Published online Jul 16, 2023. doi: 10.12998/wjcc.v11.i20.4961
Peer-review started: April 30, 2023
First decision: May 25, 2023
Revised: June 2, 2023
Accepted: June 26, 2023
Article in press: June 26, 2023
Published online: July 16, 2023
Processing time: 72 Days and 19.5 Hours
Anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis is a rare autoimmune disorder. The symptoms of anti-NMDAR encephalitis include behavioral problems, speech problems, psychosis, seizures, and memory deficits, among others. However, laryngospasm is rare. We present the case of a patient with anti-NMDAR antibodies and severe laryngospasms.
The patient was a 15-year-old female with normal psychomotor development. She was initially admitted to our neurological intensive care unit with seizures. She received anti-epilepsy treatment, and the seizures disappeared. However, 2 wk later, she developed behavioral problems and speech impairment. Then, she developed severe laryngospasms, which were treated with intubation and a tracheotomy. Antibodies against the NMDAR were detected in the patient’s cerebrospinal fluid. Therefore, she was diagnosed with anti-NMDAR encephalitis. In addition, she received intravenously administered immunoglobulins, and methylprednisolone was administered. The patient’s symptoms gradually improved, and she was discharged from our hospital. Approximately 9 mo later, the patient could speak sentences, walk independently, and carry out activities of daily living independently. Through our case report, we highlighted laryn
Laryngospasm may be an uncommon clinical manifestation of anti-NMDAR encephalitis.
Core Tip: Laryngospasms are uncommonly reported in anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis. Herein, we report a rare case of a patient with anti-NMDAR encephalitis with severe laryngospasms. The patient was treated with intubation and tracheotomy. In addition, she received intravenously administered immunoglobulins, and methylprednisolone was administered. Nine months later, the patient could perform activities of daily living independently. We highlighted that patients with anti-NMDAR encephalitis may present with fatal laryngospasms. Further study of fatal laryngospasms secondary to anti-NMDAR encephalitis may be necessary in the future.
- Citation: Wang L, Su HJ, Song GJ. Laryngospasm as an uncommon presentation in a patient with anti-N-methyl-D-aspartate receptor encephalitis: A case report. World J Clin Cases 2023; 11(20): 4961-4965
- URL: https://www.wjgnet.com/2307-8960/full/v11/i20/4961.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i20.4961
Anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis is an autoimmune disorder that is mediated by anti-NMDAR antibodies. Anti-NMDAR encephalitis is characterized by behavioral problems, speech problems, psychosis, seizures, memory deficits, dyskinesias, and autonomic and breathing dysregulation[1], with laryngospasm being uncommon. Anti-NMDAR encephalitis was first reported in 2007[2], and it predominantly affects young females with ovarian teratomas[3]. NMDAR is activated by glutamate and is expressed in the hippocampus and the forebrain. NMDAR plays a role in learning, memory, judgment, reality perception, and autonomic functions[4]. Intravenous pulse methylprednisolone and immunoglobulins are first-line treatments. Some patients require artificial ventilation in the intensive care unit. Early diagnosis and timely immunotherapy are important for treating this disorder.
Here, we reported the case of a 15-year-old female patient with anti-NMDAR encephalitis and severe laryngospasms. We intend to raise awareness that patients with anti-NMDAR encephalitis may present with fatal laryngospasms.
A 15-year-old female presented with 3 d of seizures.
Three days prior, the patient had two episodes of tonic clonic seizures, with a loss of consciousness followed by falling and tonic muscle spasms, a gray face, and jerky movements of the arms and legs, which gradually disappeared after 2-3 min.
The patient had no history of epilepsy or psychosis.
Both parents were healthy.
The patient’s body temperature was 36.5 °C, and her blood pressure was 116/80 mmHg. The findings of brain magnetic resonance imaging (MRI) and computed tomography (CT) were all initially normal. Electroencephalography (EEG) showed diffuse slow waves on basic activity. Our hypothesis was initially epilepsy, and we started treatment with levetiracetam (17 mg/kg/day), after which the seizures disappeared. Two weeks later, she started to experience behavioral problems and speech impairment, fearfulness, and auditory/visual hallucinations with an intermittent course during the day. On physical examination, the patient remained unresponsive to external stimuli. Then, she developed laryn
All listed blood investigation results were within normal ranges. For example, her white blood cell count was within the normal range at 7.2 × 109/L (normal range: 3.5-9.5 × 109/L), glucose was 5.8 mmol/L (normal range: 3.9-6.1 mmol/L), her triglyceride level was 0.90 mmol/L (normal range: 0.00-2.26 mmol/L), gamma glutamyl transpeptidase was 37 U/L (normal range: 10-60 U/L), thyrotropin was 1.36 mIU/L (normal range: 0.55-4.78 mIU/L), and creatine phosphokinase was 51 U/L (normal level: 0-171 U/L). Lumbar puncture examination of the cerebrospinal fluid (CSF) revealed a pressure of 200 mmH2O (normal range: 80-180 mmH2O). CSF analysis revealed the following: 12 nucleated cells/mL (normal level: 0-5 nucleated cells/mL); glucose 3.8 mmol/L (normal range: 2.5-4.5 mmol/L); protein 0.38 g/L (normal range: 0.15-0.45 g/L); and chloride 116.7 mmol/L (normal range: 116.0-130.0 mmol/L). NMDAR antibodies were detected in the CSF.
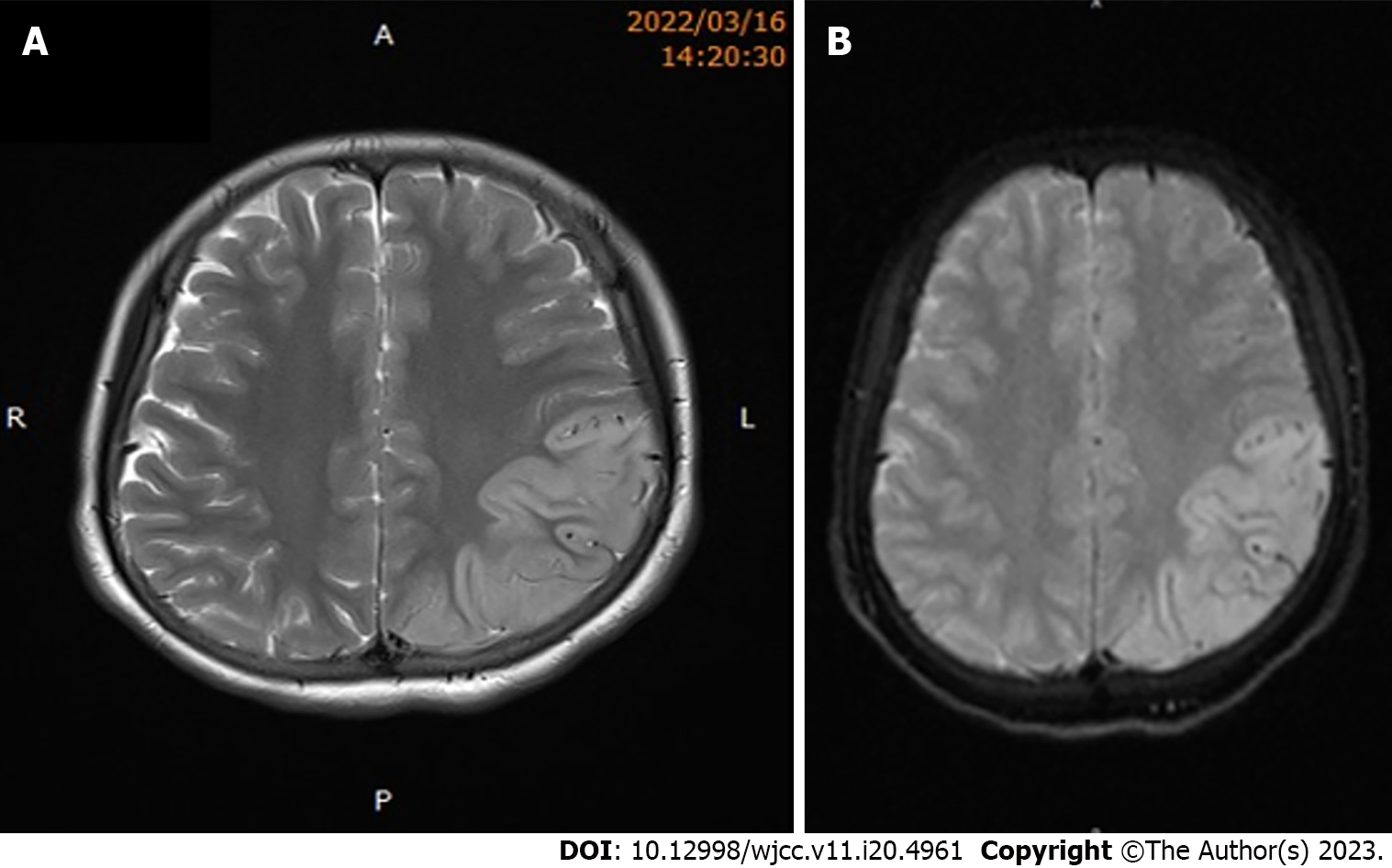
The findings of brain MRI and CT were all initially normal. However, upon re-examination 2 wk later, a cranial MRI revealed abnormally high signals in the left frontotemporal parietal occipital cortex and subcortical area on T2-weighted images and fluid-attenuated inversion recovery images (Figure 1). A 4-h video electroencephalogram showed nonspecific slow activity without epileptic discharge. Chest CT, pelvic and abdominal color ultrasound, and MRI did not reveal any tumors, including teratomas.
The patient was diagnosed with anti-NMDAR encephalitis.
The patient received glucocorticoids and human immunoglobulin (IVIG) treatments. She was started on a 3-d course of intravenous methylprednisolone (30 mg/kg/day), followed by oral administration of prednisone (2 mg/kg/day, weaned over 3 mo) and intravenous IVIG 400 mg/kg/day for 5 d. Four weeks later, the frequency of laryngospasm gradually decreased, and the clinical symptoms gradually decreased. The patient’s psychiatric and neurological symptoms were resolved. The patient was transferred to the rehabilitation unit after 3 mo.
Presently, the patient has been under follow-up for 9 mo. She is now able to speak in sentences, walk independently, and perform activities of daily living independently. She has had no seizures or abnormal body movements.
Anti-NMDAR encephalitis is an autoimmune neuropsychiatric disorder[2]. Encephalitis is associated with the production of autoantibodies directed toward NMDAR, a protein involved in synaptic plasticity and memory function. The clinical manifestations of anti-NMDAR encephalitis are complex and vary in severity. Most patients present with prodromal symptoms, including fever, nausea, headache, and diarrhea. Within 2 wk, patients usually develop a multistage illness that progresses from psychosis, seizures, speech impairment, and memory deficits to a state of unresponsiveness with catatonic features often associated with autonomic and breathing instability[5]. Approximately 60% of cases with anti-NMDAR encephalitis have tumors, and teratomas are the most commonly associated tumors[6].
No prodromal symptoms or tumors were found during the clinical diagnosis or treatment of the patient. This patient showed epilepsy onset but exhibited severe laryngospasms, which represent an uncommon symptom of anti-NMDAR encephalitis and a difficult problem during treatment. Laryngospasm may result from the spread of tonic discharges into the cortex (lateral motor nucleus and anterior insula) that controls laryngeal movement or a marked increase in vagal tone[7]. It has been speculated that laryngospasm in patients with anti-NMDAR encephalitis may be related to epileptic activity[8]. We speculate that the pathogenesis of anti-NMDAR encephalitis-related laryngospasm may be similar to the abovementioned mechanism, but more studies are needed to confirm this.
It has been reported that EEG findings either at the onset or during the course of the disorder are abnormal in more than 90% of patients[9]. The sensitivity of cranial MRI is lower, being positive in less than 55% of patients[5]. EEG showed diffuse slow waves of basic activity in our patient. Her early cranial MRI findings were nonspecific. As the disorder progresses, T2-weighted images and fluid-attenuated inversion recovery can reveal abnormal signals in the left frontotemporal parietal occipital cortex and subcortical areas.
The first-line treatment drugs are high and early doses of glucocorticoids and IVIG[10]. If first-line treatment is ineffective, second-line treatment (cyclophosphamide or rituximab) is often effective. With immunotherapy and in cases of neoplastic tumor removal, this disorder is reversible. Early initiation of treatment is associated with a more favorable clinical outcome. Bortezomib treatment showed disease remission or clinical improvement in patients with resistance or delayed treatment response to standard immunosuppressive and B-cell-depleting drugs (corticosteroids, IVIG, immunoadsorption, plasma exchange, rituximab, cyclophosphamide)[11]. With proper treatment, most patients can slowly obtain a full or a nearly full recovery. However, recovery may take 2 years or longer, and not all patients can return to former levels of motor and cognition function. In the present study, the patient was treated with glucocorticoids and IVIG. She could independently perform activities of daily living several months later.
Laryngospasm may be an uncommon clinical manifestation of anti-NMDAR encephalitis, and it can be suggestive of a critical illness and the possibility of sudden death. Early identification and early aggressive treatment can affect the prognosis of the disorder.
We would like to express our appreciation to editors and reviewers for suggesting how to improve our paper.
| 1. | Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7:1091-1098. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2443] [Cited by in RCA: 2228] [Article Influence: 123.8] [Reference Citation Analysis (0)] |
| 2. | Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi JE, Voloschin A, Baehring JM, Shimazaki H, Koide R, King D, Mason W, Sansing LH, Dichter MA, Rosenfeld MR, Lynch DR. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61:25-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2002] [Cited by in RCA: 1782] [Article Influence: 93.8] [Reference Citation Analysis (0)] |
| 3. | Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, Cortese I, Dale RC, Gelfand JM, Geschwind M, Glaser CA, Honnorat J, Höftberger R, Iizuka T, Irani SR, Lancaster E, Leypoldt F, Prüss H, Rae-Grant A, Reindl M, Rosenfeld MR, Rostásy K, Saiz A, Venkatesan A, Vincent A, Wandinger KP, Waters P, Dalmau J. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15:391-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2328] [Cited by in RCA: 2896] [Article Influence: 289.6] [Reference Citation Analysis (0)] |
| 4. | Lazar-Molnar E, Tebo AE. Autoimmune NMDA receptor encephalitis. Clin Chim Acta. 2015;438:90-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10:63-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1879] [Cited by in RCA: 1692] [Article Influence: 112.8] [Reference Citation Analysis (0)] |
| 6. | Barry H, Byrne S, Barrett E, Murphy KC, Cotter DR. Anti-N-methyl-d-aspartate receptor encephalitis: review of clinical presentation, diagnosis and treatment. BJPsych Bull. 2015;39:19-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 114] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 7. | Subramani K. Laryngospasm during subarachnoid block. Br J Anaesth. 2006;96:141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 8. | Liu LJ, Wang YT. [Ictal Iaryngospasm as a main feature in a patient with anti-NMDA receptor encephalitis]. Zhongguo Zonghe Linchuang. 2021;37:566-568. [DOI] [Full Text] |
| 9. | Gitiaux C, Simonnet H, Eisermann M, Leunen D, Dulac O, Nabbout R, Chevignard M, Honnorat J, Gataullina S, Musset L, Scalais E, Gauthier A, Hully M, Boddaert N, Kuchenbuch M, Desguerre I, Kaminska A. Early electro-clinical features may contribute to diagnosis of the anti-NMDA receptor encephalitis in children. Clin Neurophysiol. 2013;124:2354-2361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Lebas A, Husson B, Didelot A, Honnorat J, Tardieu M. Expanding spectrum of encephalitis with NMDA receptor antibodies in young children. J Child Neurol. 2010;25:742-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Scheibe F, Prüss H, Mengel AM, Kohler S, Nümann A, Köhnlein M, Ruprecht K, Alexander T, Hiepe F, Meisel A. Bortezomib for treatment of therapy-refractory anti-NMDA receptor encephalitis. Neurology. 2017;88:366-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 142] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Paparoupa M, Germany; Rudat V, Saudi Arabia S-Editor: Qu XL L-Editor: Filipodia P-Editor: Yu HG