Published online Jul 16, 2023. doi: 10.12998/wjcc.v11.i20.4814
Peer-review started: May 11, 2023
First decision: May 31, 2023
Revised: June 7, 2023
Accepted: June 25, 2023
Article in press: June 25, 2023
Published online: July 16, 2023
Processing time: 62 Days and 1 Hours
The femoral neck dynamic intersection system (FNS) is mechanically more stable than other internal fixation techniques. Current studies have confirmed that the structural design of FNS has good biomechanical properties in European and American populations. However, whether the suitability of the FNS's 130° main nail angle design for Asian populations has been thoroughly investigated remains unclear.
To compare the biomechanical stability differences among different main nail angles of the FNS in the treatment of femoral neck fractures in Asian populations.
Computed tomography data of the femur of healthy adult male volunteers were imported into Mimics software to create a three-dimensional model of the femur. The model was adapted to the curve using Geomagic software and imported into Solidworks software to construct the Pauwels I femoral neck fracture model and design the FNS internal fixation model using different main nail angles. Afterward, the models were assembled with the FNS fracture model and meshed using the preprocessing Hypermesh software. Subsequently, they were imported into Abaqus software to analyze and evaluate the biomechanical effects of different angles of the FNS main nail on the treatment of femoral neck fractures.
The peak displacement of the proximal femur under different angles of FNS fixation under stress was 7.446 millimeters in the 120° group and 7.416 millimeters in the 125° group; in the 130°, 135°, and 140° FNS fixation groups, the peak displacement was 7.324 millimeters, 8.138 millimeters, and 8.246 millimeters, respectively. In the 120° and 125° FNS fixation groups, the maximum stresses were concentrated at the main nail and the anti-rotation screw, which intersected the fracture line of the femur neck, resulting in peak stresses of 200.7 MPa and 138.8 MPa, respectively. Peak stresses of 208.8 MPa, 219.8 MPa, and 239.3 MPa were observed on the angular locking plate distal to the locking screw in the 130°, 135°, and 140° fixation groups.
FNS has significant stress distribution properties, a minimal proximal femoral displacement, and an optimal stability for treating femoral neck fractures in Asian populations when performed with a 130° main nail angle.
Core Tip: Current studies have confirmed that the structural design of the femoral neck dynamic intersection system (FNS) has good biomechanical properties in European and American populations. However, no relevant research report currently addresses the suitability of the 130° staple design of FNS for Asian populations. Herein, we compared the biomechanical stability differences in various FNS main nail angles for treating femoral neck fractures in Asian populations. We found that, in Asian populations, a main nail FNS angle of 130° has the best stability for treating femoral neck fractures with quantifiable stress distribution and minimal proximal femoral displacement.
- Citation: Wang Y, Ma JX, Bai HH, Lu B, Sun L, Jin HZ, Ma XL. Mechanical analysis of the femoral neck dynamic intersection system with different nail angles and clinical applications. World J Clin Cases 2023; 11(20): 4814-4823
- URL: https://www.wjgnet.com/2307-8960/full/v11/i20/4814.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i20.4814
Femoral neck fractures are among the most common fractures in the lower extremities, accounting for approximately 3.61% of all total body fractures[1]. Several studies have indicated that the number of hip fractures is expected to increase to 2.6 million worldwide by 2025 and to 4.5 million by 2050[2-4], of which 53.27% will be femoral neck fractures[4]. Due to the high incidence of disability and death after surgery, femoral neck fractures exert a significant socioeconomic burden and endanger patient health[5]. Moreover, adolescents are significantly more likely than middle-aged or elderly individuals to suffer from femoral head necrosis following a femoral neck fracture. Notably, femoral neck fractures and complications among adolescents have increased due to the high rate of motor vehicle accidents.
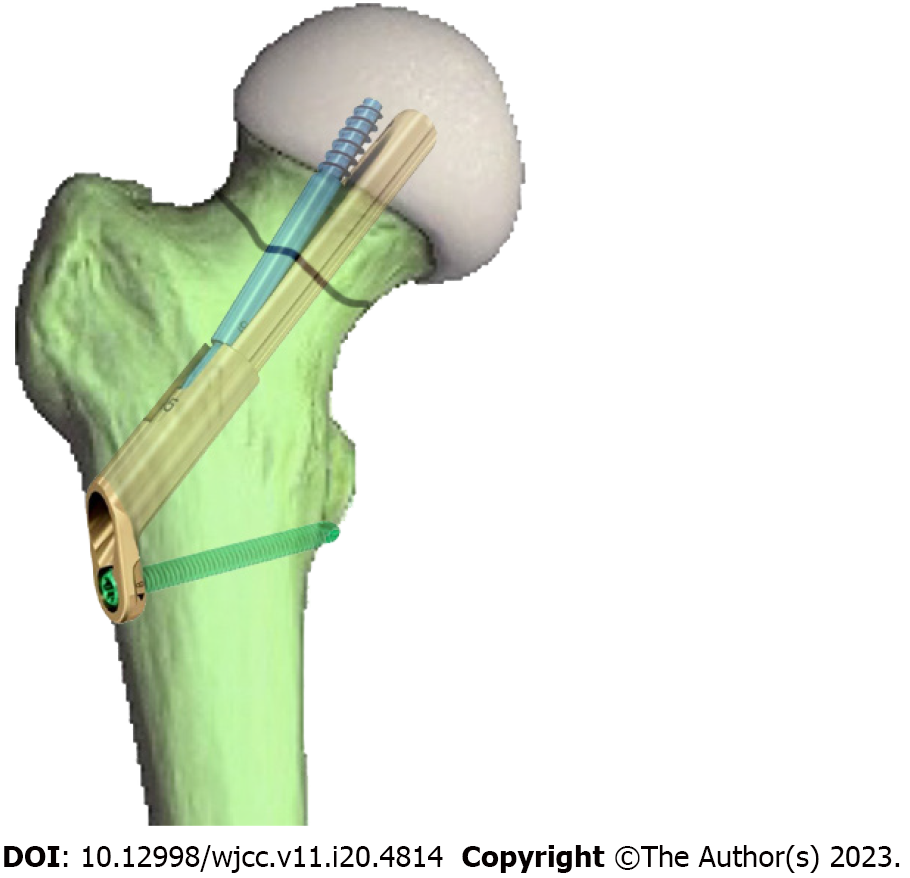
The femoral neck dynamic intersection system (FNS) is a new type of internal fixation system for treating femoral neck fracture with multiple advantages, including minimal invasiveness and good preservation of bone volume and angular stability[6-8]. Furthermore, this method has the advantages of requiring a shorter time for fracture healing, a low rate of complications, and an early return to normal daily activities following surgery[9-11]. Several mechanical stability tests have also shown that FNS is more mechanically stable than other internal fixations in treating femoral neck fractures[12,13]. FNS comprises a lateral locking plate, main nail, anti-rotation screw, and locking nail (Figure 1). The locking plate is connected to the main nail at an angle of 130°, and the main nail forms an angle of 7.5° with the anti-spinning screw, which provides rotational stability[14].
Current studies have confirmed that this structure design has good biomechanical properties in European and American populations[15]. However, considering the differences in the anatomical morphology of proximal femoris among different ethnic groups[16], we proposed a hypothesis regarding the suitability of the 130° staple design of FNS for Asian populations. To our knowledge, no relevant research has been published on this specific topic.
Experimental and clinical testing in assessing the mechanical stability of internal fixation of femoral neck fractures requires higher costs, sophisticated equipment, and longer timeframes. To avoid the obstacles experimental and clinical studies face, computational simulations based on the finite element method can be a strategic option[17]. This approach can also be the basis for initial research on developing an FNS with various parameters to assess the costs and energy wasted on trial-and-error efforts before continuing with experimental and clinical testing in further research[18]. Notably, computational simulation is key in predicting pressure conduction and displacement changes with various parameters studied in FNS application testing. Therefore, the main purpose of the present study is to investigate the advantages of the main nail angle design of the FNS lateral locking plate by comparing the biomechanical stability differences in various FNS main nail angles for treating femoral neck fractures in Asian populations.
An adult male volunteer with a height of 178 cm and a weight of 73 kg provided consent for his images to be used in image analysis. After clinical examination, the volunteer had no symptoms of hip joint diseases, injuries or ligament instability. Spiral computed tomography (CT) scans (64-row spiral CT brand GE, layer thickness 0.625 mm, voltage 120 kV, current 150 mA) were performed on both hips, and the scanned data were saved in DICOM format.
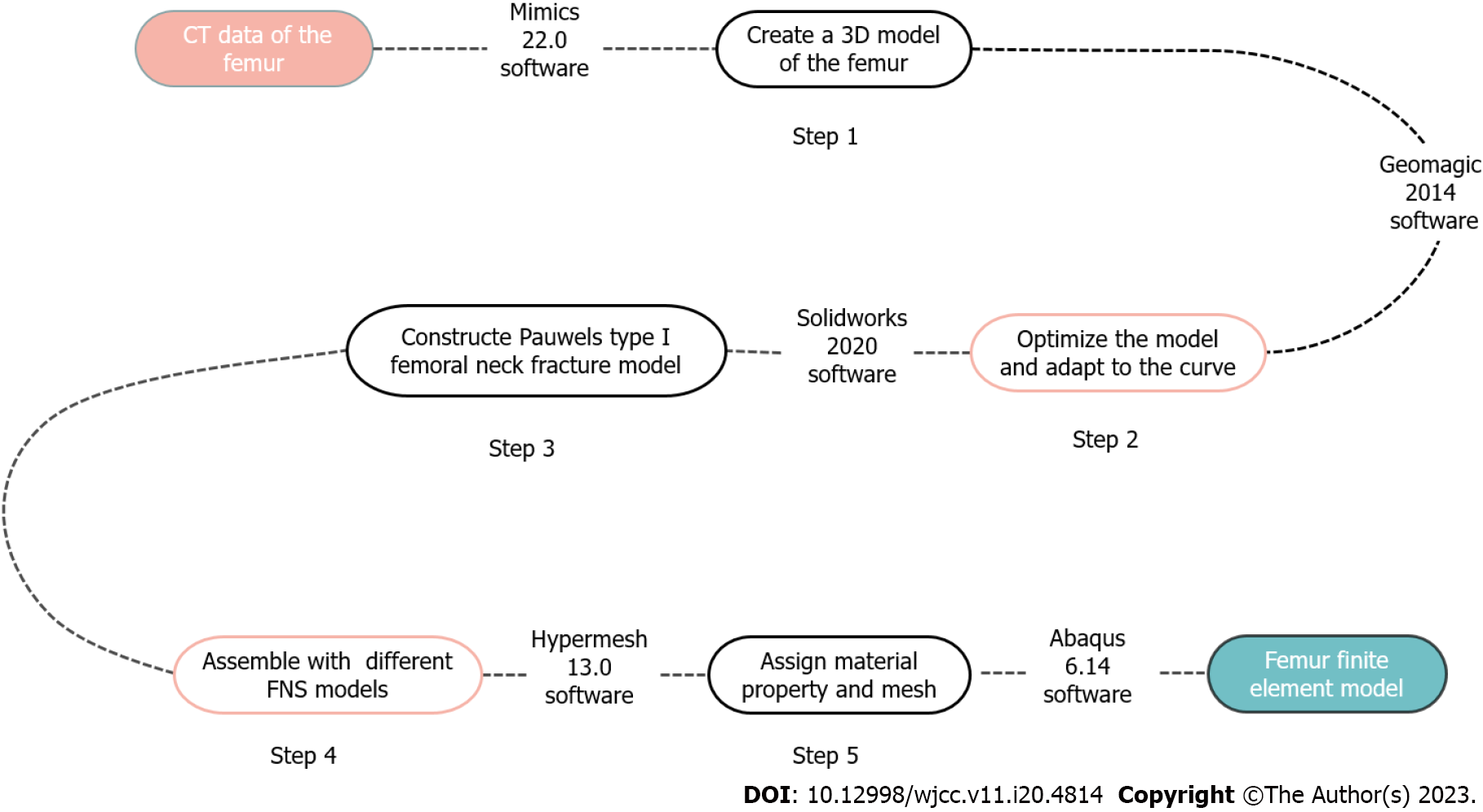
The finite element model of FNS fixation of femoral neck fracture was established using a CT image of the femur, and the flow is shown in Figure 2.
Data from the right femur of the hip joint were used as the experimental sample. Using the DICOM format data, the right femur's three-dimensional (3D) model was created with gray-scale threshold segmentation using Mimics 22.0 software (Materialise NV, Belgium) and exported as binary STL files. The femur model was subsequently imported into Geomagic 2014 software (Geomagic Inc., United States) for optimization by removing nails, starting movement, loosening, and smoothing. The surface processing stage was then initiated; this involved measuring the curvature of the femur surface, editing and adjusting constraint lines, building grids, and finally generating a NURBS surface, fitting it, and exporting it in an IGES format. Using Solidworks 2020 (SolidWorks Co., United States) software, the IGES format femur model was imported to simulate a Pauwels type I femoral neck fracture.
Using SolidWorks software (Figure 3), the FNS model was drawn with angles of 120°, 125°, 130°, 135°, and 140°, respectively, for the lateral locking steel plate and the main nail. The diameter of the main nail was 10 mm, the diameter of the anti-rotation screw was 6.4 mm, and the angle of the main nail was maintained at 7.5° (Figure 3B). A 5.0 mm diameter locking screw was placed distal to the lateral locking steel plate.
As shown in Figure 4, the FNS models with different main nail angles were assembled separately from the femoral neck fracture model to determine the relative fixation positions. Both were then imported into Hypermesh 13.0 software (Altair Engineering Inc., United States) in the IGES format for material property assignment. Femoral model material properties were assigned uniformly, and the internal fixation and femur were then meshed to generate the femoral finite element model with different internal fixation methods. Finally, Finite Element Analysis (FEA) Abaqus 6.14 software (Dassault Simulia, Inc., United States) was applied to analyze the mechanical loading.
A free mesh using tetrahedral 10-node elements was computed for each model using the Hypermesh mesher. These elements' second-order shape functions ensured a mesh close enough to the bone’s boundary surfaces. Hexahedral elements are known to be more accurate than tetrahedral ones, but the complexity of our model did not enable us to use them[19]. Therefore, the individual parts of the broken femur and fixation implants were created using volume second-order tetrahedral C3D10 elements. The results were converged to the parameter of interest, i.e., the axial femoral head displacement, with about 15000 and 81000 elements depending on the fixation methods.
In all models, the bone tissue was assumed to be homogeneous, isotropic, and elastic[20]. Even though it is well known that bone is an anisotropic and non-homogeneous material, since the focus of this study is to compare the mechanical stability of fractures treated with different FNS, the choice of isotropic material properties for the bone is acceptable for modeling the human femoral bone. The elastic moduli of the bone were chosen to be 7.3 GPa[21], and a Poisson’s ratio of 0.3 was assumed[22]. The FNS implants were made of titanium alloy, and the properties were based on previous studies[23]. The properties of these materials are shown in Table 1.
| Materials | Modulus of elasticity (GPa) | Poisson's ratio |
| Bone | 7.3 | 0.3 |
| FNS | 110 | 0.3 |
Fractures of the femur were represented as complete fractures with bone surface contact, and according to Samsami et al[20], the friction coefficient between bone and bone can be assumed to be 0.3. The distal femur was defined as being completely fixed in the X, Y, and Z axes. It was assumed that the internal fixation screws would be firmly fixed to the femoral joint surface and that there would be no interface loosening. During static loading stress, a stress load of 1400 N was applied to the joint surface of the upper femur, with the load exerted vertically downward in the axial direction, to determine the stress distribution between the femur and the internal fixation.
FEA revealed the following indexes: (1) The displacement of the proximal femur in each group and its impact on the healing process; (2) the Von Mises stress distribution of the internal fixation and the femur in the five groups of models and the maximum Von Mises stress, to evaluate the stress distribution, and to assess whether the improvement of stress distribution under the same conditions correlates with the improvement of fracture rehabilitation.
All simulation analyses were conducted by two independent researchers at different time periods. The intraclass correlation coefficients (ICCs) were used to assess the inter-observer reliability (Supplementary Table 1).
The ICCs were greater than 0.75, indicating high consistency and reliability in the analysis results.
The magnitude of the stress force causing displacement of the proximal femur can provide a direct indication of the mechanical stability of the internal fixation. In different stress angles of FNS fixation, the peak displacements of the proximal femur were 7.446 mm, 7.416 mm, 7.324 mm, 8.138 mm, and 8.246 mm in the 120°, 125°, 130°, 135°, and 140° groups, respectively. For the five angular FNS fixation groups, the magnitude of proximal femoral displacement during stress varied as follows: 130° FNS fixation group, < 125° FNS fixation group, < 120° FNS fixation group, < 135° FNS fixation group, and < 140° FNS fixation group. Displacement occurred vertically downward along the direction of stress.
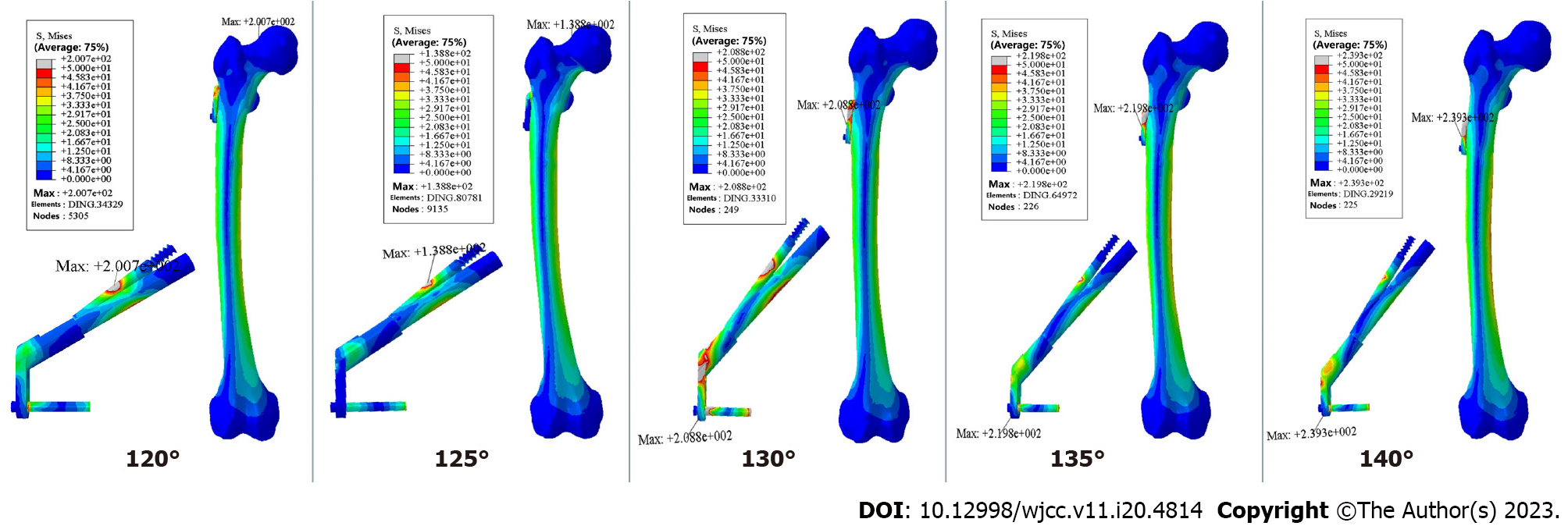
It has previously been shown that when fixing Pauwels-I-model fractures of the femoral neck with varying angles of FNS, the stresses were distributed throughout the femoral neck and femoral diaphysis area, with the maximum stresses concentrated on the internally fixed FNS (Figure 5). In the 120° and 125° FNS fixation groups, the maximum stresses were concentrated on the main nail and the anti-rotation screw and intersected with the femoral neck fracture line, with peak stresses of 200.7 MPa and 138.8 MPa, respectively. The maximum stress of 208.8 MPa, 219.8 MPa, and 239.3 MPa was observed on the locking screws of the angular distal locking plate in the 130°, 135°, and 140° FNS fixation groups. In descending order, the stresses were as follows: 125° FNS fixation group, < 120° FNS fixation group, < 130° FNS fixation group, < 135° FNS fixation group, and < 140° FNS fixation group.
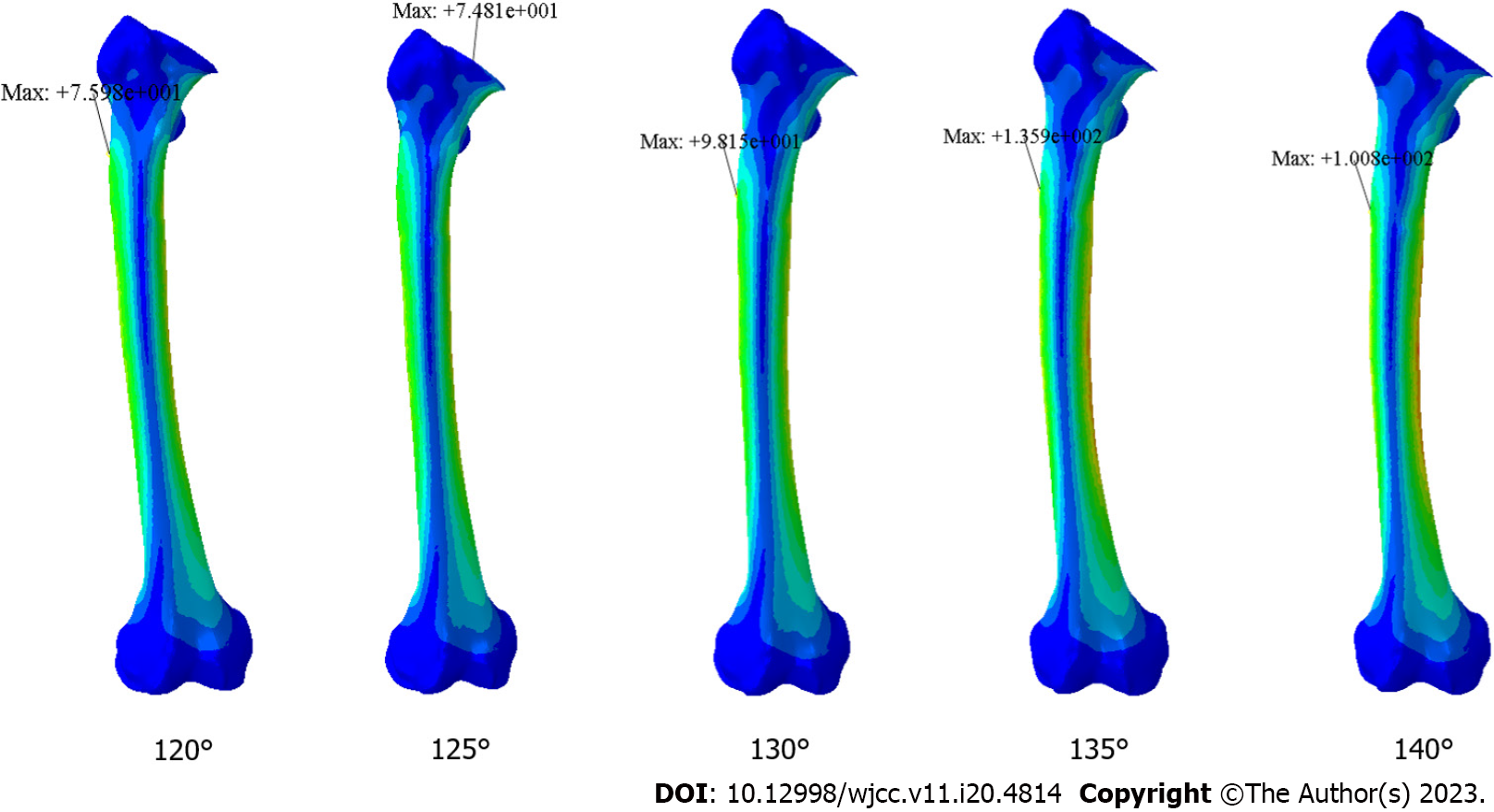
In different FNS fixation angles, the Von Mises stress on the femur was predominantly distributed in the femoral surgical neck and diaphysis, but the maximum stress concentration differed slightly. In the 120°, 130°, 135°, and 140° FNS fixation groups, peak stresses occurred on the locking screw distal to the lateral locking plate, with peak stresses of 75.98 MPa, 98.15 MPa, 135.9 MPa, and 100.8 MPa, respectively. In the 125° FNS fixation group, the maximum stress was concentrated at the intersection of the main nail and the fracture line, with a peak stress of 74.81 MPa. In ascending order, the maximum stress values were: 125° FNS fixation group, < 120° FNS fixation group, < 130° FNS fixation group, < 140° FNS fixation group, and < 135° FNS fixation group.
In addition to being a common traumatic fracture, femoral neck fractures are associated with a high mortality rate and disability[24,25]. Several surgical treatment strategies are available for femoral neck fractures, including internal fixation using hollow screws, intramedullary nails, locking plates, dynamic hip screws, and joint prostheses. The choice of technique is often selected according to the patient's condition and fracture type. FNS is an internal fixation system specifically designed for the fixation of femoral neck fractures. By incorporating the minimally invasive technique of hollow screw placement, this system reduces bone tissue damage and has a higher biomechanical strength than hollow screws, with considerable clinical application[26,27]. Additionally, this technique incorporates the pressure healing characteristics of the dynamic hip screw system; however, compared with DHS, the FNS is simpler to perform, involves a smaller incision, causes less trauma to the bone, and requires a smaller space for internal fixation[14].
Using FEA, the biomechanical characteristics of the FNS with different main nail angles were compared in the treatment of femoral neck fractures. When stress was applied to the 120° and 125° FNS fixation groups, the maximum stresses were found to be concentrated near the fracture line of the femoral neck. Upon reaching a main nail angle greater than 130°, the stressed concentration started to be transmitted to the femoral diaphysis through the greater trochanter, and the maximum stresses were exerted at the location of lateral locking. The larger the FNS angle, the higher the stress value at the locking screw. Accordingly, when the angle of the main nail is similar to that of the diaphysis in relation to the femoral neck, the stress distribution effects of the internal fixation system can be fully observed. The maximum stress concentration at the FNS locking screw indicates that the screw is subjected to a large load during stress distribution, resulting in the possibility of nonunion. In general, the larger the FNS main nail angle, the greater the risk for nonunion, especially in patients with a higher body mass index. This may explain the different locking screw numbers of FNS in clinics.
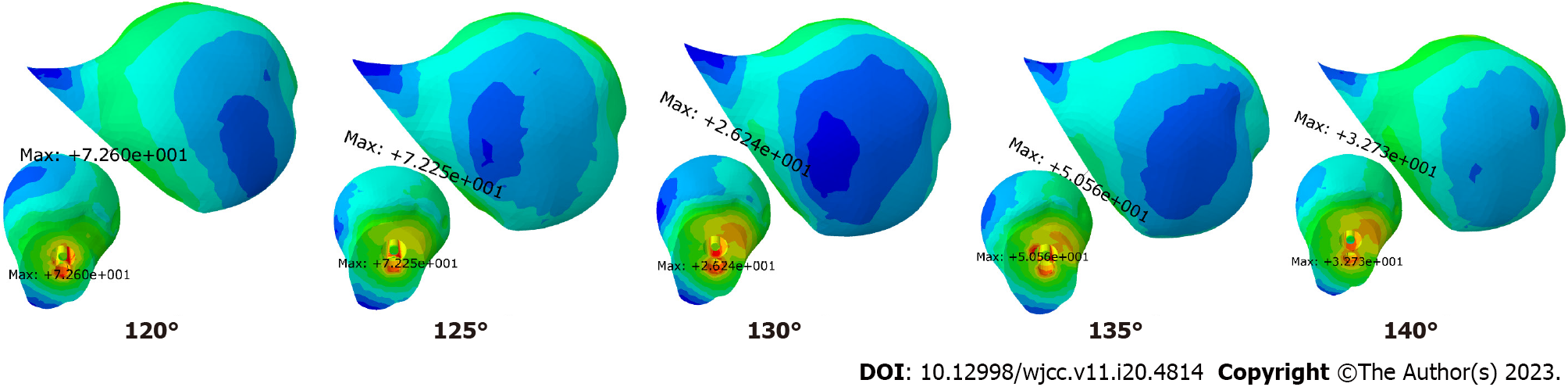
Furthermore femoral neck fractures are highly susceptible to femoral head necrosis following surgery. Indeed, one study reported that the rate of femoral head necrosis after hollow screw fixation of femoral neck fractures could reach 20.7%, and even for nondisplaced fractures, the rate was 4.7%[28]. As a result, femoral neck fractures are commonly termed "unresolved fractures"[29]. According to the present study's findings, FNS fixation of femoral neck fractures with 120° and 125° main nail angles resulted in a large peak stress on the femoral head due to poor stress distribution, which was greater than that of the other FNS fixation groups (Figure 6). Moreover, poor intraoperative realignment greatly increases the risk of femoral head necrosis[30]. At 130° FNS fixation angles, the peak stress on the femoral head is minimal, as is the displacement of the proximal femur. Compared to the 120° and 125° fixation groups, the 135° and 140° fixation groups have lower peak stresses on the femoral head, but the displacement of the proximal femur is greater in both groups, resulting in the postoperative displacement of the fracture end. As a result, poor realignment occurs, and there is an increased risk of femoral head necrosis (Table 2). For this reason, FNS with a main nail angle of 130° has a significant advantage over other angles in treating femoral neck fractures to prevent femoral head necrosis.
| 120° fixed group | 125° fixed group | 130° fixed group | 135° fixed group | 140° fixed group | |
| Maximum stress value (MPa) | 72.6 | 72.25 | 26.24 | 52.21 | 32.73 |
| Maximum displacement (mm) | 7.446 | 7.416 | 7.324 | 8.138 | 8.246 |
The magnitude of the displacement caused by the applied stress to the proximal femur during FNS fixation directly reflects the mechanical stability of the joint. As shown in Table 2, the displacement of the proximal femur in the 130° FNS fixation group was the lowest, while in terms of stress distribution, the stress distribution in the femur was more uniform in the 130° FNS fixation group, and the maximum stress occurred at the proximal end of the femoral diaphysis, which indicated an effective distribution of stress (Figure 7). Thus, we can conclude that the FNS with a main nail angle of 130° has better stability and stress distribution than with other angles. A further consideration is that the static fixation simulation model used in the present study is not representative of real-life scenarios with other involved structures, soft tissues, muscles, or ligaments, while the patient's femur is realigned intraoperatively. In these study results, the minimum displacement reached 7.324 mm, which would be considerably greater than the displacement generated by FNS in practice. Meanwhile, in real-life scenarios, the femur will be subjected to static forces and dynamic forces during walking and other processes. These will have to be better simulated to obtain more accurate simulation results. To account for these limitations, the simulation could be repeated with both a dynamic bone and muscular system analysis.
Using the same mechanical environment presented in this study, we further simulated and analyzed the performance of DHS, locking compression plates, three hollow nails, four hollow nails, and intramedullary nails when fixing femoral neck fractures[31]. Furthermore, combined with the results of this study, we found that the displacements of the FNS fixation group were smaller and more stable than those of several other internal fixation groups, as reported in related studies[26]. FNS has been demonstrated to be more effective in terms of clinical efficacy regarding postoperative rehabilitation[32], which enhances patient quality of life and accelerates the recovery of hip function.
The fracture model used in this study was a Pauwels type I femoral neck fracture, classified as a stable fracture. The type of fracture can be added later to gain a more comprehensive understanding of the mechanical stability of FNS with different main nail fixation angles. Besides, the limitation of this study was that FNS were not subjected to clinical or experimental testing for mechanical properties due to their limited material. Mechanical properties are essential in load-bearing conditions for providing structural support[33]. Therefore, this limitation can be overcome by product customization and mechanical testing to improve results.
Based on the results of this study, we found that a main nail FNS angle of 130° has the best stability for treating femoral neck fractures in Asian populations with quantifiable stress distribution and minimal proximal femoral displacement.
The suitability of the 130° main nail angle design of the femoral neck dynamic intersection system (FNS) for Asian populations lacks relevant research reports.
To provide clinical guidance for the future treatment of femoral neck fracture and internal fixation optimization in Asian populations.
To compare the biomechanical stability differences in various FNS main nail angles for treating femoral neck fractures in Asian populations.
FNS models with different nail angles were designed, and the femur computed tomography (CT) data of the Asian population were utilized for mechanical simulation analysis of FNS treatment for femoral neck fractures.
The magnitude of proximal femoral displacement during stress varied as follows: 130° FNS fixation group, < 125° FNS fixation group, < 120° FNS fixation group, < 135° FNS fixation group, and < 140° FNS fixation group. The stresses of FNS were as follows: 125° FNS fixation group, < 120° FNS fixation group, < 130° FNS fixation group, < 135° FNS fixation group, and < 140° FNS fixation group. The Von Mises stress on the femur was predominantly distributed in the femoral surgical neck and diaphysis, and the maximum stress values were: 125° FNS fixation group, < 120° FNS fixation group, < 130° FNS fixation group, < 140° FNS fixation group, and < 135° FNS fixation group.
The main nail FNS angle of 130° has the best stability for treating femoral neck fractures in Asian populations with quantifiable stress distribution and minimal proximal femoral displacement.
To gain a more comprehensive understanding of the mechanical properties of FNS with different main nail fixation angles, the type of fracture and the test in clinical or experimental can be added later.
| 1. | Swart E, Roulette P, Leas D, Bozic KJ, Karunakar M. ORIF or Arthroplasty for Displaced Femoral Neck Fractures in Patients Younger Than 65 Years Old: An Economic Decision Analysis. J Bone Joint Surg Am. 2017;99:65-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 2. | Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1375] [Cited by in RCA: 1537] [Article Influence: 53.0] [Reference Citation Analysis (0)] |
| 3. | Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20:1633-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 768] [Article Influence: 45.2] [Reference Citation Analysis (0)] |
| 4. | Tian FM, Zhang L, Zhao HY, Liang CY, Zhang N, Song HP. An increase in the incidence of hip fractures in Tangshan, China. Osteoporos Int. 2014;25:1321-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Slobogean GP, Stockton DJ, Zeng B, Wang D, Ma BT, Pollak AN. Femoral Neck Fractures in Adults Treated With Internal Fixation: A Prospective Multicenter Chinese Cohort. J Am Acad Orthop Surg. 2017;25:297-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Yang JZ, Zhou XF, Zhu WB, Li L, Xu W, Xia R, Wang G, Hua XY, Xu XZ, Fang SY, Xu L. A comparative study of short-term clinical effects between femoral neck system and cannulated compression screws in treatment of femoral neck fractures in young adults. CJOT. 2021;23:761-768. [DOI] [Full Text] |
| 7. | Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16:370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 87] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 8. | Xu XZ, Chang Q, Yu SS, Zhao Y, Xu CG, Zhang JS, Xie WK, Jing JH. Fixation with Femoral Neck System for femoral neck fractures: short-term therapeutic outcomes. CJOT. 2020;22:624-627. [DOI] [Full Text] |
| 9. | Ren C, Ma T, Li M, Xu YB, Li Z, Sun L, Xue HZ, Wang Q, Lu Y, Zhang K. Short-term clinical efficacy of femoral neck system for treatment of femoral neck fractures in young and middle-aged patients. CJOT. 2021;23:769-774. [DOI] [Full Text] |
| 10. | Lu Y, Canavese F, Nan G, Lin R, Huang Y, Pan N, Chen S. Is Femoral Neck System a Valid Alternative for the Treatment of Displaced Femoral Neck Fractures in Adolescents? A Comparative Study of Femoral Neck System versus Cannulated Compression Screw. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 11. | Wu ZF, Luo ZH, Hu LC, Luo YW. Efficacy of the femoral neck system in femoral neck fracture treatment in adults: A systematic review and meta-analysis. World J Clin Cases. 2022;10:11454-11465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Schopper C, Zderic I, Menze J, Müller D, Rocci M, Knobe M, Shoda E, Richards G, Gueorguiev B, Stoffel K. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J Orthop Translat. 2020;24:88-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 13. | Deng SY, Tan SL, Yan GH, Du Z, Cheng JW. Finite element analysis of femoral neck system and dynamic hip screw for pauwels II femoral neck fractures. Chinese Journal of Experimental Surgery. 2021;38:1959. [DOI] [Full Text] |
| 14. | Xu X, Fan J, Zhou F, Lv Y, Tian Y, Ji H, Zhang Z, Guo Y, Yang Z, Hou G. Comparison of femoral neck system to multiple cancellous screws and dynamic hip screws in the treatment of femoral neck fractures. Injury. 2023;54 Suppl 2:S28-S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 15. | Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, Oswald M, Gueorguiev B. Biomechanical Evaluation of the Femoral Neck System in Unstable Pauwels III Femoral Neck Fractures: A Comparison with the Dynamic Hip Screw and Cannulated Screws. J Orthop Trauma. 2017;31:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 214] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 16. | Hartel MJ, Petersik A, Schmidt A, Kendoff D, Nüchtern J, Rueger JM, Lehmann W, Grossterlinden LG. Determination of Femoral Neck Angle and Torsion Angle Utilizing a Novel Three-Dimensional Modeling and Analytical Technology Based on CT Datasets. PLoS One. 2016;11:e0149480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 17. | Tauviqirrahman M, Ammarullah MI, Jamari J, Saputra E, Winarni TI, Kurniawan FD, Shiddiq SA, van der Heide E. Analysis of contact pressure in a 3D model of dual-mobility hip joint prosthesis under a gait cycle. Sci Rep. 2023;13:3564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 33] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 18. | Jamari J, Ammarullah MI, Santoso G, Sugiharto S, Supriyono T, Permana MS, Winarni TI, van der Heide E. Adopted walking condition for computational simulation approach on bearing of hip joint prosthesis: review over the past 30 years. Heliyon. 2022;8:e12050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (1)] |
| 19. | Ammarullah MI, Hartono R, Supriyono T, Santoso G, Sugiharto S, Permana MS. Polycrystalline Diamond as a Potential Material for the Hard-on-Hard Bearing of Total Hip Prosthesis: Von Mises Stress Analysis. Biomedicines. 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 67] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 20. | Samsami S, Saberi S, Sadighi S, Rouhi G. Comparison of Three Fixation Methods for Femoral Neck Fracture in Young Adults: Experimental and Numerical Investigations. J Med Biol Eng. 2015;35:566-579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 99] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 21. | Cheung JT, Zhang M, Leung AK, Fan YB. Three-dimensional finite element analysis of the foot during standing--a material sensitivity study. J Biomech. 2005;38:1045-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 252] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 22. | Wang CJ, Yettram AL, Yao MS, Procter P. Finite element analysis of a Gamma nail within a fractured femur. Med Eng Phys. 1998;20:677-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Ammarullah MI, Afif IY, Maula MI, Winarni TI, Tauviqirrahman M, Akbar I, Basri H, van der Heide E, Jamari J. Tresca Stress Simulation of Metal-on-Metal Total Hip Arthroplasty during Normal Walking Activity. Materials (Basel). 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 24. | Li XP, Zhang P, Zhu SW, Yang MH, Wu XB, Jiang XY. All-cause mortality risk in older patients with femoral neck fracture. BMC Musculoskelet Disord. 2022;23:941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 25. | Rajeev A, Ali M, Tuinebreijer W, Zourob E, Anto J. Preexisting dementia is associated with higher mortality rate in patients with femoral neck fracture. Aging Med (Milton). 2021;4:12-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Fan ZR, Su HT, Zhou L, Huang HD, Zhou JD, Jiang T, Liu ZT. Finite element analysis of novel femoral neck system for unstable femoral neck fractures. CJTER. 2021;944:31-38. [DOI] [Full Text] |
| 27. | Xiong W, Yi M, Long C, Liu L, Cen SQ, Huang FG, Tang YF, Wang GL. A comparative study of femoral neck system vs inverted triangle cannulated compression screws in fixation of adult femoral neck fracture. CJOT. 2021;23:748-753. [DOI] [Full Text] |
| 28. | Konarski W, Poboży T, Kotela A, Śliwczyński A, Kotela I, Hordowicz M, Krakowiak J. The Risk of Avascular Necrosis Following the Stabilization of Femoral Neck Fractures: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 29. | Li M, Cole PA. Anatomical considerations in adult femoral neck fractures: how anatomy influences the treatment issues? Injury. 2015;46:453-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 30. | Wang Y, Ma JX, Yin T, Han Z, Cui SS, Liu ZP, Ma XL. Correlation Between Reduction Quality of Femoral Neck Fracture and Femoral Head Necrosis Based on Biomechanics. Orthop Surg. 2019;11:318-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 31. | Wang Y, Liu ZP, Yin T, Zhao YL, Han B, Guo CW, Teng YB, Fan ZR, Yang BC, Ma XL. Finite Element study on biomechanics of internal fixation for femoral neck fracture. Zhongguo Zhongxiyi Jiehe Waike Zazhi. 2019;25:56-61. [DOI] [Full Text] |
| 32. | Zhang B, Zhang Y, She RF, Jiang KD, Zhang LB, Min YC. A comparative study of the short-term effects of femoral neck system and cannulated compression screws in the treatment of femoral neck fracture under the concept of enhanced recovery alter' surgery. Guke Linchuang Yu Yanjiu Zazhi. 2022;7:15-21. [DOI] [Full Text] |
| 33. | Prakoso AT, Basri H, Adanta D, Yani I, Ammarullah MI, Akbar I, Ghazali FA, Syahrom A, Kamarul T. The Effect of Tortuosity on Permeability of Porous Scaffold. Biomedicines. 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 67] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ammarullah MI, Indonesia; Wu CC, Taiwan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH