Published online Aug 6, 2023. doi: 10.12998/wjcc.v11.i22.5358
Peer-review started: April 14, 2023
First decision: June 21, 2023
Revised: June 22, 2023
Accepted: July 10, 2023
Article in press: July 10, 2023
Published online: August 6, 2023
Processing time: 111 Days and 2.7 Hours
The combined anterior/posterior approach appears to be capable of recons
We describe a case of a 16-year-old female patient with severe thoracolumbar fracture and dislocation underwent surgery assisted by the TINAVI robot. A one-stage combined anterior and posterior operation was performed on a severe thoracolumbar fracture dislocation using the TINAVI robot, and the operation was completed in right lateral position.
The TINAVI robot-assisted one-stage anterior and posterior surgery in right lateral position for severe thoracolumbar fracture and dislocation is both safe and effective.
Core Tip: Currently, there is no reports describing TINAVI robot-assisted single lateral position anteroposterior surgery for thoracolumbar fracture dislocation. We describe a case of a 16-year-old female patient with severe thoracolumbar fracture and dislocation underwent surgery assisted by the TINAVI robot. A one-stage combined anterior and posterior operation was performed on a severe thoracolumbar fracture dislocation using the TINAVI robot, and the operation was completed in right lateral position. We hope to bring more options to the approach of spinal surgery by sharing the case.
- Citation: Ye S, Chen YZ, Zhong LJ, Yu CZ, Zhang HK, Hong Y. TINAVI robot-assisted one-stage anteroposterior surgery in lateral position for severe thoracolumbar fracture dislocation: A case report. World J Clin Cases 2023; 11(22): 5358-5364
- URL: https://www.wjgnet.com/2307-8960/full/v11/i22/5358.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i22.5358
Thoracolumbar fracture-dislocation is a high-energy spinal injury caused by compression or flexion/traction force[1]. Simple anterior or posterior surgery cannot completely decompress and reconstruct the stability of the three columns of the spine in severe thoracolumbar fracture and dislocation[2]. The combination of anterior and posterior surgery is an effective method for treating severe thoracolumbar fracture and dislocation. The combined anterior and posterior approach of thoracolumbar fracture and dislocation, on the other hand, frequently requires changing the position during the operation, resulting in a longer operation time. If the anterior and posterior operations are only performed in a lateral position, pedicle screw placement becomes more difficult, and frequent fluoroscopy is required to confirm screw accuracy, resulting in a longer operation time[3,4]. In addition, inaccurate placement of pedicle screws may lead to several complications, such as peripheral neurovascular injury, cerebrospinal fluid leakage, thoracic and abdominal organ injury, and so on[5,6]. To improve the accuracy of screw placement location in thoracolumbar pedicle screw fixation surgery, several robotic systems for have been used in clinical surgery[7].
As a universal surgical robot, TINAVI robot has achieved good surgical results in clinical surgery[8-13]. TINAVI robot-assisted one-stage anterior posterior surgery for severe thoracolumbar fracture dislocation may be safe and effective[10]. It can accurately insert pedicle screws, reducing operation time and tissue damage. This was, to the best of our knowledge, the first case of TINAVI robot-assisted single lateral position anteroposterior surgery for thoracolumbar fracture-dislocation. The patients and their families were informed that the case data would be submitted for publication and consented.
A 16-year-old girl suffered back pain from falling from a height 6 d ago.
The patient had no prior history with regard to the lesion.
The patient had no specific history of past illness.
The patient had no known personal or family medical history.
Localized back tenderness, kyphosis and restricted mobility. ASIA B of spinal cord injury. There was an open fracture of left ankle joint. The patient was bedridden and the rest of the examination could not be coordinated.
All ordered laboratory tests (complete blood count, basic metabolic panel, lipid panel, liver panel, coagulation tests, urinalysis, and stool analysis) were normal.
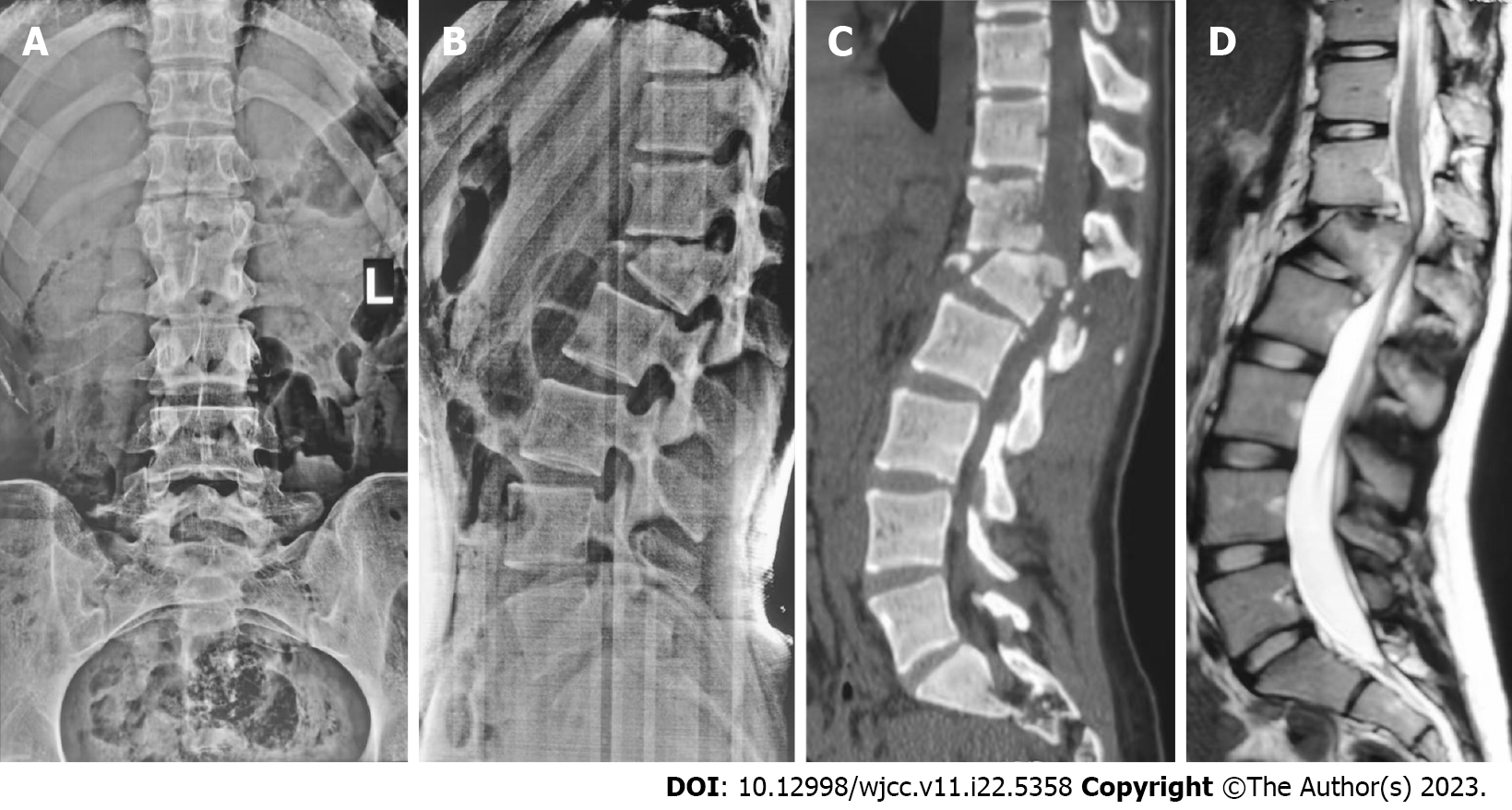
Anteroposterior, lateral, and computed tomography (CT) views revealed a classic kyphosis with a fracture dislocation of L1 (AO Type C, Load-sharing classification = 8). The kyphotic deformity's corresponding Cobb angle was approximately 26°. The spinal cord injury was discovered using magnetic resonance imaging (Figure 1). Besides, there were open fracture of left ankle joint, and fracture of right ankle joint.
The patient was diagnosed with L1 fracture combined with spinal cord injury, accompanied by bilateral ankle fractures.
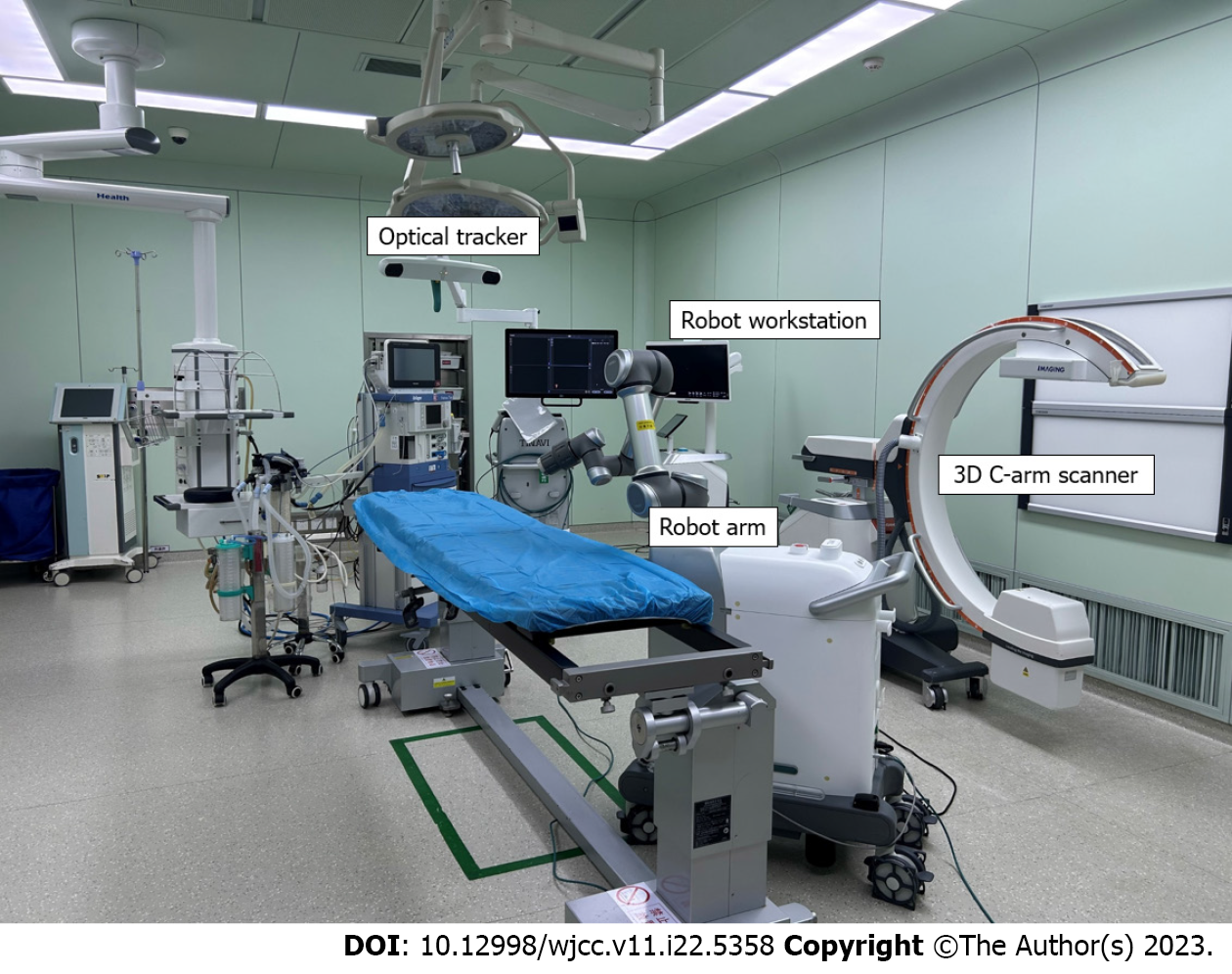
In the first step, we would treat thoracolumbar fracture dislocation with TINAVI robot-assisted lateral position combined with anteroposterior surgery, and in the second step, we would complete the operation on bilateral ankle fracture (Figure 2).
The surgical technique for the treatment of thoracolumbar fracture dislocation was described as follows:
General anesthesia was administered. The patient was positioned in the right lateral position on a carbon fiber surgical bed with hip and knee flexion. The posterior axillary line was marked as a reference point for subsequent steps.
A C-arm fluoroscopy machine was used to assist in precise positioning during the procedure. The fluoroscopy line was set perpendicular to the posterior axillary line and passed through the injured vertebra. The intersection point of the was marked, creating an anterior incision marker line approximately 8 cm.
A tracker was attached to the left iliac crest to enable accurate tracking of the patient's movements during the procedure. A 3D C-arm scan was performed to obtain a detailed image of the target vertebra. The 3D image was transferred to the robot workstation for automatic registration and further planning.
Using the 3D image, the surgeon planned the placement of percutaneous pedicle screws in the T12 and L2 vertebrae. The plan included determining the screw entry point, direction, and specification. The position of the robot arm was adjusted according to the planned trajectory.
After the robot arm was correctly positioned, a guide cannula was inserted along the robot arm guide. The surgeon marked the position for implantation on the skin and made a longitudinal incision. The guiding cannula was used to fully expand the soft tissue, ensuring contact with the bony surface. The guiding pin of an electric drill was implanted along the direction of the guiding cannula to create a pathway for the pedicle screws. The guiding cannula was then removed, and the same procedure was repeated to implant the remaining guiding pins. C-arm fluoroscopy was used to verify the proper position of the guide pins.
The surgeon reached the injured vertebra directly by separating the physiologic space between the abdominal vascular sheath and the anterior border of the psoas major muscle. This approach allowed direct access to the surgical site while minimizing disruption to surrounding structures.
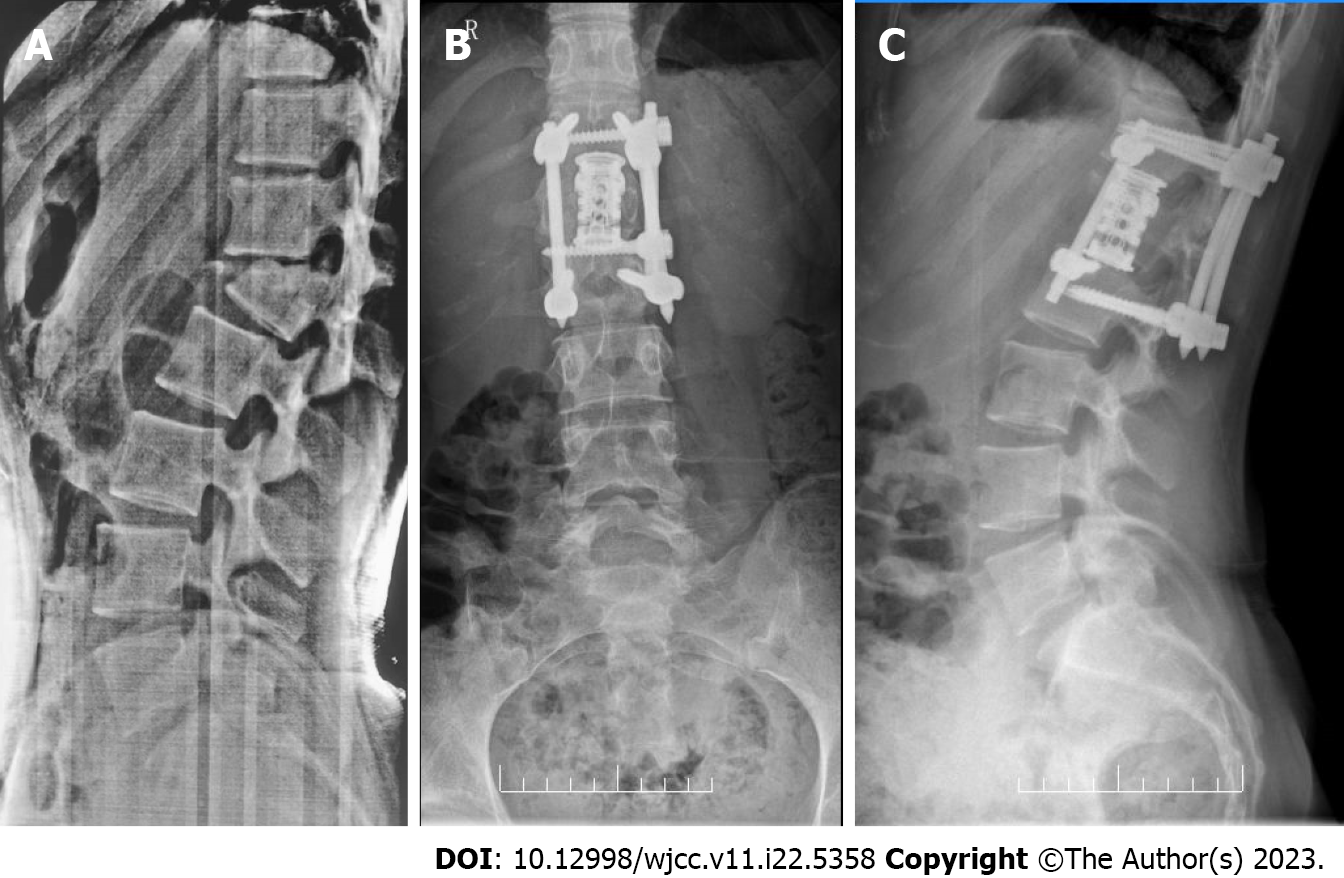
The operation was completed within the dilated channel using the oblique lateral interbody fusion channel and light source system. The transverse artery in the vertebral body was cauterized using a bipolar device. The periosteum was peeled off to fully expose the pedicle and intervertebral foramen. Special care was taken to protect the spinal nerve passing through the foramen. A corpectomy was performed on the L1 vertebra and adjacent intervertebral disc to achieve punctate bleeding and decompress the spinal cord. The bone mass in the spinal canal was carefully scraped off, relieving dural compression. The upper and lower vertebral bodies were stretched to achieve reduction. An artificial vertebral body was created using autogenous bone, and an vertebral screw rod system was installed. A drainage tube was routinely implanted to assist with fluid drainage during the initial postoperative period. To ensure stability and consolidation, image-guided transpedicular screws were inserted in the T12 and L2 vertebrae. The operation lasted 270 min and resulted in a blood loss of 400 mL. We used antibiotics for 24 h to prevent infection and removed the drainage tube when the drainage volume was less than 50 mL. During the operation, there were no complications (Figure 3).
After 5 mo of observation, the Cobb angle was 5.6°. There was no obvious loss of Cobb angle, no signs of nonunion, and neural function improved from ASIA B to ASIA D (Figure 4).
Thoracolumbar fracture-dislocation is frequently associated with nerve injury[1], which can be treated with either anterior or posterior surgery[14]. However, according to the load-sharing classification, posterior internal fixation may fail in cases of thoracolumbar burst fractures greater than 7 points[15]. Furthermore, posterior ligament reduction can reduce severe thoracolumbar fractures satisfactorily, but the sign of unstable healing accounted for 59.6%[16]. Moreover, the anterior operation was unable to stabilize the spine's posterior column[17]. As a result, either an anterior or posterior approach alone would be ineffective for treating severe thoracolumbar fracture dislocation.
It is a reliable method to perform anterior and posterior surgery simultaneously for severe thoracolumbar fracture and dislocation, which can achieve full decompression and better nerve recovery[2]. The preoperative Cobb angle for thoracolumbar kyphosis was 26°, and the postoperative Cobb angle was 5°. After 5 mo of observation, the Cobb angle was 5.6°. There was no obvious loss of Cobb angle, no signs of nonunion, and neural function improved from ASIA B to ASIA D.
Traditional surgery without robot assistance takes longer time. Besides, the operator must master the technology of lateral pedicle screw insertion, which has more technical requirements for the surgeon. As a result, we attempt to perform anterior and posterior surgery for severe thoracolumbar fracture dislocation using the TINAVI robot and pedicle screw implantation. There is no report that we are aware of that describes the treatment of severe thoracolumbar fracture dislocation with one-stage lateral anterior posterior combined surgery using the TINAVI robot.
Pedicle screw implantation accuracy was 85.8%-96.2% for "perfect" and 93.4%-96.7 for "clinically acceptable"[18,19]. Based on 3D images, the TINAVI robot system can significantly improve surgical accuracy and safety in pedicle screw fixation. The electric drill is not only easy to implant with the guiding pin along the direction of the guiding cannula under the accurate positioning guidance of the TINAVI robot, but it also does not require frequent fluoroscopy. Tissue trauma and operation time are significantly reduced. The screws at the rostral can be planned to tilt up and the screws at the distal can be planned to tilt down as much as possible, which may enable in the placement of the front screw.
At the end of 2016, the TINAVI robot developed in China was certified by the National Food and Drug Administration. Subsequently, it began to be officially applied in clinical practice and gradually expanded to the field of spinal surgery. Han et al[10] compared the safety and efficacy of robot assisted thoracolumbar surgery with the conventional fluo
This case report has some limitations. The number of cases is small, the follow-up time is short, and the results still need to be verified by larger samples and longer follow-up studies. In addition, the current cost of using TINAVI robot is still relatively high, and further research is needed to quantify the clinical benefits of its use.
To summarize, the TINAVI robot-assisted one-stage anterior and posterior surgery in right lateral position for severe thoracolumbar fracture and dislocation is both safe and effective. It can insert pedicle screws precisely, reduce surgical time, and reduce tissue damage, and is expected to gradually become widely used in orthopedic clinical surgery in the future.
We thanked Professor Fei Zou from the Department of Orthopaedics of Huashan Hospital affiliated to Fudan University for providing guidance for this operation.
| 1. | Wang F, Zhu Y. Treatment of complete fracture-dislocation of thoracolumbar spine. J Spinal Disord Tech. 2013;26:421-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Xia Q, Xu BS, Zhang JD, Miao J, Li JG, Zhang XL, Zhou J. Simultaneous combined anterior and posterior surgery for severe thoracolumbar fracture dislocations. Orthop Surg. 2009;1:28-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Zhang B, Wang JC, Jiang YZ, Song QP, An Y. Effectiveness and postoperative rehabilitation of one-stage combined anterior-posterior surgery for severe thoracolumbar fractures with spinal cord injury. World J Clin Cases. 2022;10:6001-6008. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Ma Y, Deng SC, Jia ZH, Hao YH. Lateral position one-stage combined anteroposterior approach versus posterior approach with subtotal corpectomy, decompression, and reconstruction of spine in the treatment of thoracolumbar burst fractures. Zhonghua Yi Xue Za Zhi. 2013;93:2112-2116. [PubMed] |
| 5. | Coe JD, Arlet V, Donaldson W, Berven S, Hanson DS, Mudiyam R, Perra JH, Shaffrey CI. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976). 2006;31:345-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 305] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 6. | Jutte PC, Castelein RM. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J. 2002;11:594-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 200] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 7. | Li C, Wang L, Perka C, Trampuz A. Clinical application of robotic orthopedic surgery: a bibliometric study. BMC Musculoskelet Disord. 2021;22:968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 8. | Tian W. Robot-Assisted Posterior C1-2 Transarticular Screw Fixation for Atlantoaxial Instability: A Case Report. Spine (Phila Pa 1976). 2016;41 Suppl 19:B2-B5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Tian W, Wang H, Liu YJ. Robot-assisted Anterior Odontoid Screw Fixation: A Case Report. Orthop Surg. 2016;8:400-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Han X, Tian W, Liu Y, Liu B, He D, Sun Y, Han X, Fan M, Zhao J, Xu Y, Zhang Q. Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine. 2019;1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 155] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 11. | Tian W, Fan M, Zeng C, Liu Y, He D, Zhang Q. Telerobotic Spinal Surgery Based on 5G Network: The First 12 Cases. Neurospine. 2020;17:114-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 12. | Yongqi L, Dehua Z, Hongzi W, Ke Z, Rui Y, Zhou F, Shaobo W, Yi L. Minimally invasive versus conventional fixation of tracer in robot-assisted pedicle screw insertion surgery: a randomized control trial. BMC Musculoskelet Disord. 2020;21:208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Zhang Q, Xu YF, Tian W, Le XF, Liu B, Liu YJ, He D, Sun YQ, Yuan Q, Lang Z, Han XG. Comparison of Superior-Level Facet Joint Violations Between Robot-Assisted Percutaneous Pedicle Screw Placement and Conventional Open Fluoroscopic-Guided Pedicle Screw Placement. Orthop Surg. 2019;11:850-856. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | Chokshi JJ, Shah M. Outcomes of Including Fracture Level in Short- Segment Fixation for Th oracolumbar Fracture Dislocation. Asian Spine J. 2019;13:56-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Park SR, Na HY, Kim JM, Eun DC, Son EY. More than 5-Year Follow-up Results of Two-Level and Three-Level Posterior Fixations of Thoracolumbar Burst Fractures with Load-Sharing Scores of Seven and Eight Points. Clin Orthop Surg. 2016;8:71-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Liang C, Liu G, Liang G, Zheng X, Yin D, Xiao D, Zeng S, Cai H, Chang Y. Healing pattern classification for thoracolumbar burst fractures after posterior short-segment fixation. BMC Musculoskelet Disord. 2020;21:373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Wu H, Fu C, Yu W, Wang J. The options of the three different surgical approaches for the treatment of Denis type A and B thoracolumbar burst fracture. Eur J Orthop Surg Traumatol. 2014;24:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Zhang RJ, Zhou LP, Zhang L, Zhang HQ, Zhang JX, Shen CL. Safety and risk factors of TINAVI robot-assisted percutaneous pedicle screw placement in spinal surgery. J Orthop Surg Res. 2022;17:379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 19. | Du J, Gao L, Huang D, Shan L, Wang W, Fan Y, Hao D, Yan L. Radiological and Clinical Differences between Tinavi Orthopedic Robot and O-Arm Navigation System in Thoracolumbar Screw Implantation for Reconstruction of Spinal Stability. Med Sci Monit. 2020;26:e924770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Fan M, Liu Y, He D, Han X, Zhao J, Duan F, Liu B, Tian W. Improved Accuracy of Cervical Spinal Surgery With Robot-Assisted Screw Insertion: A Prospective, Randomized, Controlled Study. Spine (Phila Pa 1976). 2020;45:285-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 21. | Le X, Tian W, Shi Z, Han X, Liu Y, Liu B, He D, Yuan Q, Sun Y, Xu Y. Robot-Assisted Versus Fluoroscopy-Assisted Cortical Bone Trajectory Screw Instrumentation in Lumbar Spinal Surgery: A Matched-Cohort Comparison. World Neurosurg. 2018;120:e745-e751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 95] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hoveidaei AH, Iran; Kuroki H, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH