Published online Jul 6, 2023. doi: 10.12998/wjcc.v11.i19.4625
Peer-review started: January 24, 2023
First decision: April 20, 2023
Revised: May 8, 2023
Accepted: May 31, 2023
Article in press: May 31, 2023
Published online: July 6, 2023
Processing time: 156 Days and 13.9 Hours
The medial patellofemoral ligament (MPFL), along with the medial patellotibial ligament (MPTL) and medial patellomeniscal ligament, aid in the stabilization of the patellofemoral joint. Although the MPFL is the primary stabilizer and the MPTL is a secondary limiter, this ligament is critical in maintaining joint stability. There have been few studies on the combined MPFL and MPTL reconstruction and its benefits.
To look into the outcomes of combined MPFL and MPTL reconstruction in frequent patellar instability.
By May 8, 2022, four electronic databases were searched: Medline (PubMed), Scopus, Web of Science, and Google Scholar. General keywords such as "patellar instability," "patellar dislocation," "MPFL," "medial patellofemoral ligament," "MPTL," and "medial patellotibial ligament" were co-searched to increase the sensitivity of the search.
The pooled effects of combined MPFL and MPTL reconstruction for Kujala score (12-mo follow-up) and Kujala score (24-mo follow-up) were positive and incremental, according to the findings of this meta-analysis. The mean difference between the Cincinnati scores was also positive, but not statistically significant. The combination of the two surgeries reduces pain. According to cumulative meta-analysis, the trend of pain reduction in various studies is declining over time.
The combined MPFL and MPTL reconstruction has good clinical results in knee function and, in addition to providing good control to maintain patellofemoral joint balance, the patient's pain level decreases over time, making it a valid surgical method for patella stabilization.
Core Tip: In patellar instability, combined medial patellofemoral ligament and medial patellotibial ligament reconstruction is associated with good clinical outcomes and can be considered a standard treatment in patellar instability treatment guidelines.
- Citation: Abbaszadeh A, Saeedi M, Hoveidaei AH, Dadgostar H, Razi S, Razi M. Combined medial patellofemoral ligament and medial patellotibial ligament reconstruction in recurrent patellar instability: A systematic review and meta-analysis. World J Clin Cases 2023; 11(19): 4625-4634
- URL: https://www.wjgnet.com/2307-8960/full/v11/i19/4625.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i19.4625
The patella is a vital component of the knee joint that includes the extensor mechanism. The main stabilizing ligamentous structure, the medial patellofemoral ligament (MPFL), allows the patella to stabilize in conjunction with the medial patellotibial ligament (MPTL) and medial patellomeniscal ligament (MPML). During knee movements, the MPFL is important in maintaining the patella's stability and position and is thought to be the primary internal stabilizing ligament[1,2]. Although the MPFL ligament is the primary stabilizer, the MPTL and MPML ligaments also play an important role in maintaining joint stability, particularly in the final stages of stretching from 26 degrees in extension and 46 to 90 degrees in flexion[3].
Recurrent patella dislocation is associated with patella alta, a large Q angle, a hypoplastic lateral femoral condyle, and congenital ligament laxity[2,4,5]. According to a review of the literature, most patients with non-surgical treatments experience frequent instability in the injured knee and reduced activity level[6]. A large number of surgical methods for treating patellofemoral instability have been described in various studies, but the best method is still controversial[7,8].
MPFL reconstruction is widely recognized as an important component of the current treatment for recurrent patellar instability. This method can be used alone or in conjunction with bone methods such as tibial tuberosity distalization or trochleoplasty in the case of patella alta or high-grade trochlear dysplasia[9]. Another surgical method is a combined MPFL and MPTL reconstruction, which has yielded positive results in clinical trials. In a cohort study conducted by Hetsroni, the effect of combined surgery (MPFL and MPTL) was investigated during 73 mo on the patients. Their findings showed that combined surgery in young patients improved knee function better than MPFL surgery alone and maintained patella-femoral balance with more degrees of flexion, even though they did not return to pre-injury levels of activity[10,11]. Hence, according to role of MPTL reconstruction in combination of MPFL reconstruction in treatment of patella instability and the fact that many studies have not been done in this field, the present study was performed with the purpose of studying the combined MPFL and MPTL reconstruction in recurrent patellar instability.
To find relevant studies, a comprehensive literature search for English-language observational studies was performed in Medline (PubMed), Scopus, Web of Science and Google Scholar. In order to maximize the sensitivity of the search, general keywords such as "patellar instability", “patellar dislocation”, “MPFL”, “medial patellofemoral ligament”, “MPTL”, and “medial patellotibial ligament” were co-searched (Supplementary material). The results of searches were refined through checking for and removing duplicate papers.
In keeping with standard meta-analysis techniques and PRISMA guidelines[12], we included studies published to May 8, 2022. Studies were independently selected for inclusion and only the original papers were included in the review. Two investigators independently applied the inclusion and exclusion criteria, which had questions about the main methodological aspects of descriptive studies, such as the sampling method, measurement of variables, objectives, and statistical analysis.
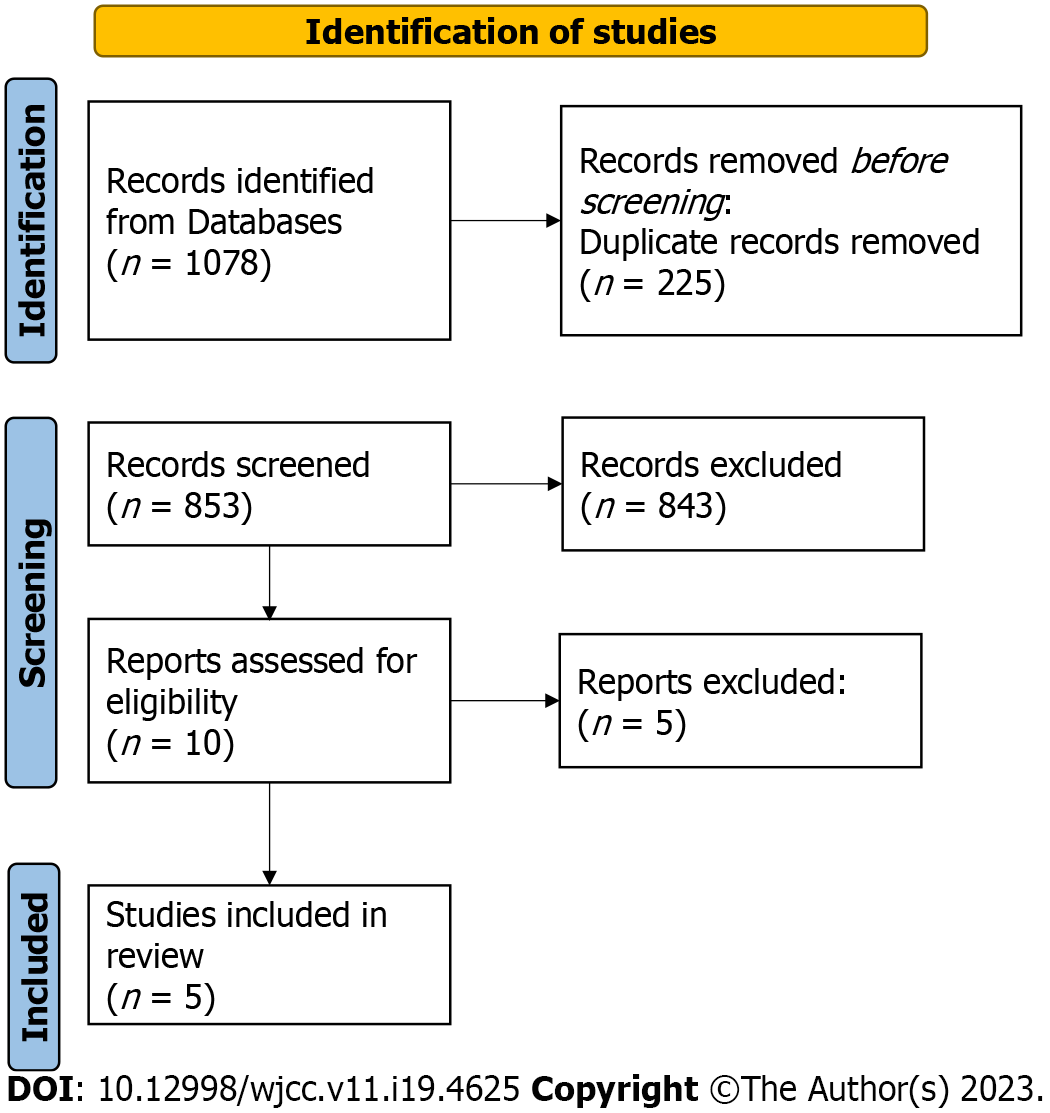
To be included in this study, inclusion criteria were: (1) Studies that used both MPFL and MPTL methods simultaneously for recurrent patellar instability; and (2) Primary studies. And Exclusion criteria were: (1) Not primary studies as well as those with only poster presentation; (2) Duplicated publication (we included just one); and (3) Studies that used only one of two methods, MPFL or MPTL for recurrent patellar instability. Figure 1 shows the PRISMA flow diagram.
All publications were reviewed independently by two researchers (Mohsen Saeedi and Ahmad Abbaszadeh). In case of discrepancies between investigators regarding inclusion criteria, it was resolved by the third author (Haleh Dadgostar). After the final evaluation, the selected publications were briefed by the name of first author, date of publication, country, sample size, study design, age average, Extension, Flexion, International knee Documentation Committee score, visual analogue scale (VAS), Patellar tilt, Patellar shift, Insall–Salvati ratio, Modified Insall–Salvati ratio, Caton–Deschamps Index, Tibial tuberosity-trochlear groove (TT–TG) distance, Kujala score, Cincinnati, Lysholm, range of motion (ROM) in degrees and Congruence angle. All the extracted data were then entered into Excel software.
In this study, due to the small number of studies in this field, publication bias was not investigated.
The "metan" command was used to apply a fixed or random effects model based on the results of Cochran's Q test or a large Higgins and Thompson’s I2 value. Standardized mean difference (SMD) estimated by Hedges' g based on sample size, mean, and standard deviation before and after intervention. Forest plots were used to describe the results graphically. In addition, the "metacum" command was used for cumulative meta-analysis to determine the trend of the Kujala score. Stata software (version 14) was used for all statistical analyses.
Five studies with a sample size of 148 knees after surgery were included in the systematic review and meta-analysis after reviewing and evaluating collected papers. These papers were published between 2013 and 2020. The highest average age was in the Maffulli study, which was 26.5 + 10.7 years. These studies were conducted in five countries. Only one study used Extension, Flexion, Caton-Deschamps Index, Tegner score, Patellar Shift, and Modified Insall-Salvati Ratio to assess the effect of combined medial patellofemoral and patellotibial ligament reconstruction. TT–TG distance and congruence angle were reported in two studies, but in one study, the value before surgery was the only one available. ROM and Lysholm were also reported in two studies, but the follow-up period was 12 mo in one study and 24 mo in another study. In two studies, the Insall–Salvati ratio was reported, but in one of them, the standard deviation was not reported. By the way, the average of VAS, patellar tilt angle, and Cincinnati were reported in two studies with a follow-up period of 24 mo. The Kujala score was also reported with a follow-up period of 12 mo in two studies and a follow-up period of 24 mo in four studies. More details about the studies are given in Tables 1-4.
| ID | Ref. | Year1 | Type of study | Country | N | Mean age | Male/female | IKDC score | Extension, degree | Flexion, degree | VAS | ||||||||
| Preop2 | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | ||||||||
| 1 | Maffulli et al[24] | 2020 | Prospective cohort | Italy | 34 | 26.5 ± 10.7 | 27:7 | ||||||||||||
| 2 | Yang et al[15] | 2019 | Prospective | China | 58 | 22.6 ± 4.9 | 25:23 | 51.9 ± 13.8 | 80 ± 19.2 | 85 ± 13.9 | 2 ± 3 | 2 ± 4 | 3 ± 4 | 143 ± 7 | 141 ± 8 | 142 ± 7 | 58 ± 11 | 12 ± 5 | 11 ± 4 |
| 3 | Hetsroni et al[10] | 2019 | - | Israel | 20 | 18 ± 2 | 6:14 | 75.7 ± 18.1 | |||||||||||
| 4 | Sadigursky et al[19] | 2017 | Case series | Brazil | 7 | 11.28 ± 1.49 | 4:3 | ||||||||||||
| 5 | Sobhy et al[22] | 2013 | Prospective | Egypt | 29 | 20.1 ± 3 | 21:8 | 63 ± 13 | 18 ± 9.7 | ||||||||||
| ID | Ref. | Year1 | Type of study | Country | N | Mean age | Male/female | Caton–deschamps index | TT–TG distance, mm | Kujala score | Cincinnati | ||||||||
| Preop2 | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | ||||||||
| 1 | Maffulli et al[24] | 2020 | Prospective cohort | Italy | 34 | 26.5 ± 10.7 | 21:8 | 47 ± 17 | 82 ± 175 | 51 ± 22 | 90 ± 19 | ||||||||
| 2 | Yang et al[15] | 2019 | Prospective | China | 58 | 22.6 ± 4.9 | 21:8 | 1.41 ± 0.21 | 1.32 ± 0.17 | 1.31 ± 0.17 | 21.5 ± 0.6 | 20.2 ± 1.5 | 19.9 ± 1.7 | 55.1 ± 15.2 | 82.6 ± 14.9 | 89.5 ± 10.2 | |||
| 3 | Hetsroni et al[10] | 2019 | - | Israel | 20 | 18 ± 2 | 21:8 | 54.9 ± 15.2 | 86.4 ± 12.56 | ||||||||||
| 4 | Sadigursky et al[19] | 2017 | Case series | Brazil | 7 | 11.28 ± 1.49 | 21:8 | 42.57 ± 8.9 | 88.57 ± 5.09 | ||||||||||
| 5 | Sobhy et al[22] | 2013 | Prospective | Egypt | 29 | 20.1 ± 3 | 21:8 | 36.6 ± 6 | 90.6 ± 7 | 50 ± 7.1 | 88 ± 6 | ||||||||
| ID | Ref. | Year1 | Type of study | Country | N | Mean age | Male/female | Lysholm | ROM, degree | Congruence angle | Tegner score | ||||||||
| Preop2 | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | ||||||||
| 1 | Maffulli et al[24] | 2020 | prospective cohort | Italy | 34 | 26.5 ± 10.7 | 21:8 | ||||||||||||
| 2 | Yang et al[15] | 2019 | prospective | China | 58 | 22.6 ± 4.9 | 21:8 | ||||||||||||
| 3 | Hetsroni et al[10] | 2019 | - | Israel | 20 | 18 ± 2 | 21:8 | 4 ± 3 | 4.8 ± 2.45 | ||||||||||
| 4 | Sadigursky et al[19] | 2017 | case series | Brazil | 7 | 11.28 ± 1.49 | 21:8 | 33.71 ± 9.6 | 87.71 ± 5.70 | 117.85 ± 8.09 | 148.57 ± 3.77 | ||||||||
| 5 | Sobhy et al[22] | 2013 | prospective | Egypt | 29 | 20.1 ± 3 | 21:8 | 51.9 ± 4.7 | 89.5 ± 5.6 | 112.1 ± 7.1 | 136.7 ± 8.5 | 11.93±1.85 | -6.48 ± 3.8 | ||||||
| ID | Ref. | Year1 | Type of study | Country | N | Mean age | Male/female | Patellar tilt angle | Patellar shift, mm | Insall–Salvati ratio | Modified Insall–Salvati ratio | ||||||||
| Preop2 | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | Preop | 12 mo3 | 24 mo4 | ||||||||
| 1 | Maffulli et al[24] | 2020 | Prospective cohort | Italy | 34 | 26.5 ± 10.7 | 21:8 | 1.1 | 1.1 | ||||||||||
| 2 | Yang et al[15] | 2019 | Prospective | China | 58 | 22.6 ± 4.9 | 21:8 | 19.1 ± 7.2 | 11.5 ± 5.6 | 11.3 ± 5.2 | 6.2 ± 2.1 | 1.2 ± 0.6 | 1.1 ± 0.7 | 1.49 ± 0.22 | 1.39 ± 0.23 | 1.37 ± 0.19 | 2.25 ± 0.18 | 1.95 ± 0.22 | 1.95 ± 0.25 |
| 3 | Hetsroni et al[10] | 2019 | - | Israel | 20 | 18 ± 2 | 21:8 | ||||||||||||
| 4 | Sadigursky et al[19] | 2017 | Case series | Brazil | 7 | 11.28 ± 1.49 | 21:8 | ||||||||||||
| 5 | Sobhy et al[22] | 2013 | Prospective | Egypt | 29 | 20.1 ± 3 | 21:8 | 10.9 ± 1.7 | 2.45 ± 2.2 | ||||||||||
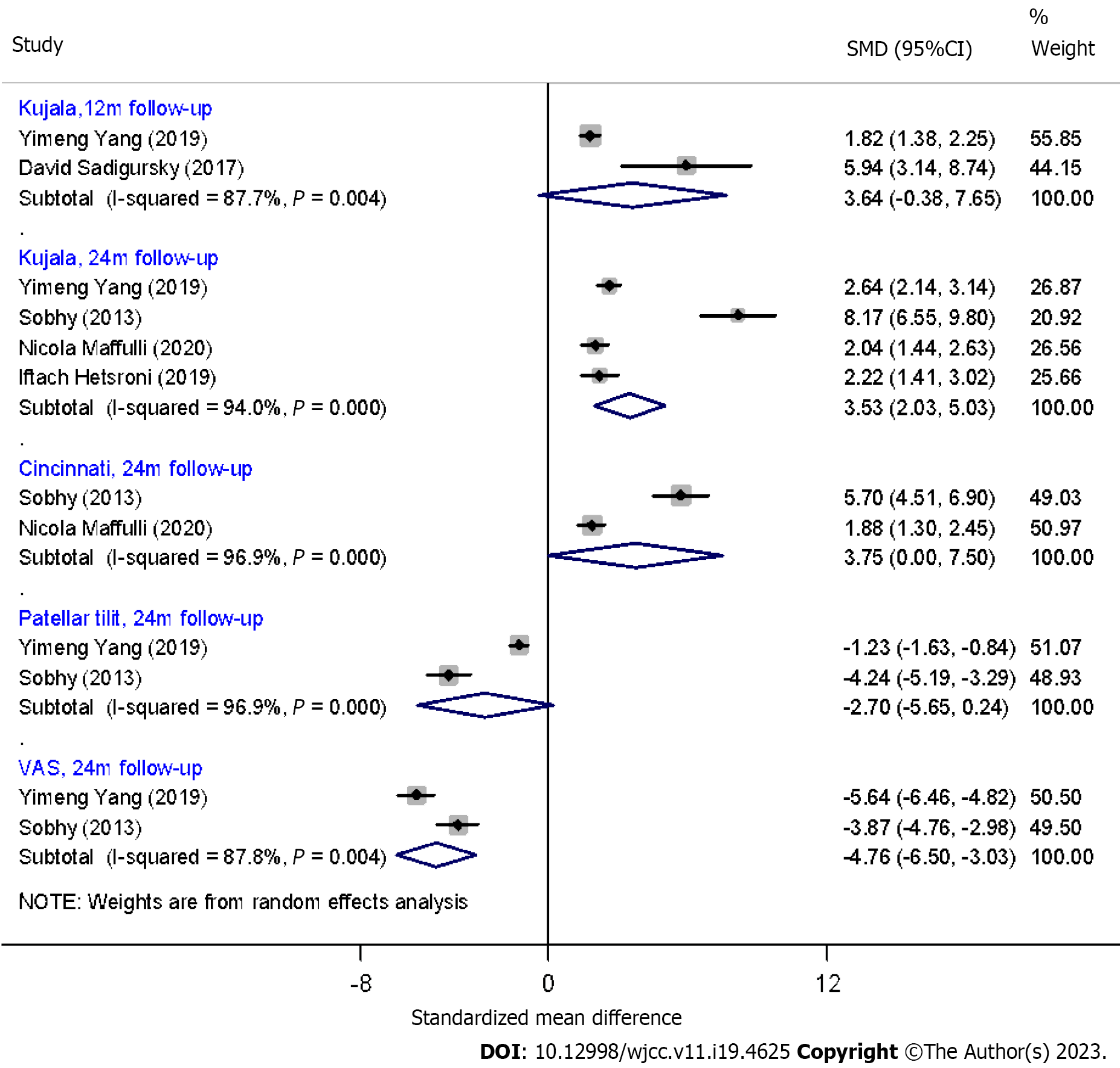
According to these studies, the pooled effects of combined medial patellofemoral and patellotibial ligament reconstruction changes for Kujala score (12 mo and 24 mo follow-up) were positive and incremental (SMD = 3.64; 95%CI: -0.38 to 7.65 and SMD = 3.53; 95%CI: 2.03 to 3.03, respectively), but they were significant only for the 24 mo follow-up. The mean difference for Cincinnati was also positive but not statistically significant (SMD = 7.74; 95%CI: -2.95 to 18.44 and SMD = 3.75; 95%CI: 0-7.5, respectively). SMD for VAS was -4.76 mm and significant 95%CI: -6.5 to -30.03, which means that the combined effect of the two treatments can reduce the amount of pain (Figure 2). Also, according to the cumulative meta-analysis, the rate of pain reduction in different studies is decreasing over time (a decrease in the SMD value from 8.17 to 2.04).
Patellar instability is one of the most common causes of knee injury and anterior knee pain, and it is associated with frequent dislocation, which prevents most patients from returning to sports and physical activities[13,14]. The main finding of this systematic review was that the combined surgical method of MPFL and MPTL reconstruction has good clinical outcomes in terms of knee function, and that patients' pain levels decrease over time, in addition to good control of patellofemoral balance. Although MPFL surgery alone was popular in the past, studies have shown that this treatment method was ineffective in some patellar conditions such as patella alta, and reconstruction of this ligament with the MPFL method alone increased the level of knee function but was ineffective when compared to the combined method[15]. According to the findings of a study conducted by Ambra et al[16], the MPFL method alone was ineffective in treating patellar instability.
The combined reconstruction (MPFL, MPTL) is typically used in patients who have at least two lateral patella dislocations, a delta patella, an increased TT-TG distance greater than 20 mm, an Insall-salvative-index greater than 1.2, multiple ligament damage, and an unstable joint[17]. The studies revealed that, while the MPFL ligament acts as the primary internal stabilizer of the patella, the MPTL is also required as a secondary lateral stabilizer to maintain patella stability and improve knee function, emphasizing the practical importance of combined surgery (MPFL, MPTL)[18].
In the current study, the Kujala score improved significantly after 12 and 24 mo of follow-up. After combined MPFL and MPTL reconstruction, the patients' performance level improved and their knee pain decreased.
According to the studies reviewed, the SMD for VAS was -4.76 mm, which was statistically significant. It demonstrates that combining MPFL and MPTL reconstruction can reduce pain. Furthermore, according to a meta-analysis, the rate of pain reduction in various studies is decreasing over time. (SMD decreased from 8.17 to 2.04). This study found that combining MPFL and MPTL reconstruction can reduce knee pain over time while also increasing knee stability and function. Perhaps it is due to the method's anatomical and biomechanical similarities with the normal knee. Then, it may be an effective method of treating recurrent Patella instability.
Yang et al[15] discovered that normalizing the size and height of the patella, as well as decreasing its slope, can lead to increased tendon stability and pain reduction over time. Moreover, studies show that combining MPFL and MPTL reconstruction reduces the need for procedures like Tibial Tuberosity Osteotomy (TTO) and surgical complications in comparison to MPFL Reconstruction on its own[14]. Another study found that combined reconstruction can stabilize the patella even in the presence of other factors when treating patellar instability in children with TT-TG>15 mm. In other words, the children's performance and range of motion improved, as measured by the Kujala and Lysholm scores[19].
Furthermore, patellar tilt angle was measured in two studies over a period of 24 mo. This angle decreased after surgery, but it was not statistically significant, which could be attributed to the small sample size in the studies examined. Over the last few years, there has been an increase in interest in the combined reconstruction of MPFI and MPTL in the management of recurrent patella instability. It could be because new histological, anatomical, and biomechanical studies have revealed that the MPTL is a true ligament that is important for patellofemoral stability[4,20].
In patients with moderate dysplasia, combined reconstruction of MPFL and MPTL may reduce the need for both bony procedures such as TTO and trochleoplasty[21]. Furthermore, it may improve outcomes when compared to MPFL reconstruction alone[1,20,22,23].
Therefore, combined MPFI and MPTI reconstruction is a safe method for management of recurrent Patella Dislocation and in the future, it may become a part of the algorithms used for the treatment of recurrent Patella instability. However, based on some previous studies, the conclusion stating that the combined procedure would be beneficial has to be made with caution.
The study's limitations included a small number of studies and a lack of randomized controlled trials. There are no randomized controlled trials that compare this method to other surgical treatments, and no article included a control group. The current study's strength is the use of precise inclusion and exclusion criteria, as well as the use of meta-analysis, which made our study more reliable.
The current meta-analysis review study found that combining MPTL and MPFL is a safe method with favorable clinical results in patellar dislocation and instability, with fewer complications and the possibility of patellar recurrence or subluxation. There is a need for clinical trial studies with a control group and long-term follow-ups to know the desired results of the surgery, as well as comparing this method with the MPFL method alone, due to a lack of studies and samples in the research conducted in this field.
The patellofemoral joint stability is aided by the medial patellofemoral ligament (MPFL), along with the medial patellotibial ligament (MPTL) and medial patellomeniscal ligament (MPML). While the MPFL is the primary stabilizer, the MPTL plays a critical role as a secondary limiter. However, there are limited studies on the combined reconstruction of MPFL and MPTL and its advantages.
Different studies on the results of patellar instability management are published with no certain consensus. So, it was necessary to do an analysis to clarify the role of combined reconstruction of MPFL and MPTL in patellar instability management.
To find out the efficacy of combined reconstruction of MPFL and MPTL.
Several databases were searched to obtain eligible randomized controlled trials. Outcomes were mechanical ventilation time, length of intensive care unit stay, and duration of postoperative hospitalization.
Combined MPFL and MPTL reconstruction led to positive outcomes in Kujala scores at 12 and 24-mo follow-ups. The surgeries reduced pain, but the trend of pain reduction decreased over time according to cumulative meta-analysis.
Combined MPFL and MPTL reconstruction is a safe method with favorable clinical results in patellar dislocation and instability.
Our conclusion needs further confirmation through the conduct of additional high-quality studies.
| 1. | Ebied AM, El-Kholy W. Reconstruction of the medial patello-femoral and patello-tibial ligaments for treatment of patellar instability. Knee Surg Sports Traumatol Arthrosc. 2012;20:926-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Garth WP Jr, Connor GS, Futch L, Belarmino H. Patellar subluxation at terminal knee extension: isolated deficiency of the medial patellomeniscal ligament. J Bone Joint Surg Am. 2011;93:954-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 139] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 4. | Hinckel BB, Gobbi RG, Demange MK, Pereira CAM, Pécora JR, Natalino RJM, Miyahira L, Kubota BS, Camanho GL. Medial Patellofemoral Ligament, Medial Patellotibial Ligament, and Medial Patellomeniscal Ligament: Anatomic, Histologic, Radiographic, and Biomechanical Study. Arthroscopy. 2017;33:1862-1873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Arendt EA, Dejour D. Patella instability: building bridges across the ocean a historic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:279-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 6. | Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, Marcacci M. Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2491-2498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Aulisa AG, Falciglia F, Giordano M, Savignoni P, Guzzanti V. Galeazzi's modified technique for recurrent patella dislocation in skeletally immature patients. J Orthop Sci. 2012;17:148-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Sappey-Marinier E, Sonnery-Cottet B, O'Loughlin P, Ouanezar H, Reina Fernandes L, Kouevidjin B, Thaunat M. Clinical Outcomes and Predictive Factors for Failure With Isolated MPFL Reconstruction for Recurrent Patellar Instability: A Series of 211 Reconstructions With a Minimum Follow-up of 3 Years. Am J Sports Med. 2019;47:1323-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 157] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 9. | Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916-1923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 405] [Cited by in RCA: 371] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 10. | Hetsroni I, Mann G, Dolev E, Nyska M. Combined reconstruction of the medial patellofemoral and medial patellotibial ligaments: outcomes and prognostic factors. Knee Surg Sports Traumatol Arthrosc. 2019;27:507-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;174-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 375] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 48646] [Article Influence: 2861.5] [Reference Citation Analysis (3)] |
| 13. | Ambrožič B, Novak S, Nabergoj M. Medial Patellofemoral Ligament Reconstruction Techniques. In: Springer, Clinical Anatomy of the Knee. 2021: 163-174. |
| 14. | Aicale R, Maffulli N. Combined medial patellofemoral and medial patellotibial reconstruction for patellar instability: a PRISMA systematic review. J Orthop Surg Res. 2020;15:529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Yang Y, Zhang Q. Reconstruction of the medial patellofemoral ligament and reinforcement of the medial patellotibial ligament is an effective treatment for patellofemoral instability with patella alta. Knee Surg Sports Traumatol Arthrosc. 2019;27:2599-2607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Ambra LF, Franciozi CE, Phan A, Faloppa F, Gomoll AH. Isolated MPTL reconstruction fails to restore lateral patellar stability when compared to MPFL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2021;29:793-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Allen MM, Krych AJ, Johnson NR, Mohan R, Stuart MJ, Dahm DL. Combined Tibial Tubercle Osteotomy and Medial Patellofemoral Ligament Reconstruction for Recurrent Lateral Patellar Instability in Patients With Multiple Anatomic Risk Factors. Arthroscopy. 2018;34:2420-2426.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 18. | Halloran JP, Esquivel AO, Cracchiolo AM, Chen C, Lemos SE. The Role of the MPFL and MPTL in Patellar Stability–A Biomechanical Study. Archives of Orthopaedics. 2020;1(2): 49-54. [DOI] [Full Text] |
| 19. | Sadigursky D, Garcia LC, Armede M, Oliveira LR, Carneiro RJF, Colavolpe PO. Medial patellofemoral ligament and medial patellotibial ligament reconstruction in children: preliminary results. Rev Bras Ortop. 2017;52:417-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 20. | Brown GD, Ahmad CS. Combined medial patellofemoral ligament and medial patellotibial ligament reconstruction in skeletally immature patients. J Knee Surg. 2008;21:328-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Hinckel BB, Gobbi RG, Kaleka CC, Camanho GL, Arendt EA. Medial patellotibial ligament and medial patellomeniscal ligament: anatomy, imaging, biomechanics, and clinical review. Knee Surg Sports Traumatol Arthrosc. 2018;26:685-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 22. | Sobhy MH, Mahran MA, Kamel EM. Midterm results of combined patellofemoral and patellotibial ligaments reconstruction in recurrent patellar dislocation. Eur J Orthop Surg Traumatol. 2013;23:465-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Drez D Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 227] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 24. | Maffulli N, Aicale R, D'Addona A, Young DA, Kader DF, Oliva F. Combined medial patellofemoral and patellotibial reconstruction with soft tissue fixation in recurrent patellar dislocation. Injury. 2020;51:1867-1873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Iranian Orthopedic Association, President; Iranian Society of Knee Surgery, Arthroscopy, and Sports Traumatology, Past President; Asian Federation of Sports Medicine, Past President.
Specialty type: Orthopedics
Country/Territory of origin: Iran
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oommen AT, India S-Editor: Ma YJ L-Editor: A P-Editor: Zhao S