Published online Aug 6, 2023. doi: 10.12998/wjcc.v11.i22.5382
Peer-review started: May 4, 2023
First decision: May 25, 2023
Revised: June 1, 2023
Accepted: July 6, 2023
Article in press: July 6, 2023
Published online: August 6, 2023
Processing time: 90 Days and 19.5 Hours
Sialolithiasis is one of the most common salivary gland disorders, most commonly affecting the submandibular gland. Submandibular sialolithiasis can be treated using non-invasive conservative measures and invasive treatments. Treatment selection was based on the ductal system anatomy and the size and location of the stones. This study aimed to review the updates on sialolithiasis treatment and compare the different management strategies of the variables.
This report presents a case of a long-term, rare, and giant sialolithiasis within the submandibular gland parenchyma for 30 years in an older adult. Our patient presented with painless right submandibular swelling. Computed tomography revealed a calcified mass measuring 35 mm × 20 mm within the right subman
Tailored management is important for preserving gland function, maintaining low risk, and reducing patient discomfort.
Core Tip: Giant sialoliths are uncommon, and their long duration is rarely documented. This report presents a case of a long-term, rare, and giant sialolithiasis within the submandibular gland parenchyma for 30 years in an older adult. We reviewed 44 cases of giant sialoliths that were reported between 1981 and 2022. Based on the comparative table, our case is the second largest with the longest duration. This case highlights the importance of proper diagnosis and treatment.
- Citation: Mao JS, Lee YC, Chi JCY, Yi WL, Tsou YA, Lin CD, Tai CJ, Shih LC. Long-term rare giant sialolithiasis for 30 years: A case report and review of literature. World J Clin Cases 2023; 11(22): 5382-5390
- URL: https://www.wjgnet.com/2307-8960/full/v11/i22/5382.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i22.5382
Sialoliths are calcified salivary stones that can form within the secretory system of the salivary glands. Although various hypotheses have been proposed, the exact etiology of these sialoliths remains unclear. Most patients with sialolithiasis present with symptoms such as local pain, focal swelling, trismus, xerostomia, and lumps in the throat. Inflammation with oozing pus may be noted in some cases due to secondary infection.
The submandibular gland is the most commonly affected site for sialoliths, accounting for approximately 80%-90% of cases[1]. The rate of giant sialolith formation within the submandibular gland is high, and several contributing factors have been proposed, including a longer Wharton’s duct, larger duct caliber, and tortuous course of the Wharton’s duct accompanied by a slower salivary flow rate within the submandibular gland compared with that in other salivary ducts. The slower salivary flow rate is caused by saliva in the submandibular glands flowing against gravity, and the dependent position of the gland makes it more prone to stasis. Additionally, owing to the higher calcium and phosphate levels, the saliva within the submandibular glands tends to be more alkaline and may induce sialolithiasis[2].
Sialoliths usually range from 1 mm to 10 mm in size, and those measuring 15 mm in one dimension are classified as giant sialoliths[3]. In this report, we present a case of giant right submandibular sialolithiasis that was treated by surgical ablation for approximately 30 years and compare various giant sialolith cases and their different treatments with respect to variables such as size, duration, and symptom presentation.
A 75-year-old woman presented to our institution with painless right submandibular swelling with a persistence of 30 years.
The clinical presentation was mostly asymptomatic, with only slight facial asymmetry and occasional right-sided aural fullness. However, the indurated mass began to manifest focal swelling 1 mo prior, with intermittent severe pain that radiated to the ipsilateral neck and contralateral face. The additional onset of dysphagia, odynophagia, and a subsequent decrease in appetite were also noted but without associated postprandial swelling or xerostomia.
The patient had no known medical history.
The patient denied alcohol or cigarette use and confirmed a family history of sialolithiasis.
Bimanual palpation revealed a raised right erythematous submandibular mass measuring 40 mm × 30 mm overlying the skin. The swelling was indurated, tender on palpation, and firm in consistency. No other obvious cervical lymphadenopathies could be palpated. Intraorally, no stones or purulent discharge was secreted from the Wharton’s duct.
White blood cells count levels were elevated (13800/µl).
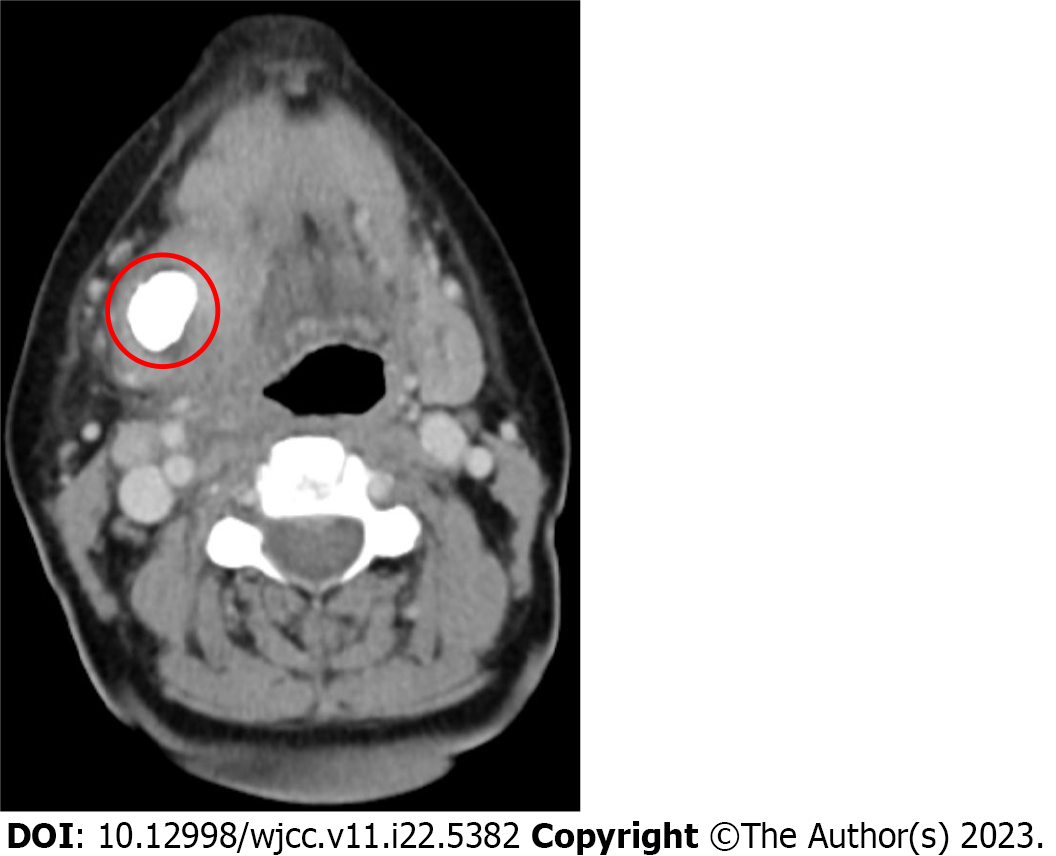
Computed tomography (CT) revealed a calcified mass measuring 35 mm × 20 mm within the right submandibular gland (Figure 1).
Combined with the patient’s medical history, the final diagnosis was submandibular sialolithiasis.
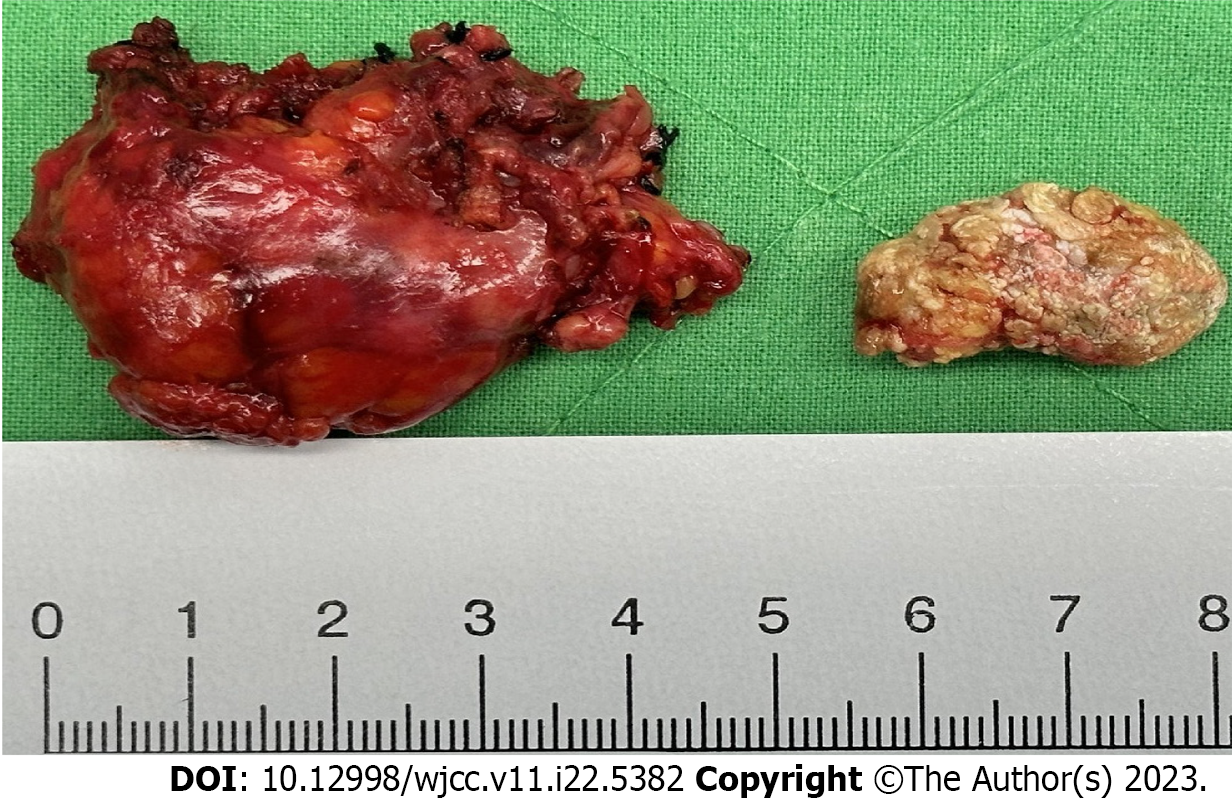
Excision of the right submandibular gland and sialoliths was performed using a standard extraoral approach. Intraoperative findings revealed that the right submandibular gland was indurated and filled with giant sialoliths. Neighboring structures, such as the hypoglossal, lingual, and marginal mandibular nerves, were preserved (Figure 2).
The postoperative was uneventful, with no complications. Histopathological examination confirmed the diagnoses of sialolithiasis and chronic sialadenitis. A giant, yellow, hard sialolith measuring 25 mm × 17 mm × 17 mm was noted. Microscopically, the submandibular gland showed varied dilatations of the salivary ducts (ductal ectasia). Ulcerative changes in the dilated ductal epithelium with areas of squamous metaplasia, periductal fibrosis, and moderately mixed acute and chronic inflammatory infiltrates with lymphocytic aggregate foci were also observed.
Several treatment modalities for submandibular sialolithiasis exist; however, the primary goal is to preserve gland function, maintain low risk, and reduce patient discomfort[4]. Non-invasive conservative measures for submandibular sialolithiasis include glandular focal massage and trans-oral removal. Glandular focal massage is important during or after the administration of sialagogues, and irrigation is primarily indicated in cases of small intraductal stones. Transoral removal can be considered if stones are palpated bimanually and/or localized within the perihilar region of the gland using ultrasonography[4,5]. If a superimposed infection is suspected, antibiotics should be prescribed and, when warranted, combined with simple sialolithotomy[5,6].
Invasive management of submandibular sialolithiasis consists of open surgery (which can be performed with transoral duct surgery[7-9] or a transcervical approach to the submandibular space[10], extracorporeal shock wave lithotripsy[11-15], interventional sialendoscopy, and intraductal shock-wave lithotripsy[16-19]. These invasive methods are recom
Transoral duct surgery may be considered for stones of all sizes in the papilla, owing to the narrow ostium of the papilla and stones in the distal and middle ducts. Small mobile stones (not exceeding 3-5 mm) in the papilla distal and middle ducts can also be extracted using interventional sialendoscopy. The proximal duct, however, is curved and narrow; thus, interventional sialendoscopy is difficult to perform. In cases where the stones are immobile, impacted, palpable, or large, transoral duct surgery is recommended, although mechanical fragmentation or intraductal shockwave lithotripsy followed by fragment extraction is also an option. Intraparenchymal stones are rare; however, if small, mobile stones (not exceeding 3–5 mm) can be visualized during endoscopy, interventional sialendoscopy, including mechanical fragmentation or intraductal shock wave lithotripsy, is recommended. Transoral duct surgery with submandibulectomy is indicated for large palpable stones ( 10 mm) located posthilar to the intraparenchymal region. Finally, salivary gland massage combined with a sour diet and sialogogue use is recommended after the removal of salivary stones[5].
In summary, transoral duct surgery offers better accessibility to the duct system and remains the preferred treatment modality; however, intraductal shock wave lithotripsy has gradually replaced transoral duct surgery in cases of smaller salivary stones. Compared with an earlier algorithm for the management of submandibular stones published in 2009, the indications for extracorporeal shockwave lithotripsy have since been adjusted, and the newly developed intraductal shockwave lithotripsy is also available. Although extracorporeal shockwave lithotripsy is considered less important, the procedure remains an option for intraparenchymal stones that are not visible or accessible. Finally, botulinum toxin injections may be considered in situations where the patient is deemed inoperable[7].
Among all the invasive treatment methods, adenectomy has a higher success rate than other techniques. Open surgery via the transcervical approach has a lower risk of infection because the oral space does not communicate with the neck space, whereas the intraoral approach avoids facial scarring. However, open surgical approaches are associated with several complications. Examples include postoperative neurological damage, particularly hypoglossal, lingual, and marginal mandibular nerve injuries, hemorrhage, hematoma, and disfiguring scars. Temporary marginal mandibular nerve damage is the most common complication of transcervical submandibular gland surgery. This complication was reported to be 36% by Smith et al[21], and permanent damage was reported to be as high as 12% by De et al[22]. in the literature. Beahm et al[23] reported rates between 7.7% and 36% in a previous literature revie. To reduce the risk of marginal mandibular nerve injury in the transcervical surgical approach to the submandibular gland, three surgical maneuvers are recommended: (1) The gland was identified to be lower than the hyoid bone, and the marginal mandibular nerve was not examined; (2) The marginal mandibular nerve is located at the level at which it leaves, tracks, and protects the parotid tail; and (3) The facial veins are located at a lower level and ligated, and the nerve is suspended by elevation; thus, the marginal mandibular nerve is removed from the surgical area.
However, Smith et al[21] reported that when a lower approach was used, no permanent marginal mandibular nerve palsy occurred, although 36% of the nerves were temporarily dysfunctional. This may have been due to stretching during the lower surgical approach to the glands. The hypoglossal nerve is partially sheltered by the posterior belly of the digastric muscle, which is located in the inferomedial portion of the lower one-third of the submandibular glands. This may explain why hypoglossal nerve damage has been reported very rarely (0%-1.4%)[24] compared with marginal mandibular nerve injuries. In this case report, no permanent or temporary complications occurred during the postoperative follow-up. Although the submandibular glands contribute 69% of the salivary secretion volume in the resting state[25], xerostomia was not reported in our case. This could be explained by the fact that other salivary glands were sufficiently functional to compensate for the resected glands.
Moreover, regarding the oncological risk to which patients with chronic inflammation and lithiasis are exposed[26], we reviewed some studies on salivary gland tumors. Most salivary gland tumors arise in the parotid gland (70%), followed by the minor salivary glands (22%) and submandibular glands (8%)[27]. Differential diagnoses for benign submandibular tumors include pleomorphic adenomas, Warthin’s tumors, and oncocytomas. Histopathological characteristics can be used to distinguish between them. Pleomorphic adenomas are characterized by thick irregularly marginated capsules[28,29]. Oncocytomas have thin capsules and monomorphic oncocytes without mitosis or necrosis[29,30]. The lymphatic population is the most common cytology and histology of Warthin's tumor[28,29]. Histopathological examination of our patient did not reveal the above characteristics, and the characteristics of malignant transformation include local invasion into the muscular, perineural, and lymphatic structures, as well as microscopic features, including nuclear atypia, cellular polymorphism, mitoses, and focal necrosis, were absent too. Thus, salivary gland tumors were excluded.
Owing to the similarities in the clinical presentation of benign salivary tumors and submandibular sialolithiasis, radiological imaging is essential to distinguish between the two entities. Ultrasound is recommended for the initial assessment of salivary gland abnormalities; however, ultrasound is insufficient because information on the surrounding structures cannot be provided. Its accuracy in the identification of benign salivary lesions can be increased using elastography or contrast-enhanced ultrasound; however, the European Federation of Societies for Ultrasound in Medicine and Biology do not recommend contrast-enhanced ultrasound for the characterization of salivary gland lesions in clinical practice. Thus, further studies are required to investigate the diagnostic roles of contrast-enhanced ultrasound and elastography in the evaluation of salivary gland lesions. Corvino et al[26] described the utility of CT and magnetic resonance imaging in the initial staging, histologic grading of salivary gland malignancies, and preoperative planning. Positron emission tomography with F-18 fluorodeoxyglucose is useful for the evaluation and clinical management of head and neck lesions[26].
Giant sialoliths are rare and classified as those measuring 15 mm in one dimension[3]. We compared cases of giant sialoliths in the submandibular gland from 1981 to 2022 and their different treatments according to variables such as size, duration, and symptom presentation. The cases and their details are listed in Table 1.
| Ref. | Year | Size (mm) | Symptoms/signs | Duration | Treatment | Complication |
| Zakaria[35] | 1981 | 33 | Swelling in the right submandibular region, increasing pain during meals | 20 yr | The right submandibular gland was excised | None |
| Naraynsingh[36] | 1985 | 60 | Painless hard left submandibular swelling | 3 yr | Incision of left submandibular gland via a transcervical approach | None |
| Frame and Smith[37] | 1986 | 30 | Recurrent pain and swelling of the right side of the face | N/A | Excise the gland and calculus | None |
| 25 | Slight discomfort in the area | N/A | Sialo-adenectomy via a standard incision | None | ||
| Kaltman and Eichner[38] | 1987 | 45 | Pain and swelling over the left submandibular area | 15 yr | Standard extraoral approach | None |
| Raveenthiran and Hayavadana Rao[39] | 2004 | 35 | Painless swelling in the floor of her mouth | N/A | Transoral sialolithotomy | None |
| Yildirim[40] | 2004 | 30 | Huge, firm mass below the right angle of the mandible | N/A | Excised via extraoral approach | None |
| Chan and Patel[41] | 2006 | 35 | Painful mass in the left floor of the mouth | N/A | Transoral sialodochoplasty and removal calculus | None |
| Graziani et al[42] | 2006 | 22 | Asymptomatic | N/A | Transorally | None |
| Ledesma-Montes et al[43] | 2007 | 36 | Painful mass located on the right side of the floor of the mouth | 12 yr | Surgical excision of the sialolith | None |
| Biddle and Arora[44] | 2008 | 26 | Persistent draining wound over the right submandibular region, odynophagia, and dysphagia were noted | 2 yr | Excised via standard incision | None |
| Rai and Burman[45] | 2009 | 72 | Episodes of pain for last 2 yr, but severe pain and swelling in the left lower submandibular region | 1 mo | Sialolithotomy with sialodochoplasty via an intraoral approach | None |
| Soares et al[46] | 2009 | 25 | Hard elongated mass along the right Wharton’s duct and a reduced salivary flow | 4 mo | Dissected with the patient under local anesthesia | None |
| Rivera-Serrano and Schaitkin[47] | 2011 | 23 | Chronic unrelenting purulent discharge from bilateral submandibular ducts | N/A | Transoral sialolithotomy approach | None |
| Krishnan et al[48] | 2009 | 34 | Recurrent pain and swelling | 8 yr | Transoral approach | None |
| Emir et al[49] | 2010 | 35 | Mass on the right side of the floor of the mouth and fistulization of the Wharton duct into the oral cavity | N/A | Removed transorally from the opening of the fistula at the floor of the mouth | None |
| Shetty and Sharma[50] | 2010 | 27 | Firm painful swelling in the left submandibular region | 1 mo | Gentle extraction | None |
| Boffano and Gallesio[51] | 2010 | 22 | Swelling and pain in the submandibular right region | N/A | Removal of the stone and sialodochoplasty were done via an intraoral approach | None |
| Arunkumar et al[52] | 2015 | 20 | Recurrent right submandibular swelling with pain during meals and gradual regression | 8 mo | Removed intraorally | None |
| Pandarakalam et al[53] | 2013 | 40 | Swelling, gradually increased in size and became painful recently | 4 yr | Excision of the right submandibular salivary gland | None |
| Iqbal et al[54] | 2012 | 35 | Hard swelling in the anterior oral floor of mouth | N/A | Intraoral incision | None |
| Ben-Shoshan and Lacroix[31] | 2014 | 17 | Mild pain in the submandibular area | 1 yr | Fell out without any intervention | None |
| Gupta et al[3] | 2013 | 28 | Intermittent, dull aching pain, and swelling in left submandibular area | 3 mo | Intraoral approach | None |
| Bhullar et al[55] | 2015 | 31 | Pain in the left submandibular region associated with meals | 6 mo | Transoral sialolithotomy | None |
| Akinyamoju and Adisa[32] | 2015 | 44 | Hard, painless, left floor of mouth swelling, moderate pain at mealtimes | 1 yr | Removed non-surgically | None |
| Shahoon et al[56] | 2015 | 55 | Difficulty breathing and a foul-tasting mouth since 21 days previously with history of right submandibular swelling episodes | 21 d | Surgical removal | None |
| Arslan et al[57] | 2015 | 35 | Recurrent pain, swelling, and redness in the left submandibular area | 6 mo | Submandibular gland resection | None |
| Oliveira et al[58] | 2016 | 30 | Pain over the right floor of mouth and submandibular region | N/A | Excision of the right submandibular gland and stone via standard extraoral approach | None |
| Weinberg and Albers[59] | 2016 | 38 | Swelling at the submandibular region, pus from Wharton’s duct was noted | N/A | Excision | None |
| Gadve et al[60] | 2016 | 25 | Pain and swelling in the floor of mouth on the left side | 1 mo | Remove the sialolith surgically | None |
| Goh et al[61] | 2016 | 35 | Left submandibular swelling, increasing pain, fever and discharge was noted | 5 yr | Submandibulectomy with transcervical approach | None |
| Omezli et al[62] | 2016 | 37 | Painful and persistent purulent discharge from unilateral submandibular ducts | N/A | Intraoral approach | None |
| Lim et al[63] | 2017 | 50 | Right submandibular swelling, increased in size rapidly causing discomfort and pain | 10 yr | Right submandibulectomy | None |
| Iwai et al[64] | 2017 | 41 | Right submandibular swelling several times | 40 yr | Submandibular sialoadenectomy | None |
| Sakthivel et al[65] | 2017 | 50 | Recurrent pain and swelling in the right submandibular region | 6 mo | Intraoral removal of stone | None |
| Rodrigues et al[33] | 2017 | 45 | Painless mass in the neck | 3 yr | Removed without anesthesia or surgical excision | None |
| Singh et al[66] | 2020 | 42 | Swelling over right side of floor of mouth and pain during meals | 2 yr | Sialolithotomy and marsupialization of Wharton's duct | None |
| Abraham et al[67] | 2021 | 40 | Hard mass beneath the tongue with occasional dull pain | N/A | Transoral surgical removal of the right submandibular calculus | None |
| Thong et al[68] | 2021 | 25 | Right submandibular swelling | 2 wk | Excision of right submandibular gland | None |
| Kumar et al[69] | 2021 | 28 | Firm mass below the left angle of the mandible | 4 yr | Excision of the left submandibular gland and stone via trans-cervical approach | None |
| Brooks et al[34] | 2021 | 16&19 | Firm, ovoid swelling in the floor of the mouth approximate to the left sublingual caruncle with thin, slightly pale overlying mucosa | N/A | Patient declined any additional diagnostic measures | None |
| Ungari et al[70] | 2022 | 23 | Painful swelling in the left side of the mouth floor | 20 yr | Excision of the left submandibular gland and stone via trans-cervical approach | None |
| Mohsin et al[71] | 2022 | 28 | Moveable, firm, extensive non-tender swelling in the posterior floor of the mouth | 15 yr | Incision of the right submandibular duct’s longitudinal axis and removed the stones | None |
Between 1981 and 2022, 44 giant sialoliths were noted. The mean giant sialoliths size is 34.70 mm (two cases were within the range of 15-19 mm; 14 cases within 20-29 mm; 15 cases within 30-39 mm; seven cases within 40-49 mm; three cases within 50-59 mm; one case within 60-69 mm and one case within the range 70-79 mm). The median duration of giant sialoliths was 2 years (11 cases were less than a year; 9 cases were within the range of 1-5 years; two cases were within 6-10 years; three cases were within the range of 11-15 years; two cases were within the range of 16-20 years; one case was within the range of 36-40 years; and 15 cases did not discuss the duration). Of the 43 tumors, 23 and 21 were located in the right and left submandibular glands, respectively. Of the giant sialoliths, 90.70% were surgically removed (incision or excision), either intra-orally or extra-orally (transcervical), whereas 9.30% were removed using other methods. The patients with giant sialoliths reported by Ben-Shoshan and Lacroixl[31] did not undergo any intervention. Akinyamoju and Adisa[32] and Rodrigues et al[33] removed the stones non-surgically. Brooks et al[34] reported that a patient declined any additional diagnostic measures and was lost at follow-up. No postoperative complications were observed in these cases.
Giant sialoliths are rare, and their longer durations have rarely been documented. This report presents a case of long-term, rare, and giant sialolithiasis within the submandibular gland parenchyma for 30 years in an older adult. Our patient presented with typical clinical and radiographic findings. In this case, the infection and fibrosis of the affected gland and size of the stone provided us with no other alternatives except for the excision of the involved gland. Thus, right submandibular sialoadenectomy was performed via the transcervical approach. After the surgery, the patient recovered smoothly without any complaints, side effects, or complications. Based on the comparative table, this is the second largest case with a long duration that we would like to share. This case highlights the importance of proper diagnosis and treatment. Clinicians are advised to tailor management according to the patient and to keep in mind that the primary goal should always be to preserve gland function, maintain low risk, and reduce patient discomfort.
| 1. | McKenna JP, Bostock DJ, McMenamin PG. Sialolithiasis. Am Fam Physician. 1987;36:119-125. [PubMed] |
| 2. | Burket LW, Greenberg MS, Glick M, Ship JA. Burket’s oral medicine. 11th ed. United States: PMPH USA, 2008: 201-202. |
| 3. | Gupta A, Rattan D, Gupta R. Giant sialoliths of submandibular gland duct: Report of two cases with unusual shape. Contemp Clin Dent. 2013;4:78-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Zenk J, Constantinidis J, Al-Kadah B, Iro H. Transoral removal of submandibular stones. Arch Otolaryngol Head Neck Surg. 2001;127:432-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 102] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Zenk J, Gottwald F, Bozzato A, Iro H. [Submandibular sialoliths. Stone removal with organ preservation]. HNO. 2005;53:243-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Williams MF. Sialolithiasis. Otolaryngol Clin North Am. 1999;32:819-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 118] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Koch M, Mantsopoulos K, Müller S, Sievert M, Iro H. Treatment of Sialolithiasis: What Has Changed? An Update of the Treatment Algorithms and a Review of the Literature. J Clin Med. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 8. | McGurk M, Makdissi J, Brown JE. Intra-oral removal of stones from the hilum of the submandibular gland: report of technique and morbidity. Int J Oral Maxillofac Surg. 2004;33:683-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Capaccio P, Torretta S, Ottavian F, Sambataro G, Pignataro L. Modern management of obstructive salivary diseases. Acta Otorhinolaryngol Ital. 2007;27:161-172. [PubMed] |
| 10. | Goh YH, Sethi DS. Submandibular gland excision: a five-year review. J Laryngol Otol. 1998;112:269-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 52] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Iro H, Zenk J, Waldfahrer F, Benzel W, Schneider T, Ell C. Extracorporeal shock wave lithotripsy of parotid stones. Results of a prospective clinical trial. Ann Otol Rhinol Laryngol. 1998;107:860-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Capaccio P, Ottaviani F, Manzo R, Schindler A, Cesana B. Extracorporeal lithotripsy for salivary calculi: a long-term clinical experience. Laryngoscope. 2004;114:1069-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 40] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Escudier MP, Brown JE, Drage NA, McGurk M. Extracorporeal shockwave lithotripsy in the management of salivary calculi. Br J Surg. 2003;90:482-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 56] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Zenk J, Bozzato A, Winter M, Gottwald F, Iro H. Extracorporeal shock wave lithotripsy of submandibular stones: evaluation after 10 years. Ann Otol Rhinol Laryngol. 2004;113:378-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 15. | Katz P. [New techniques for the treatment of salivary lithiasis: sialoendoscopy and extracorporal lithotripsy: 1773 cases]. Ann Otolaryngol Chir Cervicofac. 2004;121:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Marchal F, Dulguerov P, Becker M, Barki G, Disant F, Lehmann W. Specificity of parotid sialendoscopy. Laryngoscope. 2001;111:264-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 158] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 17. | Marchal F, Dulguerov P, Becker M, Barki G, Disant F, Lehmann W. Submandibular diagnostic and interventional sialendoscopy: new procedure for ductal disorders. Ann Otol Rhinol Laryngol. 2002;111:27-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 106] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Nahlieli O, Shacham R, Bar T, Eliav E. Endoscopic mechanical retrieval of sialoliths. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:396-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Koch M, Zenk J, Iro H. [Diagnostic and interventional sialoscopy in obstructive diseases of the salivary glands]. HNO. 2008;56:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Faizal B, Gangadharan S, Thankappan K. Comparison between Sialendoscopy and Conventional Methods in the Treatment of Sialolithiasis. Malays J Med Sci. 2017;24:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Smith WP, Peters WJ, Markus AF. Submandibular gland surgery: an audit of clinical findings, pathology and postoperative morbidity. Ann R Coll Surg Engl. 1993;75:164-167. [PubMed] |
| 22. | De M, Singh PK, Johnson AP. Morbidity associated with submandibular gland excision: a retrospective analysis. Internet J Anesthesiol 2006; 1. [DOI] [Full Text] |
| 23. | Beahm DD, Peleaz L, Nuss DW, Schaitkin B, Sedlmayr JC, Rivera-Serrano CM, Zanation AM, Walvekar RR. Surgical approaches to the submandibular gland: a review of literature. Int J Surg. 2009;7:503-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Springborg LK, Møller MN. Submandibular gland excision: long-term clinical outcome in 139 patients operated in a single institution. Eur Arch Otorhinolaryngol. 2013;270:1441-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Schneyer LH, Levin LK. Rate of secretion by individual salivary gland pairs of man under conditions of reduced exogenous stimulation. J Appl Physiol. 1955;7:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Corvino A, Caruso M, Varelli C, Di Gennaro F, Pignata S, Corvino F, Vallone G, Catalano O. Diagnostic imaging of parotid gland oncocytoma: a pictorial review with emphasis on ultrasound assessment. J Ultrasound. 2021;24:241-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Lee TH, Lin YS, Lee WY, Wu TC, Chang SL. Malignant transformation of a benign oncocytoma of the submandibular gland: a case report. Kaohsiung J Med Sci. 2010;26:327-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Eneroth CM. Oncocytoma of major salivary glands. J Laryngol Otol. 1965;79:1064-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Chen B, Hentzelman JI, Walker RJ, Lai JP. Oncocytoma of the Submandibular Gland: Diagnosis and Treatment Based on Clinicopathology. Case Rep Otolaryngol. 2016;2016:8719030. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Brandwein MS, Huvos AG. Oncocytic tumors of major salivary glands. A study of 68 cases with follow-up of 44 patients. Am J Surg Pathol. 1991;15:514-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 116] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Ben-Shoshan M, Lacroix Y. A giant sialolith in a 16-year-old boy presenting to the emergency room. Arch Dis Child. 2014;99:883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Akinyamoju AO, Adisa AO. Non-surgical extraction of a massive sialolith in the Wharton's duct of a Nigerian. Afr J Med Med Sci. 2015;44:177-180. [PubMed] |
| 33. | Rodrigues GHC, Carvalho VJG, Alves FA, Domaneschi C. Giant submandibular sialolith conservatively treated. Autops Case Rep. 2017;7:9-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Brooks JK, Macauley MR, Price JB. Concurrent giant sialoliths within the submandibular gland parenchyma and distal segment of Wharton's duct: Novel case report. Gerodontology. 2021;38:437-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 35. | Zakaria MA. Giant calculi of the submandibular salivary gland. Br J Oral Surg. 1981;19:230-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Naraynsingh V. Giant submandibular gland calculi. J Oral Maxillofac Surg. 1985;43:384-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 37. | Frame J. W. and A. J. Smith. Large calculi of the submandibular salivary glands. International journal of oral and maxillofacial surgery 15.6 (1986): 769-771. |
| 38. | Kaltman S, Eichner M. Giant sialolithiasis appearing as odontogenic infection. J Am Dent Assoc. 1987;115:425-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 39. | Raveenthiran V, Hayavadana Rao PV. Giant calculus in the submandibular salivary duct: report of the first prepubertal patient. Pediatr Surg Int. 2004;20:163-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 40. | Yildirim A. A case of giant sialolith of the submandibular salivary gland. Ear Nose Throat J. 2004;83:360-361. [PubMed] |
| 41. | Chan EK, Patel ND. Giant calculus of the submandibular salivary duct. Ear Nose Throat J. 2006;85:306, 308. [PubMed] |
| 42. | Graziani F, Vano M, Cei S, Tartaro G, Mario G. Unusual asymptomatic giant sialolith of the submandibular gland: a clinical report. J Craniofac Surg. 2006;17:549-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 43. | Ledesma-Montes C, Garcés-Ortíz M, Salcido-García JF, Hernández-Flores F, Hernández-Guerrero JC. Giant sialolith: case report and review of the literature. J Oral Maxillofac Surg. 2007;65:128-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 44. | Biddle RJ, Arora S. Giant Sialolith of the Submandibular Salivary Gland. Radiol Case Rep. 2008;3:101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 45. | Rai M, Burman R. Giant submandibular sialolith of remarkable size in the comma area of Wharton's duct: a case report. J Oral Maxillofac Surg. 2009;67:1329-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 46. | Soares EC, Costa FW, Pessoa RM, Bezerra TP. Giant salivary calculus of the submandibular gland. Otolaryngol Head Neck Surg. 2009;140:128-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | Rivera-Serrano CM, Schaitkin BM. Bilateral giant submandibular sialoliths and the role for salivary endoscopy. Am J Otolaryngol. 2011;32:85-87. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 48. | Krishnan B, Gehani RE, Shehumi MI. Submandibular giant sialoliths-2 case reports and review of the literature. Indian J Otolaryngol Head Neck Surg. 2009;61:55-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 49. | Emir H, Kaptan ZK, Uzunkulaoglu H, Dogan S. A rare case of asymptomatic bilateral submandibular gland sialolithiasis: a giant, fistulized calculus on the right and multiple calculi on the left. Ear Nose Throat J. 2010;89:502-504. [PubMed] |
| 50. | Shetty BN, Sharma P. Unusual case of a projecting intraoral giant sialolith. Indian J Surg. 2010;72:155-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 51. | Boffano P, Gallesio C. Surgical treatment of a giant sialolith of the Wharton duct. J Craniofac Surg. 2010;21:134-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 52. | Arunkumar KV, Garg N, Kumar V. Oversized submandibular gland sialolith: a report of two cases. J Maxillofac Oral Surg. 2015;14:116-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 53. | Pandarakalam C, Goebel WM, Seyer B. Chronic sclerosing sialadenitis or Küttner's tumor associated with a giant sialolith: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:e38-e40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 54. | Iqbal A, Gupta AK, Natu SS. Unusually large sialolith of Wharton's duct. Ann Maxillofac Surg. 2012;2:70-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 55. | Bhullar RS, Dhawan A, Bhullar K, Malhotra S. Giant submandibular gland duct sialolith mimicking an impacted canine tooth. Natl J Maxillofac Surg. 2015;6:89-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 56. | Shahoon H, Farhadi S, Hamedi R. Giant sialoliths of Wharton duct: Report of two rare cases and review of literature. Dent Res J (Isfahan). 2015;12:494-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 57. | Arslan S, Vuralkan E, Çobanog˘lu B, Arslan A, Ural A. Giant sialolith of submandibular gland: report of a case†. J Surg Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 58. | Oliveira Tde P, Oliveira IN, Pinheiro EC, Gomes RC, Mainenti P. Giant sialolith of submandibular gland duct treated by excision and ductal repair: a case report. Braz J Otorhinolaryngol. 2016;82:112-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 59. | Weinberg A, Albers AE. Giant sialolith after submandibulectomy. Pan Afr Med J. 2016;25:228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 60. | Gadve V, Mohite A, Bang K, Shenoi SR. Unusual giant sialolith of Wharton's duct. Indian J Dent. 2016;7:162-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 61. | Goh LC, Chitra BK, Shaariyah MM, Ng WS. Transcervical approach to the removal of a deep-seated giant submandibular calculus and the submandibular gland. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 62. | Omezli MM, Ayranci F, Sadik E, Polat ME. Case report of giant sialolith (megalith) of the Wharton's duct. Niger J Clin Pract. 2016;19:414-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 63. | Lim EH, Nadarajah S, Mohamad I. Giant Submandibular Calculus Eroding Oral Cavity Mucosa. Oman Med J. 2017;32:432-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 64. | Iwai T, Izumi T, Ohya T, Oguri S, Tohnai I. Giant Sialolith of the Submandibular Gland. J Clin Diagn Res. 2017;11:ZJ03-ZJ04. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 65. | Sakthivel P, Yogal R, Singh S, Sharma P, Singh CA. Giant Sialolith of Submandibular Duct. JNMA J Nepal Med Assoc. 2017;56:262-264. [PubMed] |
| 66. | Singh AK, Yeola M, Raghuvanshi P, Singh N. Giant Wharton's duct sialolithiasis causing sialo-oral fistula: a rare case report with literature review. J Family Med Prim Care. 2020;9:5793-5795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 67. | Abraham ZS, Mathias M, Kahinga AA. Unusual giant calculus of the submandibular duct: Case report and literature review. Int J Surg Case Rep. 2021;84:106139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 68. | Thong HK, Othman IA, Ramli R, Sabir Husin Athar PP. Painless Giant Submandibular Gland Sialolith: A Case Report. Cureus. 2021;13:e19429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 69. | Kumar ND, Sherubin JE, Bagavathy K. Sialolithiasis: An Unusually Large Salivary Stone. J Maxillofac Oral Surg. 2021;20:227-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 70. | Ungari C, Cicconetti A, Cerbelli E, Sulpasso A, Filiaci F. Giant submandibular sialolith: a case report. Clin Ter. 2022;173:217-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 71. | Mohsin SF, Riyaz MA, Alqazlan AA. Detection and Management of Giant Submandibular Gland Sialolith. Pak J Med Sci. 2022;38:2030-2033. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corvino A, Italy; Ozcan C, Turkey S-Editor: Lin C L-Editor: A P-Editor: Zhao S