Published online Aug 16, 2023. doi: 10.12998/wjcc.v11.i23.5519
Peer-review started: April 8, 2023
First decision: July 4, 2023
Revised: July 19, 2023
Accepted: July 25, 2023
Article in press: July 25, 2023
Published online: August 16, 2023
Processing time: 129 Days and 23.6 Hours
Total hip arthroplasty (THA) is an effective treatment for advanced osteonecrosis of the femoral head, which can significantly relieve pain and improve patients' quality of life. Robotic-assisted THA enhances the accuracy and stability of THA surgery and achieves better clinical outcomes than manual THA.
We report the clinical outcomes of robotic-assisted THA and manual THA in the same patient with osteonecrosis of the femoral head. A 49-year-old male patient attended our hospital due to more than 3 years of pain in both hip joints. The left hip was treated with robotic-assisted THA. The patient underwent manual THA of the right hip 3 mo after robotic-assisted THA. We obtained postoperative radiograph parameters, Harris hip score and forgotten joint score of the patient 1 year after surgery.
Compared with manual THA, the patient’s left hip felt better 1 year after robotic-assisted THA. Robotic-assisted THA resulted in a better Harris hip score and forgotten joint score than manual THA in the same patient with osteonecrosis of the femoral head.
Core Tip: Osteonecrosis of the femoral head is a common disease. Total hip arthroplasty (THA) is an effective treatment for advanced osteonecrosis of the femoral head. Robotic-assisted THA has been shown to increase accuracy and precision during surgery. We report the clinical outcomes of robotic-assisted THA and manual THA in the same patient with osteonecrosis of the femoral head. Combined with the analysis of cases indexed in PubMed, robotic-assisted THA resulted in a better Harris hip score and forgotten joint score than manual THA, and the patient felt better 1 year after surgery.
- Citation: Hu TY, Lin DC, Zhou YJ, Zhang ZW, Yuan JJ. Clinical outcomes of robotic-assisted and manual total hip arthroplasty in the same patient: A case report. World J Clin Cases 2023; 11(23): 5519-5524
- URL: https://www.wjgnet.com/2307-8960/full/v11/i23/5519.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i23.5519
Osteonecrosis of the femoral head is a common and intractable disease in orthopedics. Total hip arthroplasty (THA) is an effective treatment in the late stage to improve hip function[1,2]. Precise and accurate biomechanical reconstruction during THA is essential for durable long-term survival of the implant. Implant malposition can easily lead to intraoperative fractures, failure of prosthesis fixation, limited hip joint movement, and prosthesis dislocation and loosening[3-6]. The MAKO robotic systems (e.g., RIO®, MAKO-Stryker, Stryker Orthopedics, Mahwah, NJ, United States) is a semi-active (haptic) robotic system and one of the most advanced orthopedic surgery robot, especially in THA. Compared with manual THA, robotic-assisted THA may lead to more accurate reconstruction of radiographic parameters, such as implant positioning, fit, center-of-rotation and leg-length discrepancy, and achieve better clinical and radiographic outcomes[7-11].
Many clinical studies have reported the excellent effect of robotic-assisted THA. However, there have been no reports on bilateral THA (manual THA on one side and robotic-assisted on the other side) in the same patient within a short period of time. We here present such a case to explore the differences in hip function between the two treatments in the same patient.
A 49-year-old male patient attended our hospital due to more than 3 years of pain in both hip joints.
The patient had persistent pain in both hip joints without inducement for more than 3 years. He had visited another hospital and was diagnosed with osteonecrosis of both femoral heads. Conservative treatments were prescribed without relief. Therefore, she visited our hospital for further treatment.
The patient was previously healthy.
No relevant disorders were identified.
The patient had a stable gait, and preoperative physical examination showed no limb length discrepancy. The patient reported a mild to moderate amount of stiffness and pain in both anterior hip regions. The patient's external rotation of bilateral hip joints was limited, and more pronounced on the left.
Routine blood tests revealed normal blood cell contents. Prothrombin, D-dimer and partial thromboplastin time were normal. Serum C-reactive protein was normal at 1.01 mg/dL (reference range < 5 mg/dL) and interleukin-6 was 1.65 pg/mL (reference range 0-7 pg/mL). Blood biochemistry as well as urinary and fecal analysis were normal.
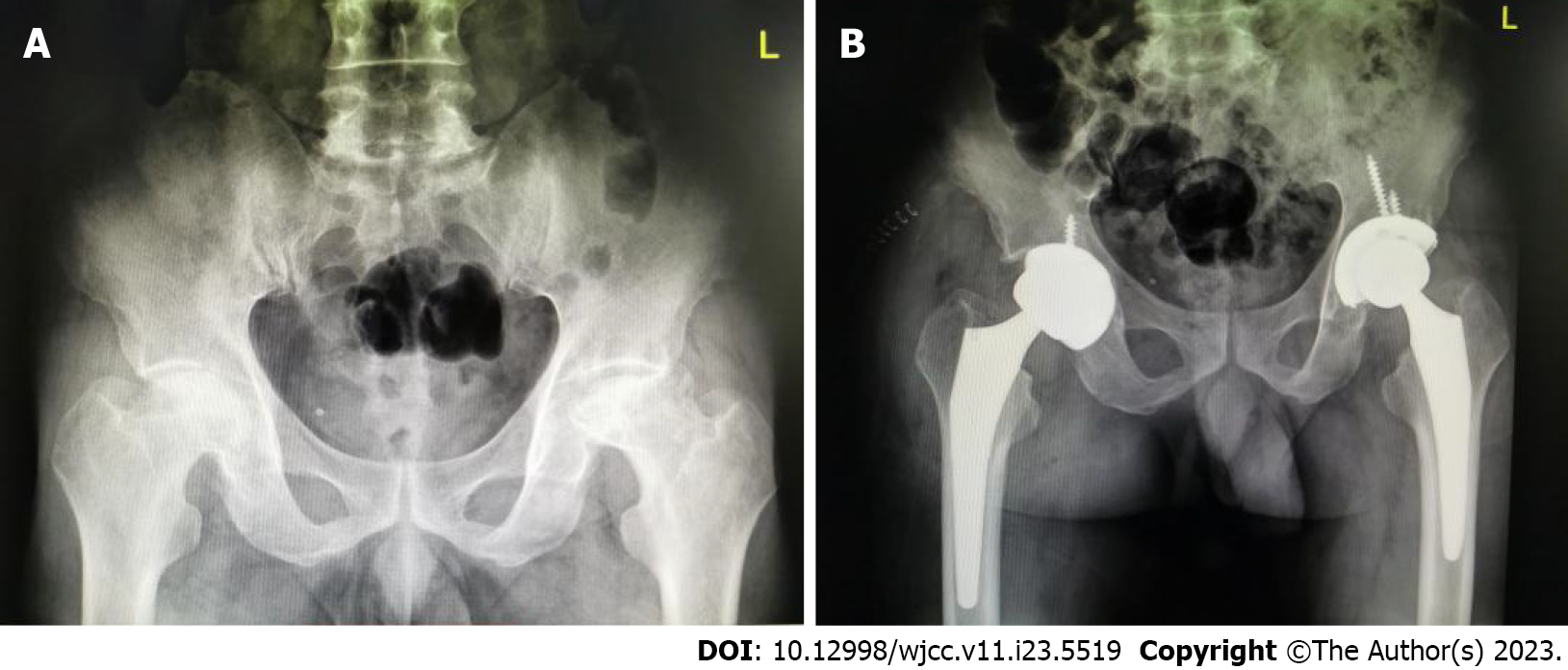
Plain radiographs (Figure 1A) revealed Association Research Circulation Osseous (ARCO) stage IV osteonecrosis of both femoral heads.
Combined with the patient’s medical history, the final diagnosis was ARCO stage IV osteonecrosis of both femoral heads.
The left hip was treated with robotic-assisted THA, the surgical robot model was RIO® Robotic Arm Interactive Orthopedic System (Stryker, United States), and the operating system version was THA 3.1. The Stryker prosthesis, Trident acetabular component, X3 polyethylene liner, and Accolade II femoral stem were used. Three-dimensional (3D) computed tomography (CT) scans of the hip joint were performed preoperatively. The scan parameters were in accordance with the requirements of the MAKO system, and the CT scan results were uploaded to the Stryker Robotic Surgery Center for preoperative planning. The virtual prosthesis was implanted to produce the surgical plan (Figure 2). In the preoperative plan, the acetabular cup inclination was 42° and anteversion was 20°. The depth of acetabular reaming was the same as that for conventional manual THA, grinding inward without penetrating the inner wall, removing all acetabular cartilage, grinding the acetabulum into a hemispherical shape, and preserving the subchondral bone as much as possible. A small uniform acetabulum was seen during the operation. Oozing blood showed the "blush sign". Specific bony landmarks were calibrated. The first step was to paste electrocardiograph (ECG) electrodes on the lower end of the patella when the knee was flexed. The second step was to implant 3 bone screws on the anterior superior iliac spine on the operative side to fix and install the acetabular reference frame. In the greater trochanter of the femur, the probe was used to locate the ECG electrode and the greater trochanter screw to complete the positioning of the bony landmarks. The marker screw was implanted above the acetabulum following exposure of the acetabulum and the probe was used to locate the marker. Acetabular registration was then performed, including 3 acetabular direction determination points, 32 registration points and 8 confirmation points, and a 3D model was established according to the preoperative CT scan corresponding to the real anatomical structure of the hip joint. Acetabular grinding and installation of the acetabular components were carried out according to the plan under the guidance and restraint of the robotic arm. During the femoral side operation, the proximal femur was exposed, followed by opening, reaming and trial. During try-out, the probes were used to locate marker screws and electrodes on the proximal and distal femurs, and the MAKO system fed back data on leg length and offset. The full range of motion demonstrated stability, especially when fully extended and externally rotated 40°, flexed 90° with at least 45° internal rotation, and adducted and axially compressed with 40° of flexion. The femoral components were installed after the leg length, offset and stability tests were satisfied.
Due to hospitalization expenses, the patient underwent manual THA of the right hip 3 mo after robotic-assisted THA of the left hip.
On the first day after surgery, the patient was able to walk a few steps with crutches. Following discharge from hospital, he used crutches for 2 mo, and then changed to a single crutch or canes for 1 mo. The patient’s Harris score (Table 1) and forgotten joint score (Table 2) were followed up 1 year after surgery, and the postoperative X-ray view of the pelvis is shown in Figure 1B.
| Robotic-assisted THA on the left | Manual THA on the right | |
| Preoperative | 46 | 55 |
| Postoperative | 89 | 82 |
| Robotic-assisted THA on the left | Manual THA on the right | |
| 1 yr after surgery | 76 | 82 |
A large number of literature has reported the accuracy advantages of robotic-assisted surgery compared to manual operations[12-15], which can achieve more accurate prosthesis anteversion angle and better limb length. However, robot surgery also has limitations. According to a report[16], the operating time of robotic-assisted surgery is significantly longer than that of manual surgery, which is related to the additional time required for parameter setting of the robotic-assisted surgical system. Another study[17] reported that the learning curve of the same doctor for this operation was 14 cases. After 14 cases, the operation performance of the doctor tended to be stable.
People tend to pay more attention to the feelings of the majority, but in this era, the feelings of each individual deserve more attention. A large number of clinical studies have proved that robotic-assisted THA surgery can achieve a better prognosis. However, few studies have reported the short-term clinical efficacy of robotic-assisted THA and traditional manual THA in the same patient. In the present case, at the request of the patient, manual THA surgery (to reduce the cost of treatment) was performed on the right side 3 mo after the robotic-assisted surgery, and the patient was followed up in terms of the postoperative radiograph parameters, Harris hip score and forgotten joint score after surgery. Postoperative X-rays of the hip joint showed that an ideal acetabular inclination was obtained by preoperative planning of robotic-assisted THA. Previous studies have shown significant advantages of robotic-assisted THA in restoring leg length and offset. The study by Tsai et al[12] has demonstrated that robotic-assisted THA can better restore the physiological structure of the hip joint, making the leg length difference smaller and the offset closer to the physiological level. The study by Redmond et al[13] showed that robotic-assisted THA could obtain an average length difference of less than 0.5 cm, and the largest difference was less than 1 cm. In the present study, the difference in the patient’s limb length discrepancy was less than 0.5 cm, which was basically the same as that reported in the previous study. This means that manual THA can also achieve a satisfactory limb length difference. In terms of clinical outcomes, in the study by Perets et al[9], robotic-assisted THA was superior in terms of functional recovery. The findings in the present case were consistent with previously reported results, the patient's Harris hip scores and forgotten joint scores were greater compared with manual THA, and no complications were observed in both hips.
There are few reports on the clinical effect of bilateral THA (manual THA and robotic-assisted THA) in the same patient. In our case, robotic-assisted THA resulted in a better Harris hip score and forgotten joint score than manual THA. The future surgery should be more precise and personalized, and with the help of robotic-assistance may achieve goals that cannot be reached by manual surgery. This case report provides strong clinical evidence for robotic-assisted THA.
| 1. | Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1477] [Cited by in RCA: 1912] [Article Influence: 100.6] [Reference Citation Analysis (0)] |
| 2. | Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1270] [Cited by in RCA: 1367] [Article Influence: 62.1] [Reference Citation Analysis (0)] |
| 3. | Zengerink I, Reijman M, Mathijssen NM, Eikens-Jansen MP, Bos PK. Hip Arthroplasty Malpractice Claims in the Netherlands: Closed Claim Study 2000-2012. J Arthroplasty. 2016;31:1890-1893.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Patterson DC, Grelsamer RP, Bronson MJ, Moucha CS. Lawsuits After Primary and Revision Total Hip Arthroplasties: A Malpractice Claims Analysis. J Arthroplasty. 2017;32:2958-2962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Ellapparadja P, Mahajan V, Atiya S, Sankar B, Deep K. Leg length discrepancy in computer navigated total hip arthroplasty - how accurate are we? Hip Int. 2016;26:438-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | GE L, JL L, CL C, JR Z. Dislocations after total hip replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217-220. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1972] [Cited by in RCA: 2099] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 7. | Kanawade V, Dorr LD, Banks SA, Zhang Z, Wan Z. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty. 2015;30:392-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Nodzo SR, Chang CC, Carroll KM, Barlow BT, Banks SA, Padgett DE, Mayman DJ, Jerabek SA. Intraoperative placement of total hip arthroplasty components with robotic-arm assisted technology correlates with postoperative implant position: a CT-based study. Bone Joint J. 2018;100-B:1303-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 81] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 9. | Perets I, Walsh JP, Close MR, Mu BH, Yuen LC, Domb BG. Robot-assisted total hip arthroplasty: Clinical outcomes and complication rate. Int J Med Robot. 2018;14:e1912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Kong X, Yang M, Jerabek S, Zhang G, Chen J, Chai W. A retrospective study comparing a single surgeon's experience on manual versus robot-assisted total hip arthroplasty after the learning curve of the latter procedure - A cohort study. Int J Surg. 2020;77:174-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 11. | Kong X, Yang M, Li X, Ni M, Zhang G, Chen J, Chai W. Impact of surgeon handedness in manual and robot-assisted total hip arthroplasty. J Orthop Surg Res. 2020;15:159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Tsai TY, Dimitriou D, Li JS, Kwon YM. Does haptic robot-assisted total hip arthroplasty better restore native acetabular and femoral anatomy? Int J Med Robot. 2016;12:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Redmond JM, Gupta A, Hammarstedt JE, Petrakos AE, Finch NA, Domb BG. The learning curve associated with robotic-assisted total hip arthroplasty. J Arthroplasty. 2015;30:50-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 14. | Domb BG, El Bitar YF, Sadik AY, Stake CE, Botser IB. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. 2014;472:329-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 242] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 15. | Chen X, Xiong J, Wang P, Zhu S, Qi W, Peng H, Yu L, Qian W. Robotic-assisted compared with conventional total hip arthroplasty: systematic review and meta-analysis. Postgrad Med J. 2018;94:335-341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 16. | Zhang Z, Kong X, Yang M, Guo R, Song P, Wu D, Chen J, Chai W. Short⁃term outcome of robot⁃assisted total hip arthroplasty. Orthopaedics. 2020;11:269-273. [DOI] [Full Text] |
| 17. | Kong X, Yang M, Jerabek S, Zhang G, Chen J, Chai W. A retrospective study comparing a single surgeon's experience on manual versus robot-assisted total hip arthroplasty after the learning curve of the latter procedure - A cohort study. Int J Surg. 2020;77:174-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Primadhi RA, Indonesia S-Editor: Liu JH L-Editor: A P-Editor: Yuan YY