Published online Jul 6, 2023. doi: 10.12998/wjcc.v11.i19.4531
Peer-review started: April 6, 2023
First decision: April 19, 2023
Revised: May 8, 2023
Accepted: May 22, 2023
Article in press: May 22, 2023
Published online: July 6, 2023
Processing time: 85 Days and 3.1 Hours
Stroke is a common cause of neurological dysfunction, often resulting in hemi
To investigate whether unilateral strength training in hemiplegic stroke patients could lead to cross-migration, an increase in bilateral muscle strength, and an improvement in lower limb motor function.
We randomly divided 120 patients with hemiplegic stroke into two groups: Eexperimental and control groups, with 60 patients in each group. Both groups received routine rehabilitation treatment, while the experimental group additional
The FMA score in the experimental group improved significantly compared to both their pre-training score and the control group's post-training score (P < 0.05). The integrated EMG of the anterior tibialis muscle and pulmonary intestine muscle in the experimental group were significantly different after training than before (P < 0.05). Furthermore, the MVC of the anterior tibialis muscle on both the healthy and affected sides and the MVC of the pulmonary intestine muscle on both sides showed significant improvement compared with before training and the control group (P < 0.05).
Our findings suggest that ankle dorsiflexion resistance training on the healthy side in hemiplegic stroke patients can increase strength in the opposite tibialis anterior muscle and antagonist's muscle, indicating a cross-migration phenomenon of strength training. Furthermore, this type of training can also improve lower limb motor function, providing a new exercise method for improving early ankle dorsiflexion dysfunction.
Core Tip: Unilateral ankle dorsiflexion resistance training on the healthy side can improve lower limb motor function and lead to cross-migration of strength in hemiplegic stroke patients.
- Citation: Lu YH, Fu Y, Shu J, Yan LY, Shen HJ. Application of cross-migration theory in limb rehabilitation of stroke patients with hemiplegia. World J Clin Cases 2023; 11(19): 4531-4543
- URL: https://www.wjgnet.com/2307-8960/full/v11/i19/4531.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i19.4531
Stroke, also known as a cerebrovascular accident, refers to acute cerebral vasospasm, occlusion, or rupture caused by various reasons, resulting in neurological impairment diseases dominated by hemiplegia. The incidence of stroke is very high, and the complications are characterized by high disability and high recurrence rate. Hemiplegia is a syndrome with the main clinical manifestation of incomplete or complete loss of random movement of one side of the limbs caused by brain diseases[1]. China is the largest country in the world affected by strokes. Every year, there are two million new stroke patients, with one-third of them having obvious disabilities and 80%-90% having movement disorders. Rehabilitation of patients' limb functions is an essential step in their recovery and return to their families and society. It is the most important part of rehabilitation care. Under stable conditions, rehabilitation nursing can effectively accelerate the recovery time of patients, minimize the disability of patients, improve recovery of patients' self-care ability, and thus improve the quality of life of stroke patients.
In sports physiology, there is a phenomenon of cross-migration of training effects, which means that unilateral limb movement can produce simultaneous improvement in the functions of opposite homologous parts (strength, joint range of motion, function)[2]. Short, high-intensity resistance exercises on one side of a healthy person's limb can cause the strength of the untrained limb on the opposite side to increase[3]. It has been found that training the opposite arm can offset muscle atrophy caused by limb fixation, and the phenomenon of cross-migration is unilateral, which can only be transferred from the dominant limb to the non-dominant limb[4]. Training the healthy side of the limb inhibits the flexor modes of the upper limb and the extensor modes of the lower limb, effectively establishing a normal mode. This improves the level of ADL[5]. Cross–migration could be applied in stroke patients with hemiplegia, and equal-length resistance training could be performed on the healthy side to increase the strength of the affected side without exercise and improve the motor function of lower limbs[6]. It shows that when joints and muscles of one side of a limb are injured, their injuries and dysfunction can affect both sides of the limb, leading to a decline of the healthy side function. It suggests that training uninjured limbs may be one of the important measures to prevent its occurrence. Even for stroke patients in the 1st week, muscle strength of the healthy side lower limb has decreased to varying degrees, and the state of the healthy side limb will affect the overall function of stroke patients[7]. It also shows that muscular atrophy and hypotonia in stroke patients are not limited to paralyzed limbs but also can cause disuse muscular atrophy and hypotonia in healthy limbs.
At present, a consensus has been reached on the training of affected limbs, with various theories and training methods emerging endlessly. For stroke patients with hemiplegia, functional training of the affected limb is generally emphasized, while compensation and functional training of the healthy limb is easily ignored. In clinical rehabilitation training, therapists pay more attention to the recovery of the limb function of the affected side but neglect or pay less attention to functional activities of the healthy side, leading to the disuse degradation of the healthy side. Active exercise of healthy limbs can improve the tension of the central nervous system, activate the physiological function of the system, prevent complications, improve the general condition, and increase the confidence of patients in rehabilitation[8]. It has been confirmed that cross-migration refers to the concept that training one side of a limb can not only enhance the muscle strength of that side of the limb but also enhance the muscle strength of the opposite limb that has not received direct training[9]. The study found that functional exercise of healthy limbs can accelerate the establishment of ipsilateral cerebral collateral circulation, promote the recurrence of tissues around lesions, and further enhance the functional recovery of affected limbs. Bilateral exercise can promote the formation of new brain nerve channels, aid in the recovery of neural function, and trigger changes in EMG signals[10]. A study of 20 stroke patients who trained five times per week for 5 wk found that maximum wrist resistance training increased extension strength by 42% in the healthy wrist and 35% in the affected wrist. The scores of motor function assessment (FMA) of four patients increased, and longer training time resulted in a more noticeable rehabilitation effect. The rehabilitation of healthy limbs is not only effective for establishing collateral circulation but also improves daily life capacities. The rehabilitation training of healthy limbs is equally important to rehabilitation training of affected limbs in the functional recovery of hemiplegia.
Stroke has become one of the global public health problems, with the highest incidence observed in people aged ≥ 41-50 years. Motor dysfunction is one of the most common dysfunctions in stroke, and early successful rehabilitation nursing can reduce muscle atrophy, joint dislocation, joint contracture deformity, foot drop, or varus, which drugs cannot replace. Resistance movement is a type of resistance movement of the limbs that uses muscle-strength exercise equipment (such as sandbags and elastic belts). It increases the diameter of muscle fibers, exercises muscles, and effectively enhances muscle strength through rhythmic weight bearing and repeated exercises. Active exercise against resistance is the best approach to enhance muscle strength and has a positive effect on enhancing bone density and bone metabolism. Current scientific consensus is that 3-6 sets of resistance exercise are optimal for strength gains. Beyond 6 sets, there is no additional benefit for strength[11]. After 12 wk of low-intensity resistance exercise, the lower limb movement ability of older people has been improved to a certain extent.
Rehabilitation nursing intervention for stroke patients can improve the effect of nursing, help patients recover better, and improve patient satisfaction. Nursing intervention aims to improve the quality of life and self-management ability during the recovery period from a stroke. The resistance exercise based on cross-migration theory has a broad application prospect for the rehabilitation of limb motor function of stroke patients. However, there is little research on this model of resistance exercise worldwide. The central control mechanism of cross-migration and how to effectively use this principle in the field of rehabilitation still needs to be further explored.
This study focuses on patients with unilateral hemiplegia after stroke. The research team was comprised of rehabilitation nurses, doctors, and therapists. Under the guidance of cross-migration theory, while carrying out routine rehabilitation training of the affected limb, we provided progressive resistance exercise training to the healthy limb through nursing intervention to maintain muscle strength of the healthy limb, promote the growth of muscle strength of the affected limb, prevent disuse syndrome, improve motor function, improve patient's quality of life, and improve nursing satisfaction.
Between September 2020 and June 2022, we selected 120 eligible stroke hemiplegic patients hospitalized in the geriatric rehabilitation department of our hospital, randomly dividing them into control and experimental groups with 60 patients in each. Patients received conventional therapies, such as improving cerebral microcirculation, protecting nerves, and promoting metabolism. The control group received conventional rehabilitation training, while the experimental group added healthy side-limb resistance exercise to their conventional rehabilitation training. We compared the improvement of hemiplegic limb muscle strength, peak change of surface electromyography, and FMA score before the intervention, 4 wk after the intervention, and 12 wk after the intervention.
We created a sports manual and videos of healthy limb resistance movement; We purchased the necessary equipment for the study, including standard sandbags weighing 0.5kg-2.5kg.
Inclusion criteria: (1) The diagnosis was in line with the diagnostic criteria for stroke formulated at the 4th Academic Conference on Cerebrovascular Diseases and confirmed by head computed tomography or magnetic resonance imaging scanning; (2) The primary disease was stroke, and there was no obvious dysfunction before onset; (3) The course of the disease is within 1-6 mo, and the condition is stable; (4) The patients were aged between 50-79; and (5) One side was hemiplegic. The muscle strength of the hemiplegic side is ≤ 2 Levels, and the muscle strength of the healthy side is 4-5 Levels.
Exclusion criteria: (1) People with aphasia, cognitive impairment, and other nervous system symptoms that made them unstable and unable to communicate; (2) People with severe osteoporosis, traumatic diseases, or peripheral nerve injury; (3) People with acute joint disease and injury; (4) People with severely limited joint mobility; and (5) People with serious heart, liver, kidney diseases, or bleeding diseases in the past.
We used PASS11 to estimate the sample size with α = 0.05 (one side), β = 0.1, a ratio of 1:1 (prevalence rate was 0.5). The results showed that at least 106 people, including 53 patients and 53 controls, should be included. Considering a 10% loss rate, we included 60 patients and 60 controls in the study. A total of 120 patients were enrolled in the control and experimental groups, respectively.
We recorded the personal information of 120 subjects, including name, sex, age, diagnosis, contact address, and telephone number, in a registration book and entered it into a computer for archiving so that subjects could better cooperate with the study and follow-up.
Control group: We implemented routine rehabilitation training: After the rehabilitation assessment, the rehabilitation physician issued a sports prescription, and the rehabilitation therapist implemented sports therapy based on the patient's condition and limb dysfunction. The treatment consisted of Placement and conversion of antispasmodic postures; the range of motion training of hemiplegic limbs; muscle strength training of hemiplegic side; bridge sports; bedside sitting balance training; standing balance training; activities of daily living ability training.
The above treatment was administered once a day, for 30 min each time, five times a week, for 6 consecutive weeks. The intensity and time of each training were properly adjusted according to the patient's movements, step by step, so as not to increase the patient's overall spasticity or cause excessive fatigue.
Patients in the control group also received routine health education. The responsible nurse issued an exercise manual and instructed patients to move the healthy side of their limb autonomously.
Experimental group: Progressive resistance exercise of the contralateral side was carried out as described below. The experimental group received a sports intervention consisting of rehabilitation nurses, doctors, and therapists. The head nurse acted as the team leader and coordinated the intervention and health education activities. The rehabilitation physician formulated the intervention plan and dealt with adverse events. The rehabilitation therapist was responsible for routine exercise training, evaluation, and collection of muscle strength and electromyography data. The researcher trained the team members through a PowerPoint and on-site demonstration to highlight the key points and precautions of the resistance movement. The rehabilitation nurse was mainly responsible for implementing the patient's healthy limb resistance exercise, monitoring the patient's discomfort, blood pressure, and heart rate changes during muscle strength training, and providing health education and discharge follow-up of patients and their families through WeChat management.
Health education included issuing exercise manuals to patients and their families, highlighting the importance of motor rehabilitation for stroke, and instructing patients and their families on the importance of healthy side movement as well as how to resist movement of healthy side limbs. Electronic screens were used to play an operation video of the resistance movement. WeChat groups were established for intervention members and patients or family members to provide related knowledge of stroke motor function exercise and enhance motor concept of patients and family members.
The movement mode for the experimental group was progressive resistance movement of the healthy side limb using sandbags to exert resistance. The standard sandbags purchased by the hospital's procurement office were ankle leggings sandbags and wrist leggings sandbag with a weight range of 0.5 kg-2.5 kg. Before the intervention, healthy side muscle strength was evaluated, and sandbags with appropriate weight were selected to apply resistance according to age and individual tolerance. The exercise intensity was medium to low and was evaluated according to Borg's subjective exertion scoring method. According to a patient's subjective feeling of exertion, a score of 6 points indicates no exertion, while a score of 20 points indicates exhaustion. If a patient's score was between 12 and 14 points, it indicated medium and low exercise intensity. If a subject experienced dizziness, asthma, dyspnea, arrhythmia, chest tightness, chest pain, and other discomfort symptoms, the exercise was stopped immediately. The exercise steps were divided into 4 wk of resistance exercise carried out 0.5 h after regular rehabilitation training, subject to completion of the specified number of times, each time for 30 min, five times a week, to avoid excessive exercise.
Before and after resistance exercise, warm-up exercises were carried out, including muscle relaxation exercises and gripping palm and finger joints exercises. The maximum exercise intensity of each patient was evaluated by a rehabilitation technician every week. The weight added every week was not more than 10% of the original; the weight of sandbags or the number of exercises that the patient could tolerate. The adaptation stage lasted about 1 wk, and the heart rate response to exercise was observed. In the improvement phase, the weight of the sandbag gradually increased. In the maintenance phase, the exercise intensity was maintained until the end of the intervention.
Upper limb exercise method: To apply resistance on the wrist, appropriate sandbags were selected and divided into two groups of five movements each. They included: shoulder joint horizontal adduction and abduction, shoulder joint forward flexion and extension, and elbow joint flexion and extension. There was a two- minute rest between the groups.
Lower limb exercise method: Appropriate sandbags were selected to apply resistance, and five movements were performed. They included: Straightening and lifting the lower limb of one side; and extending the knee joint. There was a two-minute rest between the sets.
Rehabilitation nurse education: The rehabilitation nurse educated the patients about the essential aspects of exercise training, emphasizing to both patients and their families that rehabilitation was a gradual process. The patients were encouraged to adhere to the training regime. Patients were given wrist and ankle sandbags and an exercise manual to continue functional exercise at home. Home caregivers were instructed to record the frequency and time of resistance movement of healthy side limbs in each diary.
WeChat and telephone follow-up: After discharge, the patients were followed up by WeChat and telephone. Home caregivers sent daily resistance exercise videos to the WeChat group. The rehabilitation nurses supervised the implementation of the exercise plan, answered questions of patients and their families, and ensured compliance of the exercise regime.
Regular outpatient visits: Patients were advised to regularly visit the geriatric rehabilitation department to evaluate their condition and motor function recovery. If necessary, the patients were re-admitted to the hospital for further rehabilitation treatment.
The patients were evaluated before the intervention, 4 wk after the intervention (after training), and 12wk after the intervention. The specific evaluation contents are described below.
Free hand muscle strength assessment: Muscle strength was measured according to the internationally accepted modified MRC grading assessment standard. Based on the Lovett grading method, muscle strength was further subdivided by the degree of motion amplitude and degree of applied resistance. The muscle strength test results are divided into 0-5 grades, with level 5 indicating normal force, level 4 indicating anti-gravity and resistance active motion, level 3 indicating anti-gravity but not resistance active motion, level 2 indicating gravity-free active motion, and level 1 indicating muscular contraction. Grade 0 meant no muscle contraction. If muscle strength reached a certain level, but the range of activity could not reach the full range, "-" was added to the upper right corner of the level symbol. If at the end of the movement, it showed resistance or gravity beyond the level, "+" was added to the upper right corner of the level symbol. The higher the percentage of normal muscle strength, the better the effect.
Surface electromyography: The subject's surface electromyography (sEMG) was monitored by removing oil with a 75% alcohol cotton ball and taking a supine position. The patient was required to perform isometric contraction with maximum strength, adhere to it for five seconds, and then perform voluntary contraction for 10 s after a rest of 1min. Surface EMG signals of the upper limb deltoid muscle, biceps brachii muscle, and lower limb quadriceps femoris muscle on the hemiplegic side were recorded, and EMG analysis software was used for signal processing and analysis. The ability of EMG signal is concentrated at 0-500Hz. After filtering, 3S extreme maximum voluntary contraction (MVC), integrated EMG value (IEMG), and root mean square value were selected to compare the activation intensity of EMG before and after training. The growth showed that muscle contraction was improved.
Limb function: The Fugl Meyer motor function evaluation scale was used to evaluate limb function. The total score of 100 points included two dimensions of upper and lower limb motor function, including 33 items of the upper limb, 0-2 points for each item, and 66 points for the total score. The lower limbs include 17 items with 0-2 points for each item and 34 points in total. The lower the score, the more serious the motor dysfunction of the patient (Figure 1).
Initially, 19 patients were enrolled in the clinical trial. However, 4 patients dropped out of the study, leaving 15 patients in the treatment group and 15 in the control group. Table 1 and Figure 1 present a comparison of the general characteristics of the subjects. Independent sample T test showed that there was no statistical difference in age, course of disease, height, and weight between the two groups (P < 0.05). Similarly, the chi-square test revealed no significant differences in sex and hemiplegic side limbs between the two groups (P < 0.05), indicating that the groups were comparable at baseline.
| Parameter | Experience, mean ± SD | Control, mean ± SD |
| Number | 60 | 60 |
| Left hemiplegia, n | 44 | 40 |
| Right hemiplegia, n | 16 | 20 |
| Male sex, n | 40 | 36 |
| Age in yr | 64.42 ± 9.12 | 63.82 ± 7.77 |
| Course of disease in d | 45.45 ± 15.34 | 49.00 ± 14.90 |
| Height in cm | 165.42 ± 6.91 | 164.45 ± 7.12 |
| Weight in kg | 64.25 ± 8.05 | 63.62 ± 9.64 |
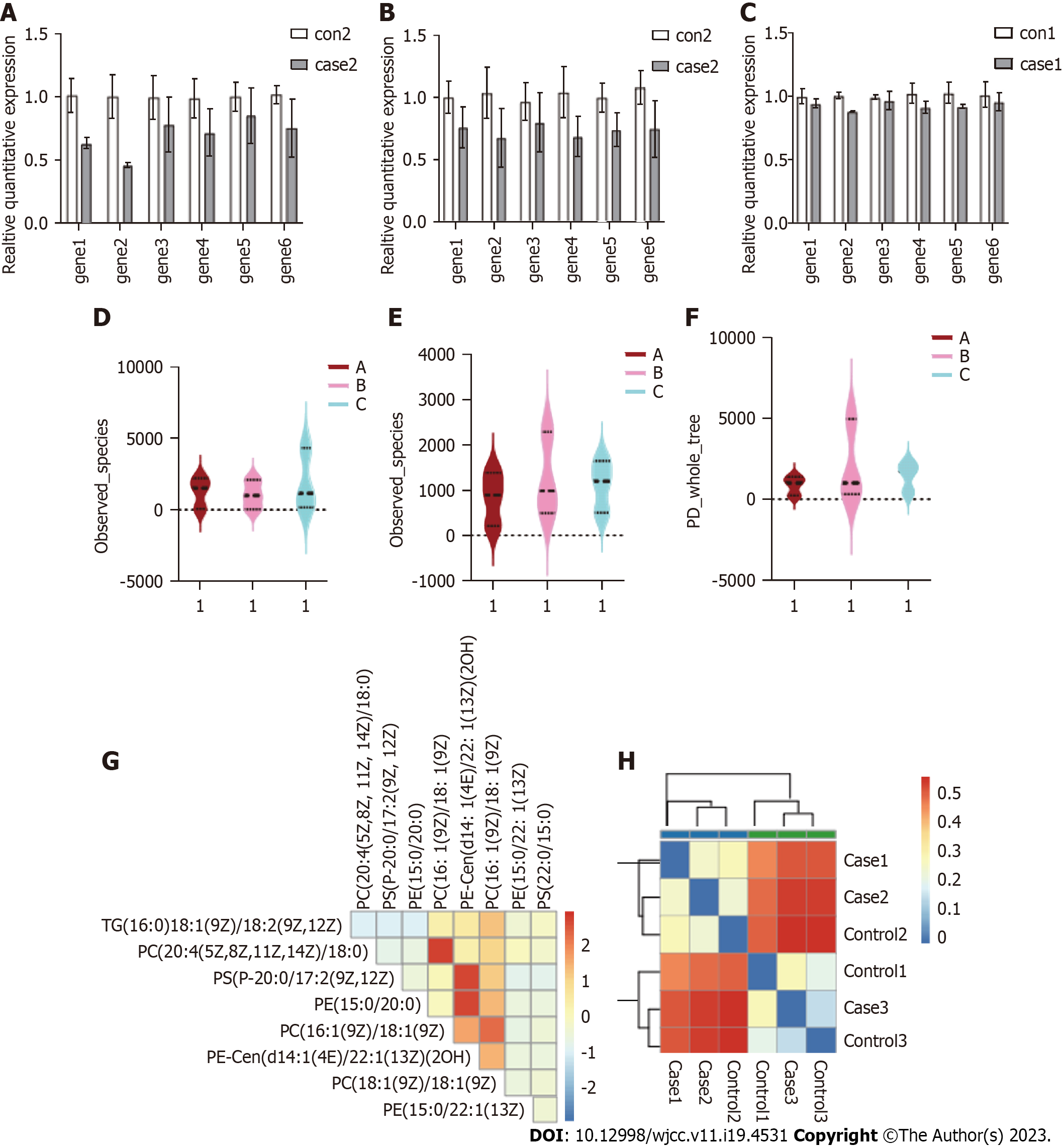
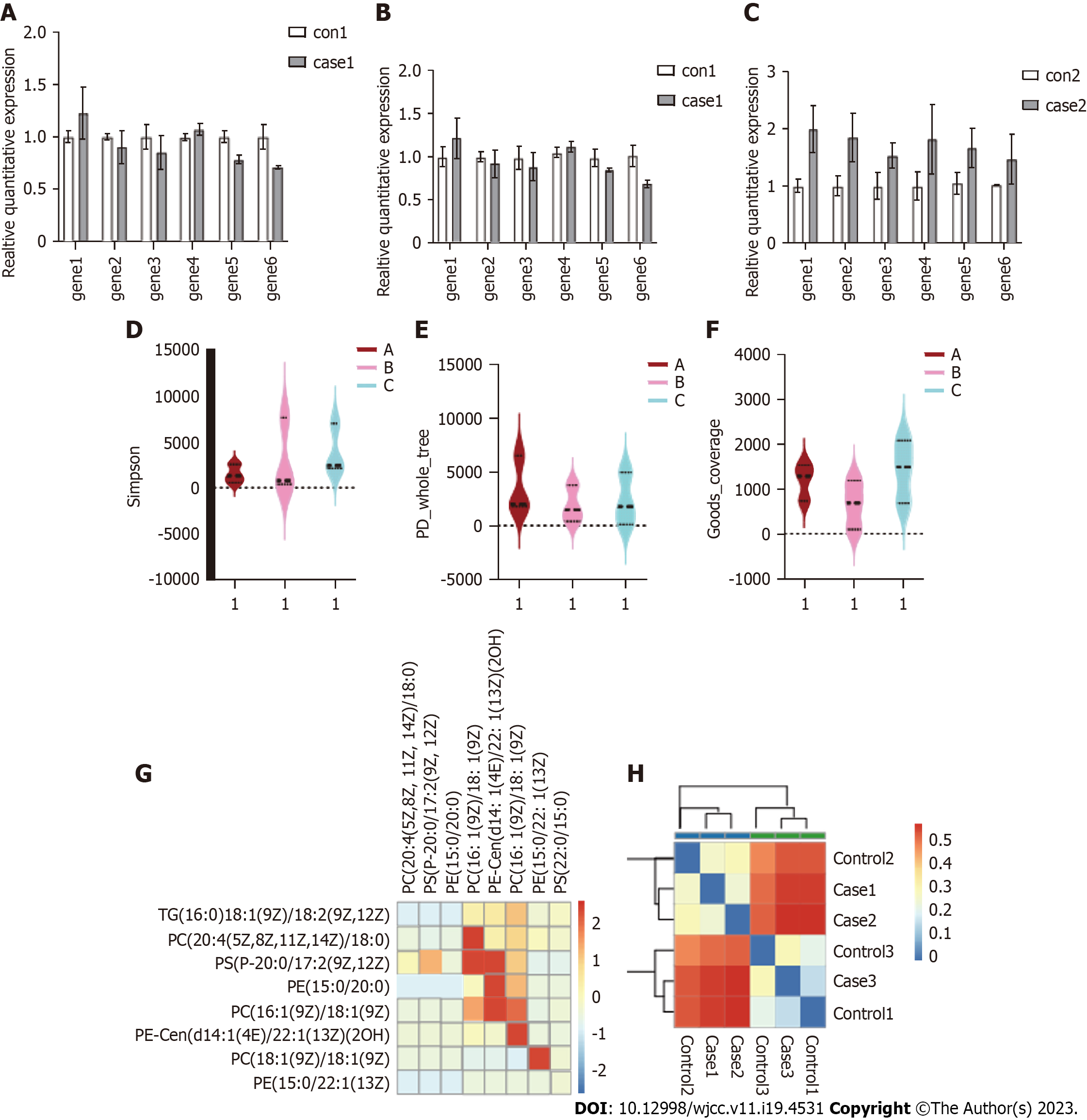
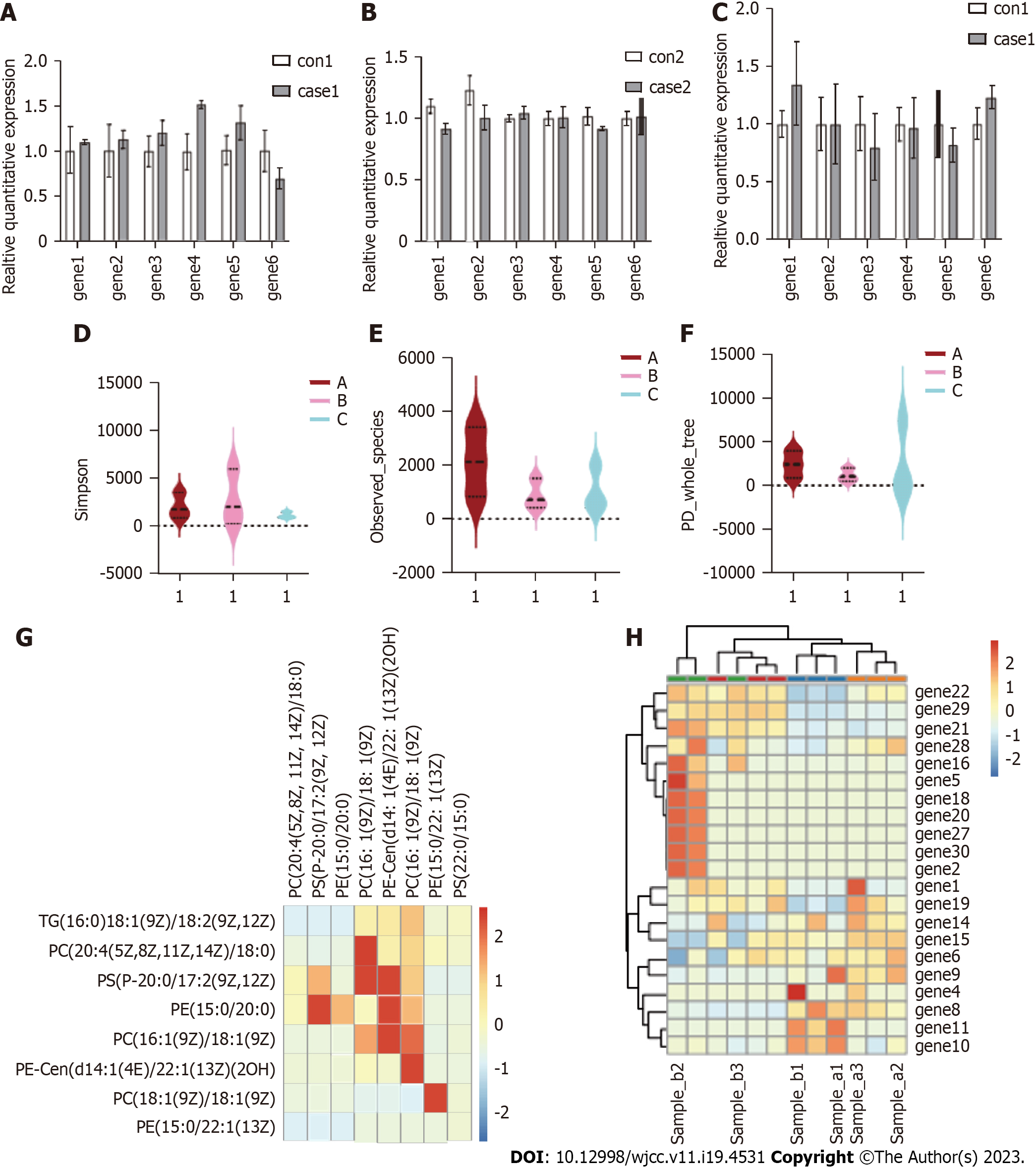
The FMA scores improved after the training intervention, with varying degrees of improvement between the treatment and control groups. The results are shown in Table 2 and Figure 2. Specifically, the FMA scores in the experimental group increased significantly compared to both pre-training and post-training scores in control group (P < 0.05). These results suggest that the training intervention effectively improved motor function of the experimental group.
| Indication | Treatment, mean ± SD | Control, mean ± SD | ||
| Before training | After training | Before training | After training | |
| FMA score, points | 20.05 ± 3.06 | 26.55 ± 2.66 | 19.15 ± 3.05 | 23.42 ± 2.94 |
After the training intervention, the MVC of the anterior tibialis muscle and pulmonary intercostal muscle on both the healthy and affected sides were significantly improved compared with pre-training values (P < 0.05), as presented in Table 3 and Figure 3. Furthermore, the MVC of the anterior tibialis muscle and pulmonary intercostal muscle on both the healthy and diseased sides in the experimental group were significantly higher than those in the control group (P < 0.05) after training. These findings suggest that the training intervention improved the muscle strength, particularly in the experimental group.
| Group | Cases, n | MVC of tibialis anterior muscle, kg, mean ± SD | MVC of gastrocnemius, kg, mean ± SD | ||
| Contralateral | Affected side | Contralateral | Affected side | ||
| Treatment group | |||||
| Before training | 60 | 10.43 ± 2.16 | 4.87 ± 2.08 | 11.07 ± 2.66 | 4.00 ± 1.36 |
| After training | 60 | 12.86 ± 1.75 | 8.21 ± 1.53 | 13.65 ± 2.86 | 7.77 ± 1.16 |
| Control group | |||||
| Before training | 60 | 9.82 ± 1.84 | 4.44 ± 2.03 | 10.91 ± 2.26 | 3.86 ± 1.55 |
| After training | 60 | 10.22 ± 1.54 | 6.97 ± 1.68 | 11.44 ± 2.34 | 6.87 ± 1.42 |
After the training intervention, the IEMG of the anterior tibialis muscle and pulmonary intercostal muscle on the healthy side in the experimental group was significantly different from pre-training values (P < 0.05), as shown in Table 4 and Figure 4. Additionally, IEMG of tibialis anterior and pulmonary intercostal muscles on both the healthy and affected sides in the experimental group were significantly different from those in the control group (P < 0.05) after training. These results suggested that the training intervention influenced the muscle activation patterns, particularly in the experimental group (Figure 5).
| Group | Cases, n | Tibial anterior muscle IEMG, mV, mean ± SD | Gastrocnemius IEMG, mV, mean ± SD | ||
| Contralateral | Affected side | Contralateral | Affected side | ||
| Treatment groups | |||||
| Before training | 60 | 60.05 ± 15.97 | 34.55 ± 5.76 | 49.71 ± 10.96 | 12.42 ± 6.11 |
| After training | 60 | 76.89 ± 8.41 | 58.45 ± 6.66 | 62.82 ± 8.76 | 32.45 ± 6.25 |
| Control groups | |||||
| Before training | 60 | 58.82 ± 16.07 | 32.71 ± 7.42 | 48.91 ± 10.97 | 12.31 ± 7.22 |
| After training | 60 | 62.05 ± 15.54 | 50.05 ± 10.35 | 50.65 ± 10.38 | 27.85 ± 7.91 |
Stroke, also known as a cerebrovascular accident or cerebrovascular disease, is a major health concern worldwide, particularly in aging populations. In China, the annual incidence rate of stroke exceeds 2.4 million with more than 70% of patients experiencing limb movement disorders in China[12]. Stroke survivors often experience functional disorders, including cognitive, sensory, language, and motor dysfunction. Motor dysfunction is the most common type, accounting for about 80% of stroke-related dysfunction[13,14].
Research has shown that up to 80% of stroke patients experience decreased upper limb motor function in the acute stage, and only 5% to 20% of patients recover full upper limb function even with rehabilitation treatment[15]. Myodynamia of hemiplegic limbs after stroke is a common problem that limits the rehabilitation of affected limb function, and the healthy side of stroke patients also suffers from myodynamia decline[16]. Currently, most of the treatment for stroke limb rehabilitation is limited to the hemiplegic side, and training of the healthy side is often ignored. Cross-migration is a training method that leverages unilateral limb training to stimulate strength development in the corresponding muscles on the opposite side of the limb. Therefore, cross-migration can be used to train the healthy side of stroke limbs to promote rehabilitation of the hemiplegic side[17].
This study investigated the effects of ankle dorsiflexion equal-length resistance training on the strength of the anterior tibialis muscle on the affected side of stroke hemiplegic patients as well as the strength of the pulmonary intestinal muscles. The results showed that after 6 wk of training, there was a significant increase in the strength of the anterior tibialis muscle of the affected side and the pulmonary intercostal muscles, compared to before training and the control group (P < 0.05).
Interestingly, ankle dorsiflexion equals length resistance training on the healthy side not only increased the strength of the affected side's tibialis anterior muscle without muscle strength training but also increased the strength of the antagonist's muscle. This phenomenon of cross-migration has been reported in previous studies, with two main mechanisms proposed: myogenic and neural[18,19]. A group of 30 young people received unilateral electrical stimulation and underwent maximum voluntary contraction strength training of the right lower limb for 6 wk. The results showed that high-intensity unilateral training increased the MVC of the opposite side, but there was no evidence of hypertrophy in the leg muscles, indicating that the myogenic mechanism does not play a major role in cross-migration[20,21]. Instead, the brain and spinal cord were found to play a significant role in the occurrence of cross-migration[22,23].
Additionally, it was observed that voluntary contraction could affect the motor pathway of the contralateral homologous muscle, which is consistent with the increase of motor cortex excitability and plays an important role in the strength training process[24,25]. Unilateral strength training was shown to increase the strength of both sides of the limbs, reduce inhibitory transmission of signals from the training side of the cerebral hemisphere to the untrained side, increase the excitability of the motor cortex on the same side of the trained limb, and reduce inhibition and transmission of bilateral corticospinal tracts.
In conclusion, while the mechanism of cross-migration requires further discussion and research, this study provides valuable insights into the neural mechanisms that underlie this phenomenon and its potential application in clinical rehabilitation.
The study concludes that ankle dorsiflexion resistance training on the healthy side can improve lower limb motor function and increase strength in the opposite tibialis anterior muscle and antagonist's muscle, suggesting a cross-migration phenomenon of strength training. This provides a new exercise method for improving early ankle dorsiflexion dysfunction in hemiplegic stroke patients.
Stroke-induced hemiplegia has a high incidence rate and is characterized by movement disorders. Rehabilitation of limb function is an essential step for patients' recovery, and resistance training is a promising method to improve muscle strength and motor function.
Rehabilitation care can accelerate stroke patients' recovery time, minimize disability, and improve their quality of life. This study aims to investigate the effectiveness of unilateral strength training in improving lower limb motor function and muscle strength in hemiplegic stroke patients.
The objective of this study is to investigate whether ankle dorsiflexion resistance training on the healthy side can lead to cross-migration of strength, an increase in bilateral muscle strength, and an improvement in lower limb motor function in hemiplegic stroke patients.
In this study, 120 hemiplegic stroke patients were randomly divided into two groups. The experimental group received ankle dorsiflexion resistance training on the healthy side for 6 wk, in addition to routine rehabilitation treatment. Both groups were assessed before and after the training using various measures, including EMG and FMA. Statistical analysis was conducted to compare the results between the two groups.
Ankle training improves post-stroke strength & motor function. Cross-migration phenomenon observed. New exercise method for early dysfunction.
Ankle training improves strength & motor function in stroke patients.
Could investigate the long-term effects and optimal duration/frequency of ankle training for stroke patients.
| 1. | Xu SY, Zhang M, Wu XW, Li L, Li CX. The mechanisms of limb hemiplegia after ipsilateral brain hemisphere stroke. Int J Clin Exp Med. 13:7386-7392. |
| 2. | Ling X, Zhang G, Xia Y, Zhu Q, Zhang J, Li Q, Niu X, Hu G, Yang Y, Wang Y, Deng Z. Exosomes from human urine-derived stem cells enhanced neurogenesis via miR-26a/HDAC6 axis after ischaemic stroke. J Cell Mol Med. 2020;24:640-654. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 89] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 3. | Zhang D, Liu G, Huang L, Zhang L, Gui X, Tao J, Zeng P, Ding M. Monitoring of Motor Nerve Function Rehabilitation in Patients with Upper Extremity Hemiplegia Based on Functional Magnetic Resonance Imaging. J Med Imaging Health Inform. 2021;11:1761-1770. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Knoll JM, Knight LR, Quiroz D, Popat SM, Pederson TG, Morton-Gonzaba N. Variation in Clinical Presentations and Outcomes of Heat Stroke Victims in the Mass-Casualty Setting. J Emerg Med. 2019;57:866-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Noh J, Jung E, Jung AY, Lee BH, Lee BS, Kim EAR, Kim KS. A Novel COL4A1 Mutation in a Neonate with Intrauterine Intraventricular Hemorrhage and Porencephaly. Neonatal Medicine. 2020;27:16-20. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Stancioiu F, Makk R. Post-stroke recovery of motor function with a new combination of medicines-A pilot study. EJMO. 2019;3:167-181. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Xie Q, Zhang X, Peng S, Sun J, Chen X, Deng Y, Yi L. Identification of novel biomarkers in ischemic stroke: a genome-wide integrated analysis. BMC Med Genet. 2020;21:66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Le Roux M, Barth M, Gueden S, Desbordes de Cepoy P, Aeby A, Vilain C, Hirsch E, de Saint Martin A, Portes VD, Lesca G, Riquet A, Chaton L, Villeneuve N, Villard L, Cances C, Valton L, Renaldo F, Vermersch AI, Altuzarra C, Nguyen-Morel MA, Van Gils J, Angelini C, Biraben A, Arnaud L, Riant F, Van Bogaert P. CACNA1A-associated epilepsy: Electroclinical findings and treatment response on seizures in 18 patients. Eur J Paediatr Neurol. 2021;33:75-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 9. | Ullah S, Bin Ayaz S, Zaheer Qureshi A, Samir Tantawy S, Fe Flandez M. Characteristics and functional outcomes of pediatric stroke survivors at a rehabilitation unit in Saudi Arabia. J Clin Neurosci. 2020;81:403-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Ghosh MK, Chakraborty D, Sarkar S, Bhowmik A, Basu M. The interrelationship between cerebral ischemic stroke and glioma: a comprehensive study of recent reports. Signal Transduct Target Ther. 2019;4:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 11. | Prasetyanto D, Yona S. Meridian acupuncture in stroke rehabilitation: a literature review. IJNHS. 2019;2:48-54. [DOI] [Full Text] |
| 12. | Borlongan CV. Concise Review: Stem Cell Therapy for Stroke Patients: Are We There Yet? Stem Cells Transl Med. 2019;8:983-988. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 100] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 13. | Subbarayan MK, Chinnaiyan P, Sampati S. Study of high specific c-reactive protein in acute ischaemic stroke. J Evol Med Dent Sci. 2019;8:1243-1248. [DOI] [Full Text] |
| 14. | Löwe B, Gerloff C. Functional somatic symptoms across cultures: Perceptual and health care issues. Psychosom Med. 2018;80:412-415. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Yu S, Lam C, Shinde S, Kuczynski AM, Carlson HL, Dukelow SP, Brooks BL, Kirton A. Perilesional Gliosis Is Associated with Outcome after Perinatal Stroke. J Pediatr Neurol. 2021;19:321-329. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Zhang H, Rzechorzek W, Aghajanian A, Faber JE. Hypoxia induces de novo formation of cerebral collaterals and lessens the severity of ischemic stroke. J Cereb Blood Flow Metab. 2020;40:1806-1822. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 17. | Saida FB, Chaker J, Khedija S, Mouna B, Nadia A, Amine J, Mami A, Ariana H, Fatma B. A Rare Vascular Complication in a COVID-19 Patient: A Case Report of Free-Floating Carotid Thrombus. J Surg Res Prac. 2022;3:1-6. [DOI] [Full Text] |
| 18. | Chiu TL, Baskaran R, Tsai ST, Huang CY, Chuang MH, Syu WS, Harn HJ, Lin YC, Chen CH, Huang PC, Wang YF, Chuang CH, Lin PC, Lin SZ. Intracerebral transplantation of autologous adipose-derived stem cells for chronic ischemic stroke: A phase I study. J Tissue Eng Regen Med. 2022;16:3-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Oh JH, Kim W, Kim JY, Rhee YG. Outcomes of Rotator Cuff Repair in Patients with Comorbid Disability in the Extremities. Clin Orthop Surg. 2017;9:77-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Specchio N, Wirrell EC, Scheffer IE, Nabbout R, Riney K, Samia P, Guerreiro M, Gwer S, Zuberi SM, Wilmshurst JM, Yozawitz E, Pressler R, Hirsch E, Wiebe S, Cross HJ, Perucca E, Moshé SL, Tinuper P, Auvin S. International League Against Epilepsy classification and definition of epilepsy syndromes with onset in childhood: Position paper by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022;63:1398-1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 697] [Cited by in RCA: 598] [Article Influence: 149.5] [Reference Citation Analysis (0)] |
| 21. | Nam C, Rong W, Li W, Cheung C, Ngai W, Cheung T, Pang M, Li L, Hu J, Wai H, Hu X. An Exoneuromusculoskeleton for Self-Help Upper Limb Rehabilitation After Stroke. Soft Robot. 2022;9:14-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 22. | Nemanich ST, Chen CY, Chen M, Zorn E, Mueller B, Peyton C, Elison JT, Stinear J, Rao R, Georgieff M, Menk J, Rudser K, Gillick B. Safety and Feasibility of Transcranial Magnetic Stimulation as an Exploratory Assessment of Corticospinal Connectivity in Infants After Perinatal Brain Injury: An Observational Study. Phys Ther. 2019;99:689-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Han C, Shao P, Li H, Shi R, Wang Y. Effects of Unilateral Intermediate Cervical Plexus Block on the Diaphragmatic Function in Patients Undergoing Unilateral Thyroidectomy: A Randomized Controlled Study. J Pain Res. 2022;15:2663-2672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 24. | Sharma S, Anand A, Garg D, Batra S, Mukherjee SB, Patra B, Aneja S. Use of the International League Against Epilepsy (ILAE) 1989, 2010, and 2017 Classification of Epilepsy in children in a low-resource setting: A hospital-based cross-sectional study. Epilepsia Open. 2020;5:397-405. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Strand N, D'Souza RS, Hagedorn JM, Pritzlaff S, Sayed D, Azeem N, Abd-Elsayed A, Escobar A, Huntoon MA, Lam CM, Deer TR. Evidence-Based Clinical Guidelines from the American Society of Pain and Neuroscience for the Use of Implantable Peripheral Nerve Stimulation in the Treatment of Chronic Pain. J Pain Res. 2022;15:2483-2504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 67] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Rehabilitation
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Higashi K, Japan; Nogueira ML, Brazil S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ju JL