Published online Jul 26, 2023. doi: 10.12998/wjcc.v11.i21.5073
Peer-review started: May 31, 2023
First decision: June 14, 2023
Revised: June 28, 2023
Accepted: July 7, 2023
Article in press: July 7, 2023
Published online: July 26, 2023
Processing time: 56 Days and 22.8 Hours
During anesthesia administration for cataract surgery, low pH of proparacaine may induce pain or complications such as corneal damage and poor wound hea
To identify a method of anesthesia for geriatric cataract phacoemulsification that provides more efficient analgesia and improves clinical efficacy.
A total of 130 geriatric patients with cataracts who attended Hebei Eye Hospital from December 2020 to December 2022 were included in the present study. Patients were divided into the proparacaine surface anesthesia (SA) group (65 cases) and the compound acupuncture-medicine anesthesia group (CAMA group, 65 cases). Patients in the CAMA group were provided acupuncture analgesia in addition to SA. Preoperative anxiety [Self-Rating Anxiety Scale (SAS) score and state anxiety inventory (SAI) score], intraoperative stress, vital signs, analgesia, and cooperation, as well as postoperative adverse events, were compared between groups.
More marked reductions in anxiety were observed among patients in the CAMA group, with corresponding reductions in SAS and SAI scores. During the operation, no change in the secretion of E, NE, or Cor group compared to the preoperative period was observed in the CAMA, which was markedly lower than that in the SA group. Heart rate, blood pressure, and respiratory rate were more stable intraoperatively in the CAMA group. In addition, the incidence of intraoperative pain and the number of additional doses of anesthesia required in the CAMA group were markedly lower than in the SA group. Accordingly, patients in the CAMA group were able to avoid eye movements and eyelid closing leading to greater cooperation with surgeons during surgery. Furthermore, marked reductions in intraoperative adverse effects were observed in the CAMA group, indicating greater overall safety.
Proparacaine SA combined with acupuncture as an analgesic provides improved analgesia with greater safety compared to surface anesthesia with proparacaine during geriatric cataract phacoemulsification.
Core Tip: Innovatively use acupuncture anesthesia in traditional medicine to assist proparacaine in the anesthesia process of cataract surgery, to effectively improve the anesthetic effect, stabilize intraoperative vital signs, and reduce postoperative complications in geriatric cataract phacoemulsification.
- Citation: Dong P, Wang LF, Zhang LX, Li F, Yin HS, Dou ZX, Huang XJ, Xu R, Zhang WL. Clinical study of acupuncture combined with surface anesthesia using proparacaine in geriatric cataract phacoemulsification. World J Clin Cases 2023; 11(21): 5073-5082
- URL: https://www.wjgnet.com/2307-8960/full/v11/i21/5073.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i21.5073
As a common ophthalmological disease, cataracts are characterized by lens clouding resulting in blurred vision and reduced visual acuity, which becomes more severe with age[1]. Due to aging populations globally, the number of patients with cataracts, which negatively affects the quality of life of elderly individuals, continues to increase. Accordingly, there is a need for effective treatments in the clinical management of cataracts. With the continuous development of medical technologies, phacoemulsification has become widely used in the treatment of cataracts due to advantages of the requirement for smaller incisions, speedier recovery, and less pain[2]. As phacoemulsification is increasingly used in clinical practice, increasing attention is being paid to the effectiveness and safety of anesthesia during surgery. As patients are typically conscious during cataract surgery, effective anesthesia is an essential component of successful cataract surgery[3]. Effective anesthesia can reduce pain and improve intraoperative cooperation, which is essential for improving surgical outcomes and promoting postoperative recovery[4]. Therefore, there is an urgent clinical need for the identification of effective anesthetic methods for cataract surgery involving phacoemulsification.
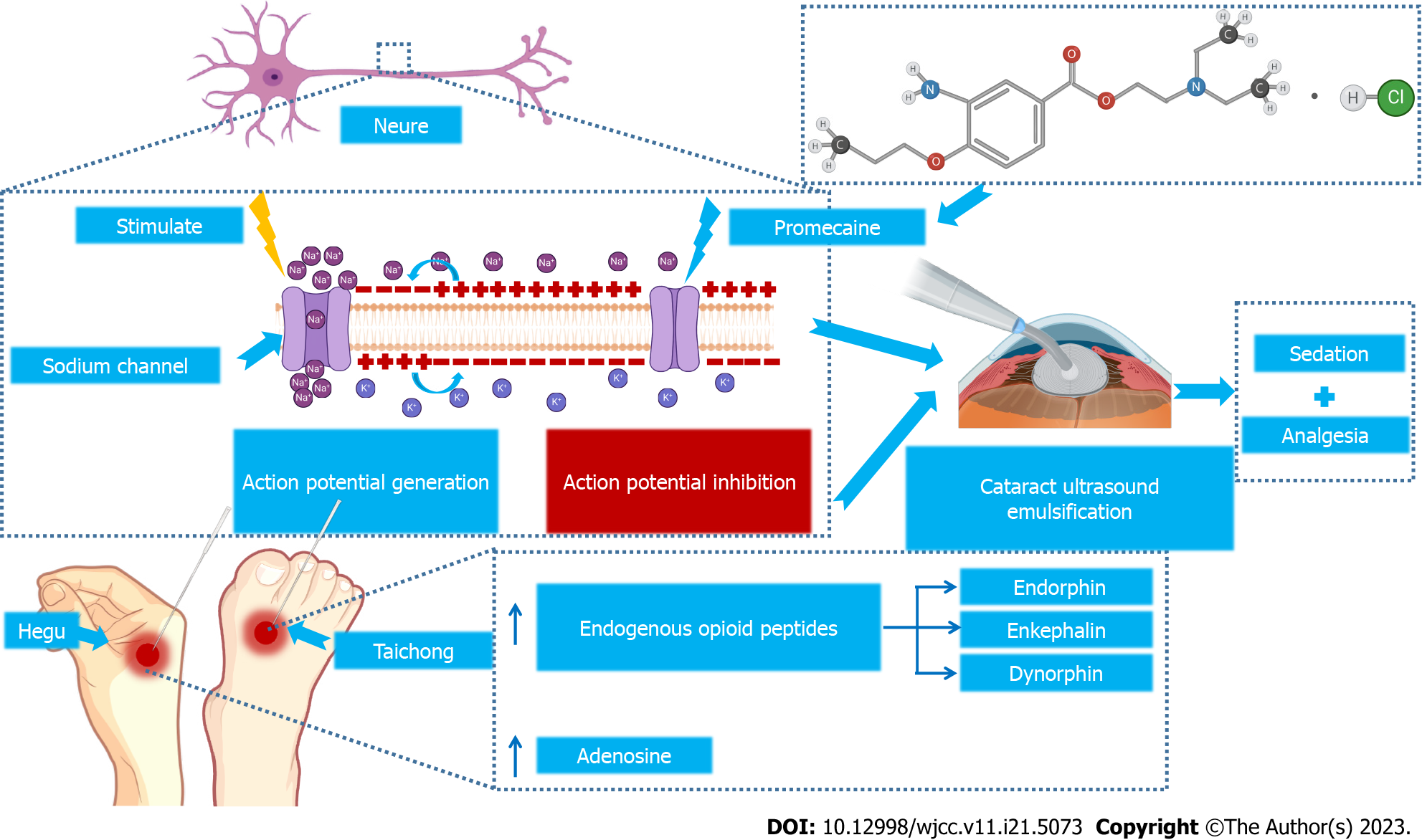
Retrobulbar anesthesia was previously the preferred method of anesthesia during cataract surgery due to its good analgesic effect associated with improved intraoperative cooperation[5]. However, retrobulbar anesthesia is an invasive procedure that is prone to complications such as ocular perforation and retrobulbar hemorrhage in addition to intraoperative transient nebulism and central depression[6,7]. Accordingly, retrobulbar anesthesia has been gradually replaced by SA, which is considered a simple and safe method of anesthesia for cataract surgery. Proparacaine is a commonly used surface anesthetic with rapid onset and sustained anesthesia, which can stabilize nerve cell membranes by reducing the instantaneous permeability of neurons to sodium, thereby achieving rapid anesthesia by preventing the generation and conduction of nerve impulses[8]. Joshi et al[9] showed that proparacaine can rapidly produce anesthesia within 20 s and effectively maintain anesthesia for 45 min. However, as the pH value of proparacaine is approximately 5, the initial drop of proparacaine applied to the ocular surface typically induces pain and anxiety[10]. In addition, the use of additional drops of intraoperatively can result in corneal damage leading to complications such as decreased visual acuity or poor wound healing which may adversely affect surgical outcomes[11].
Recently, as an example of traditional Chinese medicine, acupuncture analgesia has been increasingly used in clinical settings. Acupuncture can regulate the nervous system and promote the release of neurotransmitters by stimulating corresponding body points, thereby preventing the patient from feeling physical pain. Gioia et al[12] posited that acupuncture on Neiguan and Hegu prior to induction of anesthesia can provide effective sedation, thereby reducing patient anxiety and promoting cooperation during surgical treatments. Acupuncture can also contribute to the optimization of the physical condition of patients. Acupuncture stabilizes the blood pressure by inhibiting sympathetic excitation and stimulating parasympathetic nerves[13] which can increase the stability of intraoperative vital signs in elderly patients who are more likely to have hypertension, thereby reducing the incidence of postoperative complications. Accordingly, the use of acupuncture during surgery for s cataracts in elderly patients may represent an effective adjunct to anesthesia without inducing pain. However, few studies have examined the analgesic effects of acupuncture combined with SA with proparacaine. The present study therefore aimed to evaluate the use of CAMA in improving the anesthetic effect of proparacaine, stabilizing intraoperative vital signs, and reducing postoperative complications in elderly patients undergoing cataract phacoemulsification.
Elderly patients with cataracts who attended Hebei Eye Hospital from December 2020 to December 2022 were included as study subjects. Study inclusion criteria were as follows: visual acuity and ophthalmological condition meeting the relevant diagnostic criteria for cataracts; age 60-80 years; treated with phacoemulsification and lens implantation; no previous history of eye surgery; and no relevant ophthalmological interventions in the preceding 3 mo. Study exclusion criteria were as follows: Ocular infectious diseases such as conjunctivitis and iritis; mental disorders such as anxiety and depression; ocular motility disorders; and allergy to any of the drugs used in the study. A total of 130 patients (130 eyes) were enrolled and divided into a surface anesthesia group (SA group, 65 eyes) and a compound acupuncture-medicine anesthesia group (CAMA group, 65 eyes). The SA group received SA with proparacaine and the CAMA group received SA with proparacaine combined with acupuncture analgesia at the time of SA. Patient demographics and clinical backgrounds of both groups are shown in Table 1, with no statistically significant difference in any factor observed between the two groups (P > 0.05).
| Factors | SA group (n = 65) | CAMA group (n = 65) | χ2/t | P value |
| Sex | 0.290 | 0.590 | ||
| Male | 41 (63.08) | 38 (58.46) | ||
| Female | 24 (36.92) | 27 (41.54) | ||
| Age (yr old) | 72.84 ± 9.97 | 73.24 ± 10.14 | −0.227 | 0.821 |
| Course of disease (yr) | 2.06 ± 0.93 | 2.12 ± 1.02 | −0.350 | 0.727 |
| Pathogenic site | 0.495 | 0.482 | ||
| Left eye | 28 (43.08) | 32 (49.23) | ||
| Right eye | 37 (56.92) | 33 (50.77) | ||
| Co-morbidities | ||||
| Hypertension | 7 (10.77) | 9 (13.85) | 0.285 | 0.593 |
| Diabetes | 4 (6.15) | 3 (4.62) | 0.151 | 0.698 |
| Coronary heart disease | 8 (12.31) | 10 (15.38) | 0.258 | 0.612 |
| Family history of cataracts | 0.769 | 0.380 | ||
| No | 57 (87.69) | 60 (92.31) | ||
| Yes | 8 (12.31) | 5 (7.69) |
Preoperatively, the SA group were administered 0.5% proparacaine drops into the conjunctival sac as SA, with 1-2 drops administered every 5 min for a total of three administrations of SA.
The CAMA group were administered SA in addition to acupuncture on both sides of the Hegu and Taichong acupoints. Acupuncture needles were rapidly advanced 0.8 inch and then twisted to obtain Qi and left in place. Needles were twisted every 5 min until the end of surgery (Figure 1).
All procedures were performed by the same surgeon using the following surgical approach. After opening the eyelid, a 3-mm incision was made at the 10 o’clock position of the cornea and an auxiliary incision of approximately 1 mm in length was made in the 3 o’clock direction. Subsequently, a continuous circumferential capsular tear was created, and the nucleus was cut and emulsified using a high negative pressure and low energy phacoemulsification technique. After aspiration, the IOL was injected and adjusted to the proper position. After surgery, the incision was closed using a 10-0 suture.
Evaluation of patient sedation: The Self-Rating Anxiety Scale (SAS) scale and the state anxiety inventory (SAI) were used to assess patient tendency toward anxiety and an emotional state in hazardous emergencies, respectively. Both scales contain 20 questions, with each question evaluated using a four-point scale (1-4 points). Higher scores indicate more severe anxiety or preoperative fear in SAS and SAI, respectively.
Evaluation of patient stress: Preoperative and intraoperative venesection was performed to measure serum levels of epinephrine (E), norepinephrine (NE), and cortisol (Cor) using a fully automated biochemical analyzer as markers of sympathetic excitation.
Vital sign measurements: Heart rate (HR), mean arterial pressure (MAP), and respiratory rate (RR) were monitored before, during, and after surgery to assess clinical condition and responses to anesthesia.
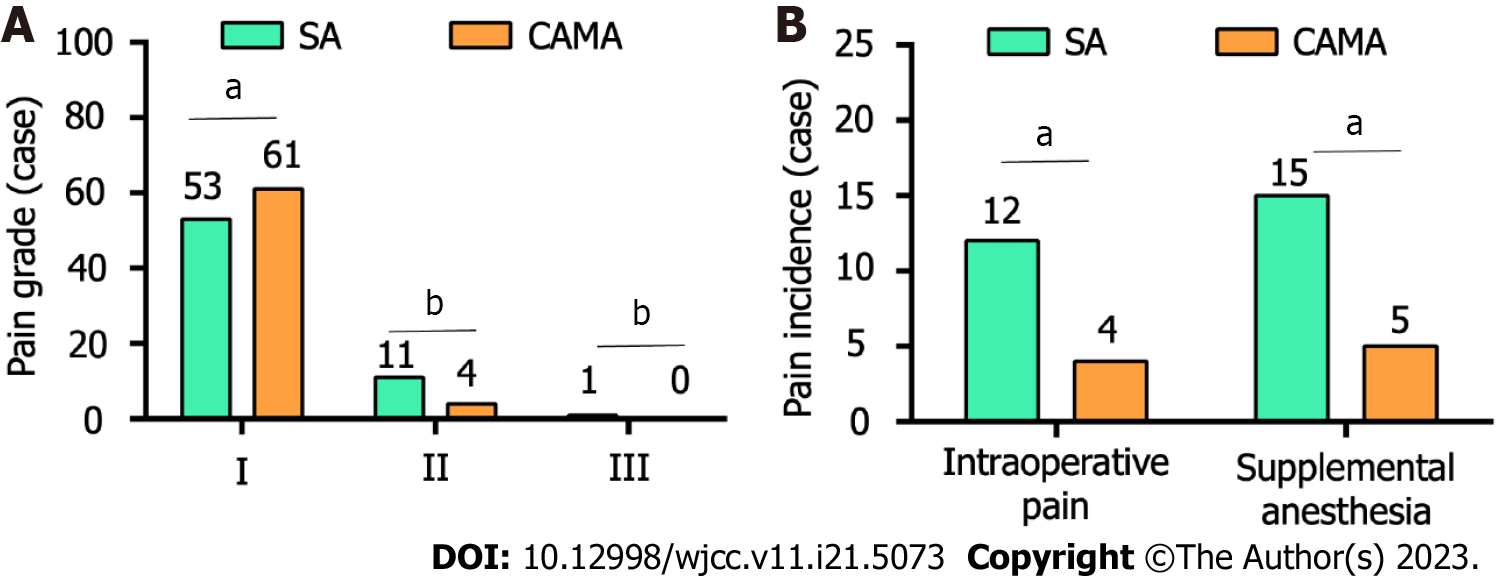
The VAS scale was used to allow patients to self-assess intraoperative pain on an 11-point scale (0-11), with higher scores indicating greater pain levels. Anesthetic effect was divided into three levels according to reported VAS scores as follows: grade I, 0 points, no intraoperative pain, good surgical cooperation; grade II, 1-4 points, minimal or moderate intraoperative pain, patient able to tolerate surgery after one or two additional administrations of anesthesia; grade III, ≥ 5 points, severe intraoperative pain, patient unable to cooperate despite two or three additional administrations of anesthesia and barely able to complete the operation. The occurrence of pain and the number of additional administrations of anesthesia required during surgery were recorded.
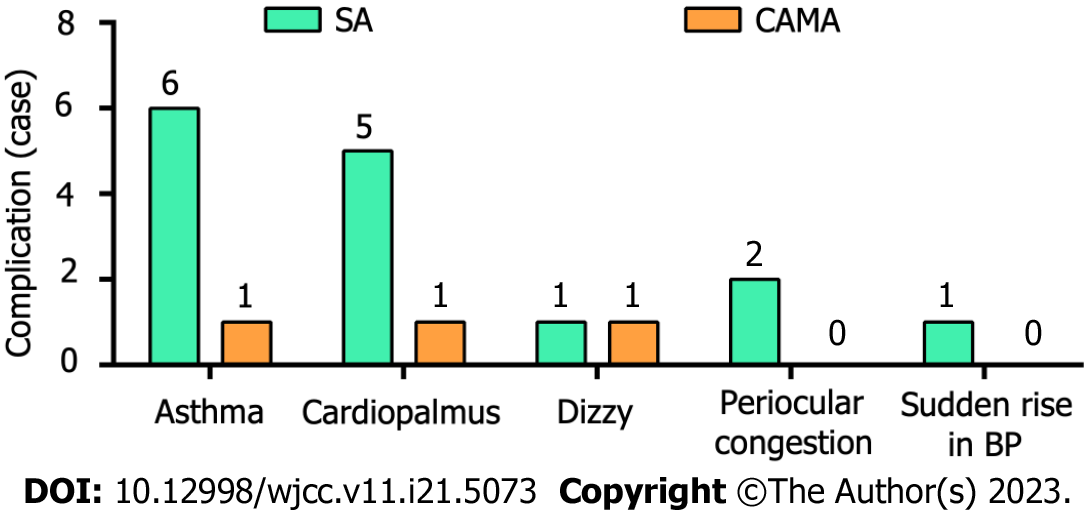
Intraoperative adverse reactions, including asthma, cardiopalmus, dizziness, periocular congestion, and sudden increases in blood pressure (BP), were recorded to evaluate the safety of the methods of anesthesia used.
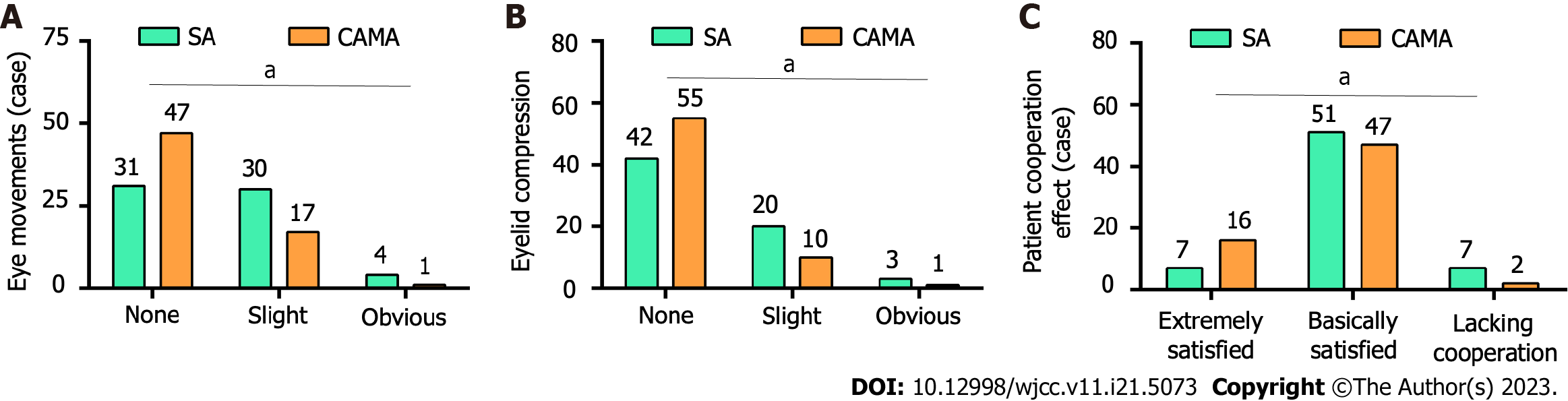
The operating surgeon assessed intraoperative eye movements and eyelid compression using a 3-point scale (0, none; 1, slight; 2, significant). The degree of intraoperative patient cooperation was classified as lacking cooperation (4 points), basic cooperation (2-3 points), and full cooperation (0-1 points).
All data were analyzed using GraphPad Prism 7. Categorical variables were expressed as n (%) and compared using the
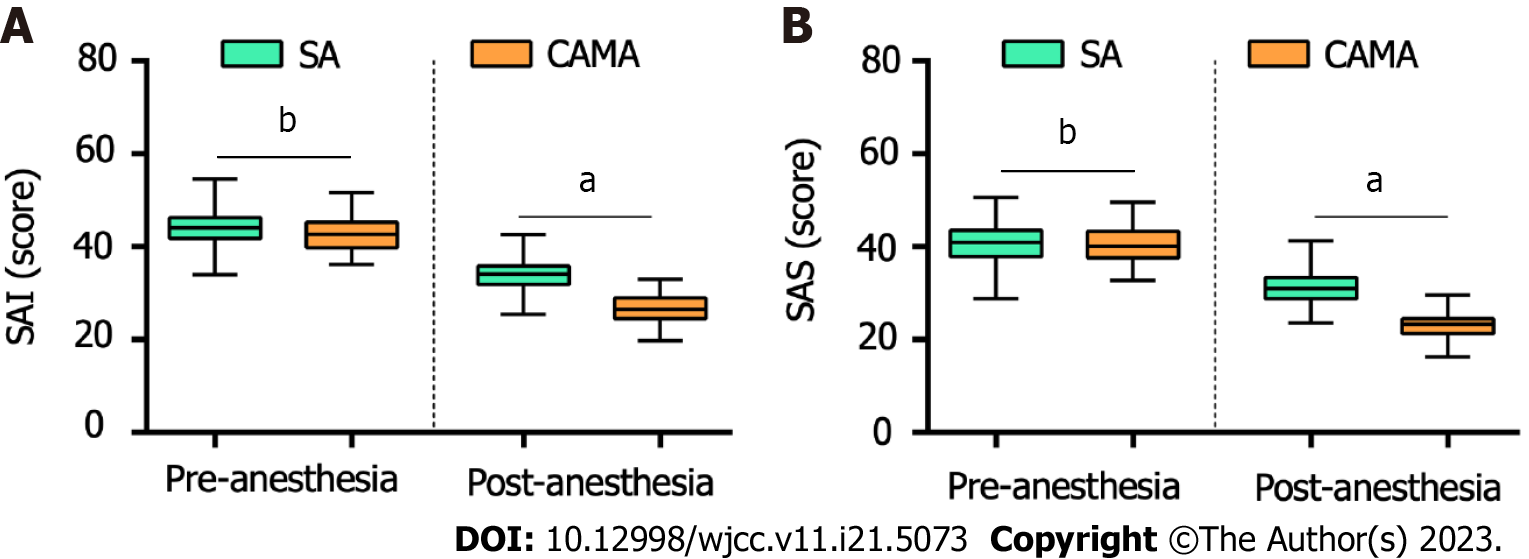
Preoperative anxiety adversely affects the technical difficulty and risk of complications of anesthesia. The results of the present study demonstrate that intraoperative anxiety was markedly reduced following the use of CAMA, with corresponding decreases in SAI and SAS scores compared to the use of SA alone (Figure 2). These results indicate that CAMA can effectively relieve preoperative anxiety and provide adequate sedation.
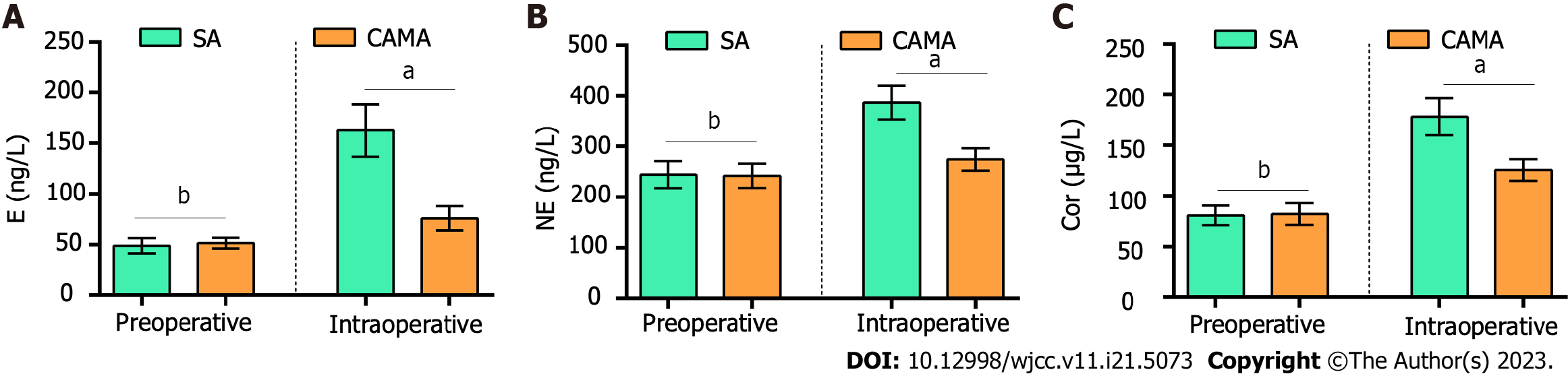
As an invasive operation, cataract surgery may cause adverse stress stimuli and interfere with the surgical process if pain is not well controlled. Intraoperative serum levels of E, NE, and Cor were markedly higher in both groups compared to preoperative levels, particularly in the SA group (Figure 3). These results indicate that CAMA provide a greater analgesic effect, prevents stressful stimulation, and suppresses sympathetic excitation during cataract surgery.
Stable intraoperative vital signs are conducive to successful surgery and improved clinical efficacy. The results of the present study demonstrate that HR, MAP, and RR were markedly increased intraoperatively in the SA group. In particular, MAP did not return to preoperative levels after the operation. However, intraoperative vital signs remained stable in the CAMA group without significant fluctuations (Figure 4). These results indicate the greater analgesic effect of CAMA and effectively maintains the stable intraoperative vital signs.
The degree of intraoperative pain in patients is an essential marker of anesthetic efficacy. In the CAMA group, a markedly higher proportion of patients in the CAMA group reported an anesthesia efficacy of grade I compared to patients in the SA group (93.85% vs 81.54%). In addition, the proportion of patients in the SA group that judged the anesthetic efficacy as grade 2 was markedly higher than in the CAMA group (16.92% vs 6.15%), with one patient in the SA group reporting an anesthetic efficacy of grade 3 (Figure 5A). Furthermore, the incidence of intraoperative pain was markedly greater in the SA group than in the CAMA group (18.46% vs 6.15%), and the number of additional administrations of anesthesia was higher in the SA group than in the CAMA group (Figure 5B). These findings indicate that CAMA provides a greater anesthetic effect and reduces the incidence of intraoperative pain.
The incidence of asthma and cardiopalmus was markedly higher in the SA group compared to the CAMA group (9.23% vs 1.54% and 7.69% vs 1.54%, respectively). In addition, there was no statistical difference in the incidence of dizziness, periocular congestion, or sudden increases in BP between the two groups (Figure 6). These findings indicate that CAMA reduces the incidence of postoperative complications, thereby improving patient satisfaction with treatment.
The results of a questionnaire provided to surgeons found that the incidence of intraoperative eye movements and eyelid exhaustion was markedly higher in the SA group than that in the CAMA group. These behaviors increase the technical difficulty of surgery and affect the surgical process (Figure 7A and B). Regarding the degree of patient cooperation during surgery, total cooperation was higher in the CAMA group than in the SA group (Figure 7C). These findings suggest that CAMA facilitates greater patient cooperation and reduces technical difficulty during cataract surgery.
To provide greater sedation and analgesia allowing for the successful completion of ultrasound emulsion surgery in elderly patients with cataracts, we innovatively combined acupuncture analgesia with the use of proparacaine as SA. The results of the present study were as we expected, with CAMA shown to effectively alleviate preoperative anxiety, reduce the occurrence of intraoperative stress, and provide greater analgesic efficacy. CAMA also had efficacy in maintaining the stability of intraoperative vital signs, improving intraoperative patient cooperation, and reducing postoperative adverse effects. Accordingly, CAMA appears to have considerable potential as an adjunct to anesthesia during phacoemulsification for cataracts in elderly patients.
As patients remain conscious during cataract surgery, preoperative anxiety can increase sensitivity to pain and affect the surgical procedure. Further, excessive anxiety may affect intraoperative patient cooperation and increase the technical difficulty of the procedure. Therefore, effective management of patient anxiety is essential. The results of the present study demonstrate that patients in the CAMA group had markedly lower SAS and SAI scores. This finding is likely attributable to the effects of acupuncture in stimulating Hegu and Neiguan points, thereby suppressing sympathetic excitation and reducing anxiety[14]. Accordingly, anesthesia supplemented with acupuncture may provide greater alleviation of patient anxiety.
We further evaluated the analgesic effect of CAMA in terms of patient stress, changes in vital signs, and pain levels during surgery. Serum levels of E, NE, and Cor did not fluctuate significantly in the CAMA group. In contrast, patients experienced significant fluctuations in serum levels of E, NE, and Cor in the SA group, particularly NE. This finding may be due to inhibition of the the sympathetic-adrenergic axis and hypothalamic-pituitary-adrenocortical axis by acupuncture on Hegu and Neiguan, which can reduce the release of E, NE, and Cor, thereby providing a sedative and analgesic effect[15,16]. These neurotransmitters are also known to increase BP, HR, and blood glucose in vivo in response to stressful stimuli[17,18]. Accordingly, large fluctuations in intraoperative vital signs were observed in the SA group, which may have negatively affected surgical outcomes and the risk of complications.
Traditional Chinese medicine posits that the production of pain in vivo is related to deficiency and stagnation of meridians, with acupuncture able to resolve blood stasis, strengthen the liver and kidney, and promote blood flow by stimulating the corresponding acupuncture points in vivo, thereby relieving pain[19,20]. According to classic books, the Hegu and Taichong points are both commonly used in traditional Chinese medicine as analgesic points, which have a more desirable effect in clearing and soothing the meridians, thereby relieving pain in the joints and the five senses[21]. Acupuncture reportedly promotes the secretion of endogenous opioid peptides and activates the endogenous nociceptive modulation system in vivo, thereby reducing the sensitivity of the central system to pain and providing an analgesic effect[22,23]. Recent studies have demonstrated that the secretion of endorphin, encephalin, and dynorphin can be increased depending on the frequency of needle stimulation to reduce the perception of pain[24,25]. In addition, recent studies have shown that acupuncture promotes the release of adenosine, a natural analgesic substance, in vivo[26]. In rat models, previous studies have reported that concentrations of adenosine in local tissues increase by 24-fold following acupuncture at points near the knee joint, and this increase in adenosine concentration was effectively maintained for more than one hour. Further, rats treated with acupuncture analgesia had a significant increase in heat-sensitive pain thresholds and heat tolerance, with an almost threefold increase in tactile heat retraction times[27]. Accordingly, the incidence of intraoperative pain of patients in the CAMA group was markedly reduced and the number of additional administrations of analgesia was also greatly reduced, which improved patients’ surgical experience and facilitated successful surgery.
Finally, our comparison of postoperative adverse reactions in both groups revealed that patients in the SA group were more prone to intraoperative complications, particularly asthma and cardiopalmus. These adverse events were likely related to poor intraoperative analgesia and patient anxiety, which led to increased susceptibility to fluctuations in HR, MAP, and RR. However, no serious adverse events, such as syncope or cardiac arrest, were observed in either group. In addition, due to the greater sedation and analgesia effect of CAMA, patients were less likely to exhibit intraoperative behaviors such as eye movements and eyelid closing, and were able to have greater cooperation with the surgeon.
The present study also has certain shortcomings. First, we did not explore the mechanism underlying the analgesic effect of acupuncture to better facilitate its application in surgical settings. In addition, the present study did not include a separate acupuncture group to allow greater evaluation of the analgesic effect of acupuncture. Third, the small sample size of the preset study may have resulted in the introduction of bias in to the study analysis. Accordingly, further studies are required to facilitate the application of CAMA in clinical settings.
In conclusion, CAMA has unique advantages in relieving preoperative anxiety, reducing intraoperative stress, and maintaining stable vital signs, which have a critical impact on improving surgical outcomes and reducing complications in elderly patients. In addition, the greater analgesic effect of CAMA can reduce undesirable intraoperative behaviors, such as eye movements and eyelid closing, as well as the requirement for additional intraoperative analgesia, thereby increasing patient cooperation during surgical procedures, improving surgical safety, and reducing adverse reactions. These findings indicate CAMA has considerable potential as an adjunct to anesthesia during cataract phacoemulsification in elderly patients.
During cataract surgery anesthesia, the low pH of proparacaine can produce some stinging and complications such as corneal damage and poor wound healing that may arise from the use of additional drops intraoperative. Therefore, an alternative adjunct to anesthesia needs to be sought to improve anesthesia and reduce the amount of intraoperative proparacaine.
Search for a new anesthesia method for cataract surgery.
To investigate a more suitable anesthesia method for geriatric cataract phacoemulsification to provide better analgesia and improve clinical efficacy.
130 geriatric cataract patients who attended Hebei Eye Hospital from December 2020 to December 2022 were included in the study and divided into the proparacaine surface anesthesia group (SA group, 65 cases) and the compound acupuncture-medicine anesthesia group (CAMA group, 65 cases), among which, patients in CAMA group were given acupuncture analgesia on the basis of SA. The preoperative anxiety (SAS score, SAI score), intraoperative stress, vital signs, analgesia, and cooperation, as well as postoperative adverse events were compared between both groups.
The results showed that the anxiety of patients in CAMA group was more markedly relieved, and their Self-Rating Anxiety Scale score and state anxiety inventory score decreased more dramatically. During the operation, the secretion of E, NE, and Cor in CAMA group showed no marked change compared to the preoperative period, which was markedly lower than that in SA group, meanwhile, their heart rate, blood pressure, and respiratory rate were maintained more stable without significant fluctuations. In addition, the incidence of intraoperative pain and the number of additional anesthesia in CAMA group were markedly lower than those in SA group, and they could effectively avoid eye movements and eyelid squeezing movements to better cooperate with the surgeon in completing the surgery. Furthermore, CAMA could markedly reduce intraoperative adverse effects and had better safety.
Proparacaine SA combined with acupuncture analgesia can provide better analgesia with guaranteed safety.
Traditional medical acupuncture anaesthesia for cataract surgery provides good sedation and analgesia, which effectively enhances the anaesthetic effect of proparacaine and reduces adverse effects, thus showing great potential in geriatric cataract phacoemulsification.
| 1. | Qureshi MH, Steel DHW. Retinal detachment following cataract phacoemulsification-a review of the literature. Eye (Lond). 2020;34:616-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 2. | Day AC, Gore DM, Bunce C, Evans JR. Laser-assisted cataract surgery versus standard ultrasound phacoemulsification cataract surgery. Cochrane Database Syst Rev. 2016;7:CD010735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Pirogova ES, Fabrikantov OL, Nikolashin SI. Femtolaser-assisted phacoemulsification of intumescent cataract. Vestn Oftalmol. 2022;138:13-22. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Masis Solano M, Lin SC. Cataract, phacoemulsification and intraocular pressure: Is the anterior segment anatomy the missing piece of the puzzle? Prog Retin Eye Res. 2018;64:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Ryu JH, Kim M, Bahk JH, Do SH, Cheong IY, Kim YC. A comparison of retrobulbar block, sub-Tenon block, and topical anesthesia during cataract surgery. Eur J Ophthalmol. 2009;19:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Nagy AA, El-Sayd SH, Ahmed AA, Rajab GZ. Optimal Dose of Dexmedetomidine Retrobulbar Anesthesia during Phacoemulsification Cataract Surgery. Anesth Essays Res. 2017;11:1046-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Kongsap P. Superior subconjunctival anesthesia versus retrobulbar anesthesia for manual small-incision cataract surgery in a residency training program: a randomized controlled trial. Clin Ophthalmol. 2012;6:1981-1986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Yang Z, Zhao J, Feng Y, Lei Y, Liu D, Qin F, Zheng J, Wang S. Identification, synthesis and structural confirmation of process-related impurities in proparacaine hydrochloride. J Pharm Biomed Anal. 2020;190:113497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Joshi RS. Proparacaine hydrochloride topical drop and intracameral 0.5% lignocaine for phacotrabeculectomy in patients with primary open angle glaucoma. Middle East Afr J Ophthalmol. 2014;21:210-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Little WB, Jean GS, Sithole F, Little E, Jean KY. Degree of corneal anaesthesia after topical application of 0.4% oxybuprocaine hydrochloride and 0.5% proparacaine hydrochloride ophthalmic solution in clinically normal cattle. Aust Vet J. 2016;94:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Joshi RS. A single drop of 0.5% proparacaine hydrochloride for uncomplicated clear corneal phacoemulsification. Middle East Afr J Ophthalmol. 2013;20:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Gioia L, Cabrini L, Gemma M, Fiori R, Fasce F, Bolognesi G, Spinelli A, Beretta L. Sedative effect of acupuncture during cataract surgery: prospective randomized double-blind study. J Cataract Refract Surg. 2006;32:1951-1954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Cheng L, Li P, Tjen-A-Looi SC, Longhurst JC. What do we understand from clinical and mechanistic studies on acupuncture treatment for hypertension? Chin Med. 2015;10:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Liu Y, Park JE, Shin KM, Lee M, Jung HJ, Kim AR, Jung SY, Yoo HR, Sang KO, Choi SM. Acupuncture lowers blood pressure in mild hypertension patients: a randomized, controlled, assessor-blinded pilot trial. Complement Ther Med. 2015;23:658-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Li DZ, Zhou Y, Yang YN, Ma YT, Li XM, Yu J, Zhao Y, Zhai H, Lao L. Acupuncture for essential hypertension: a meta-analysis of randomized sham-controlled clinical trials. Evid Based Complement Alternat Med. 2014;2014:279478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 16. | Ma W, Zhu YM, Zhou H, Fu GQ, Pan H, Shen WD. Protecting action of acupuncture-drug compound anesthesia with different frequency electroacupuncture on stress reaction in pneumonectomy. Zhongguo Zhen Jiu. 2011;31:1020-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Zheng Y, Zhang J, Wang Y, Lan Y, Qu S, Tang C, Huang Y. Acupuncture Decreases Blood Pressure Related to Hypothalamus Functional Connectivity with Frontal Lobe, Cerebellum, and Insula: A Study of Instantaneous and Short-Term Acupuncture Treatment in Essential Hypertension. Evid Based Complement Alternat Med. 2016;2016:6908710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Zhiyuan W, Ming Y, Jie J, Yi W, Tiansheng H, Mingfen L, Zhijie H, Zhenzhen G, Pang LM. Effect of transcutaneous electrical nerve stimulation at acupoints on patients with type 2 diabetes mellitus: a randomized controlled trial. J Tradit Chin Med. 2015;35:134-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Ji S, Zhang H, Qin W, Liu M, Zheng W, Han Y, Song H, Li K, Lu J, Wang Z. Effect of Acupuncture Stimulation of Hegu (LI4) and Taichong (LR3) on the Resting-State Networks in Alzheimer's Disease: Beyond the Default Mode Network. Neural Plast. 2021;2021:8876873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Liang P, Wang Z, Qian T, Li K. Acupuncture stimulation of Taichong (Liv3) and Hegu (LI4) modulates the default mode network activity in Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2014;29:739-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 21. | Jiang MC, Liang J, Zhang YJ, Wang JR, Hao JD, Wang MK, Xu J. Effects of Acupuncture Stimulation of Bilateral "Hegu" (LI 4) and "Taichong" (LR 3) on Learning-memory Ability, Hippocampal AP 42 Expression and Inflammatory Cytokines in Rats with Alzheimer's Disease. Zhen Ci Yan Jiu. 2016;41:113-118. [PubMed] |
| 22. | Lin JG, Chen WL. Acupuncture analgesia: a review of its mechanisms of actions. Am J Chin Med. 2008;36:635-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 234] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 23. | Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008;85:355-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 665] [Cited by in RCA: 778] [Article Influence: 43.2] [Reference Citation Analysis (1)] |
| 24. | Meng X, Zhang Y, Li A, Xin J, Lao L, Ren K, Berman BM, Tan M, Zhang RX. The effects of opioid receptor antagonists on electroacupuncture-produced anti-allodynia/hyperalgesia in rats with paclitaxel-evoked peripheral neuropathy. Brain Res. 2011;1414:58-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 25. | Shimoyama M, Toyama S, Tagaito Y, Shimoyama N. Endogenous endomorphin-2 contributes to spinal ĸ-opioid antinociception. Pharmacology. 2012;89:145-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Goldman N, Chen M, Fujita T, Xu Q, Peng W, Liu W, Jensen TK, Pei Y, Wang F, Han X, Chen JF, Schnermann J, Takano T, Bekar L, Tieu K, Nedergaard M. Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat Neurosci. 2010;13:883-888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 659] [Cited by in RCA: 593] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 27. | Yi M, Zhang H, Lao L, Xing GG, Wan Y. Anterior cingulate cortex is crucial for contra- but not ipsi-lateral electro-acupuncture in the formalin-induced inflammatory pain model of rats. Mol Pain. 2011;7:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Garcia-Ibanez P, Spain; Lee D, United States S-Editor: Liu JH L-Editor: A P-Editor: Zhang XD