 | 1/1 (100) |
Most of the cases in this report are under the age of 60, with only a few elderly patients discussed. In this case, we were able to perform PEN safely, without complications, even in an elderly patient who was approximately 90-year-old. Other reports have indicated that age dose not play a role in the success rate of endoscopic transluminal drainage and necrosectomy[21,22], which might be the same for PEN.
In a report by Jagielski et al[5], the number of PEN procedures was less and the clinical success rate was high. In our case, although we were able to remove most of the necrotic material, the hospital stay of the patient was prolonged, and his activities of daily living were negatively affected. Moreover, fever and elevated inflammatory response seen in blood tests persisted, and the treatment period was prolonged because the WON in narrow spaces like the ventral side of the kidney and the pelvic cavity was difficult to remove. CT showed a large amount of necrotic material in the WON, making it difficult to treat with only an indwelling drainage tube. In such cases, considering the start of PEN sooner could potentially complete the treatment early. Current international guidelines recommend postponing endoscopic interventions for pancreatic necrosis until at least 4 wk after the onset of pancreatitis, helping to encapsulate and define necrosis. However, there are also reports that the number of complications dose not increase when transluminal endoscopic necrosectomy is performed early than 4 wk after pancreatitis onset[23,24]. In this case, it may have been better to perform drainage and necrosectomy early, as soon as encapsulation of the necrotic material was confirmed.
Snare forceps are often used for necrosectomy, and were mainly used in our case as well. Grasping forceps were used in narrow spaces during the procedure; however, the necrotic material containing pus and fat was soft and difficult to grasp. Multi-prong forceps were not used because they might damage to blood vessels and kidneys, which are not visible due to necrotic material. Snare forceps are considered to be the first choice because they make it easier to grasp necrotic material and are less likely to damage surrounding organs.
In transluminal endoscopic necrosectomy, removal of the lumen-apposing metal stents within 4 wk is recommended due to the risk of perforation and migration. In this case, the stent was removed 12 wk after placement, which required general anesthesia. However, there were no stent problems during placement or after removal.
In the present case, WON was found mainly in the retroperitoneal space, and PEN would be appropriate. Because of old age and malnutrition, invasive procedures were not possible. If the percutaneous drainage tube did not work well as in this patient, PEN might be attempted for the elderly. However, it takes time for the elderly to recover appropriately to perform daily living activities, so it is necessary to determine the appropriate timing of treatment.
We experienced a case of WON that extensively spread to the retroperitoneal space but was relieved by PEN. The procedure was safe and effective even in older patients with frailty.
| 1. | Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4932] [Cited by in RCA: 4719] [Article Influence: 363.0] [Reference Citation Analysis (48)] |
| 2. | da Costa DW, Boerma D, van Santvoort HC, Horvath KD, Werner J, Carter CR, Bollen TL, Gooszen HG, Besselink MG, Bakker OJ. Staged multidisciplinary step-up management for necrotizing pancreatitis. Br J Surg. 2014;101:e65-e79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 119] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 3. | Feng L, Guo J, Wang S, Liu X, Ge N, Wang G, Sun S. Endoscopic Transmural Drainage and Necrosectomy in Acute Necrotizing Pancreatitis: A Review. J Transl Int Med. 2021;9:168-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | van Brunschot S, van Grinsven J, van Santvoort HC, Bakker OJ, Besselink MG, Boermeester MA, Bollen TL, Bosscha K, Bouwense SA, Bruno MJ, Cappendijk VC, Consten EC, Dejong CH, van Eijck CH, Erkelens WG, van Goor H, van Grevenstein WMU, Haveman JW, Hofker SH, Jansen JM, Laméris JS, van Lienden KP, Meijssen MA, Mulder CJ, Nieuwenhuijs VB, Poley JW, Quispel R, de Ridder RJ, Römkens TE, Scheepers JJ, Schepers NJ, Schwartz MP, Seerden T, Spanier BWM, Straathof JWA, Strijker M, Timmer R, Venneman NG, Vleggaar FP, Voermans RP, Witteman BJ, Gooszen HG, Dijkgraaf MG, Fockens P; Dutch Pancreatitis Study Group. Endoscopic or surgical step-up approach for infected necrotising pancreatitis: a multicentre randomised trial. Lancet. 2018;391:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 588] [Cited by in RCA: 510] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 5. | Jagielski M, Chwarścianek A, Piątkowski J, Jackowski M. Percutaneous Endoscopic Necrosectomy-A Review of the Literature. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Bakken JC, Baron TH. Pancreatic necrosectomy via percutaneous selfexpandable metal stent placement. Gastrointest Endosc. 2011;73:AB103. [DOI] [Full Text] |
| 7. | Bakken JC, Baron TH. Use of partially covered and fully covered selfexpandable metal stents to establish percutaneous access for endoscopic necrosectomy. Endoscopy. 2011;43:A69. [DOI] [Full Text] |
| 8. | Patil G, Maydeo A, Dalal A, Iyer A, More R, Thakare S. Endoscopic Retroperitoneal Necrosectomy for Infected Pancreatic Necrosis Using a Self-Expandable Metal Stent. GE Port J Gastroenterol. 2021;28:425-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Binda C, Sbrancia M, La Marca M, Colussi D, Vizzuso A, Tomasoni M, Agnoletti V, Giampalma E, Ansaloni L, Fabbri C. EUS-guided drainage using lumen apposing metal stent and percutaneous endoscopic necrosectomy as dual approach for the management of complex walled-off necrosis: a case report and a review of the literature. World J Emerg Surg. 2021;16:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Ke L, Mao W, Zhou J, Ye B, Li G, Zhang J, Wang P, Tong Z, Windsor J, Li W. Stent-Assisted Percutaneous Endoscopic Necrosectomy for Infected Pancreatic Necrosis: Technical Report and a Pilot Study. World J Surg. 2019;43:1121-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Thorsen A, Borch AM, Novovic S, Schmidt PN, Gluud LL. Endoscopic Necrosectomy Through Percutaneous Self-Expanding Metal Stents May Be a Promising Additive in Treatment of Necrotizing Pancreatitis. Dig Dis Sci. 2018;63:2456-2465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Tringali A, Vadalà di Prampero SF, Bove V, Perri V, La Greca A, Pepe G, Cozza V, Costamagna G. Endoscopic necrosectomy of walled-off pancreatic necrosis by large-bore percutaneus metal stent: a new opportunity? Endosc Int Open. 2018;6:E274-E278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Saumoy M, Kumta NA, Tyberg A, Brown E, Lieberman MD, Eachempati SR, Winokur RS, Gaidhane M, Sharaiha RZ, Kahaleh M. Transcutaneous Endoscopic Necrosectomy for Walled-off Pancreatic Necrosis in the Paracolic Gutter. J Clin Gastroenterol. 2018;52:458-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | D'Souza LS, Korman A, Carr-Locke DL, Benias PC. Percutaneous endoscopic necrosectomy. Endoscopy. 2017;49:E242-E243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Sato S, Takahashi H, Sato M, Yokoyama M, Itoi T, Kawano Y, Kawashima H. A case of walled-off necrosis with systemic lupus erythematosus: Successful treatment with endoscopic necrosectomy. Semin Arthritis Rheum. 2016;46:e13-e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Kedia P, Parra V, Zerbo S, Sharaiha RZ, Kahaleh M. Cleaning the paracolic gutter: transcutaneous endoscopic necrosectomy through a fully covered metal esophageal stent. Gastrointest Endosc. 2015;81:1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Cerecedo-Rodriguez J, Hernández-Trejo A, Alanís-Monroy E, Barba-Mendoza JA, Benítez Tress-Faez Mdel P, Figueroa-Barojas P. Endoscopic percutaneous pancreatic necrosectomy. Gastrointest Endosc. 2014;80:165-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Navarrete C, Castillo C, Caracci M, Vargas P, Gobelet J, Robles I. Wide percutaneous access to pancreatic necrosis with self-expandable stent: new application (with video). Gastrointest Endosc. 2011;73:609-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Laopeamthong I, Tonozuka R, Kojima H, Mukai S, Tsuchiya T, Sofuni A, Itoi T. Percutaneous endoscopic necrosectomy using a fully covered self-expandable metal stent in severe necrotizing pancreatitis. Endoscopy. 2019;51:E22-E23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Ross AS, Irani S, Gan SI, Rocha F, Siegal J, Fotoohi M, Hauptmann E, Robinson D, Crane R, Kozarek R, Gluck M. Dual-modality drainage of infected and symptomatic walled-off pancreatic necrosis: long-term clinical outcomes. Gastrointest Endosc. 2014;79:929-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 21. | Bang JY, Wilcox CM, Trevino J, Ramesh J, Peter S, Hasan M, Hawes RH, Varadarajulu S. Factors impacting treatment outcomes in the endoscopic management of walled-off pancreatic necrosis. J Gastroenterol Hepatol. 2013;28:1725-1732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Kim YS, Cho JH, Cho DH, Park SW, Moon SH, Park JS, Lee YN, Lee SS. Long-term Outcomes of Direct Endoscopic Necrosectomy for Complicated or Symptomatic Walled-Off Necrosis: A Korean Multicenter Study. Gut Liver. 2021;15:930-939. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Trikudanathan G, Tawfik P, Amateau SK, Munigala S, Arain M, Attam R, Beilman G, Flanagan S, Freeman ML, Mallery S. Early (<4 Weeks) Versus Standard (≥ 4 Weeks) Endoscopically Centered Step-Up Interventions for Necrotizing Pancreatitis. Am J Gastroenterol. 2018;113:1550-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 125] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 24. | Oblizajek N, Takahashi N, Agayeva S, Bazerbachi F, Chandrasekhara V, Levy M, Storm A, Baron T, Chari S, Gleeson FC, Pearson R, Petersen BT, Vege SS, Lennon R, Topazian M, Abu Dayyeh BK. Outcomes of early endoscopic intervention for pancreatic necrotic collections: a matched case-control study. Gastrointest Endosc. 2020;91:1303-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D, D
Grade E (Poor): E
P-Reviewer: Angst E, United States; Jha AK, India; Tharavej C, Thailand S-Editor: Yan JP L-Editor: A P-Editor: Zhang XD