Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3362
Peer-review started: March 6, 2023
First decision: March 24, 2023
Revised: April 3, 2023
Accepted: April 12, 2023
Article in press: April 12, 2023
Published online: May 16, 2023
Processing time: 71 Days and 0.1 Hours
Mucosa-associated lymphoid tissue (MALT) lymphoma is a distinct subtype of non-Hodgkin B cell lymphoma that mostly involves the gastrointestinal tract. The stomach is the most commonly affected site whereas colorectal involvement occurs very rarely. Given its rarity, the management and clinical outcome of colorectal MALT lymphoma are not well established yet.
From the superficial capillary bed in the lower rectum. Endoscopic ultrasonography showed homogenous hypoechoic lesions in the deep mucosal layer. Endoscopic submucosal dissection (ESD) was done for accurate histologic diagnosis and treatment and both the rectal lesions were completely removed en bloc and subsequently diagnosed as primary rectal MALT lymphoma. Herein, we report a case of primary rectal MALT lymphoma in a 68-year-old woman that was treated by only ESD, and the 12-month follow-up revealed no tumour recurrence.
These results of our case and previous reports suggest that endoscopic resection alone may be a feasible and safe treatment for primary colorectal MALT lymphoma and allows organ preservation.
Core Tip: Colorectal involvement of Mucosa-associated lymphoid tissue (MALT) lymphoma occurs rarely and the management of colorectal MALT lymphoma are not well established yet. We report a rare case of colorectal MALT lymphoma treated with endoscopic resection alone. To date, only six cases of primary colorectal MALT lymphomas treated with endoscopic resection alone, including our patient, have been documented in the medical literature. Among the reported cases, there was no recurrence during follow-up. These results of our case and previous reports suggest that endoscopic resection alone may be a feasible and safe treatment for primary colorectal MALT lymphoma and allows organ preservation.
- Citation: Lee WS, Noh MG, Joo YE. Primary rectal mucosa-associated lymphoid tissue lymphoma treated with only endoscopic submucosal dissection: A case report. World J Clin Cases 2023; 11(14): 3362-3368
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3362.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3362
Gastrointestinal lymphoma is an uncommon disease that constitutes a small proportion of gastrointestinal neoplasms. Primary gastrointestinal mucosa-associated lymphoid tissue (MALT) lymphoma is a rare type of non-Hodgkin lymphoma that comprises 1%-4% of gastrointestinal non-Hodgkin lymphomas[1-3]. Most primary gastrointestinal MALT lymphomas occur in the stomach, and colorectal involvement occurs very rarely. Thus, the management and clinical outcome of colorectal MALT lymphoma are highly variable and not well established[4-7].
Here, we report a case of a 68-year-old woman with primary rectal MALT lymphoma that was treated with endoscopic submucosal dissection (ESD) alone and present a literature review pertaining to this condition.
A 68-year-old woman visited our clinic for a routine health screening examination.
She had no systemic B symptoms, including abdominal pain, fever, night sweats, and weight loss.
Ten years earlier, she underwent surgery for thyroid cancer. She had been on medication for hypertension and diabetes mellitus for 15 years.
The patient denied any family history of malignant tumours.
On physical examination, she was afebrile, her blood pressure and pulse were normal, and her abdomen was soft, nondistended, and nontender without hepatosplenomegaly or palpable lymphadenopathy.
Laboratory examinations, including complete blood cell count, liver function test, renal function study, and tumour markers, were within normal limits.
Computed tomography scan of the neck, chest, abdomen, and pelvis as well as bone marrow aspiration revealed no significant abnormalities.
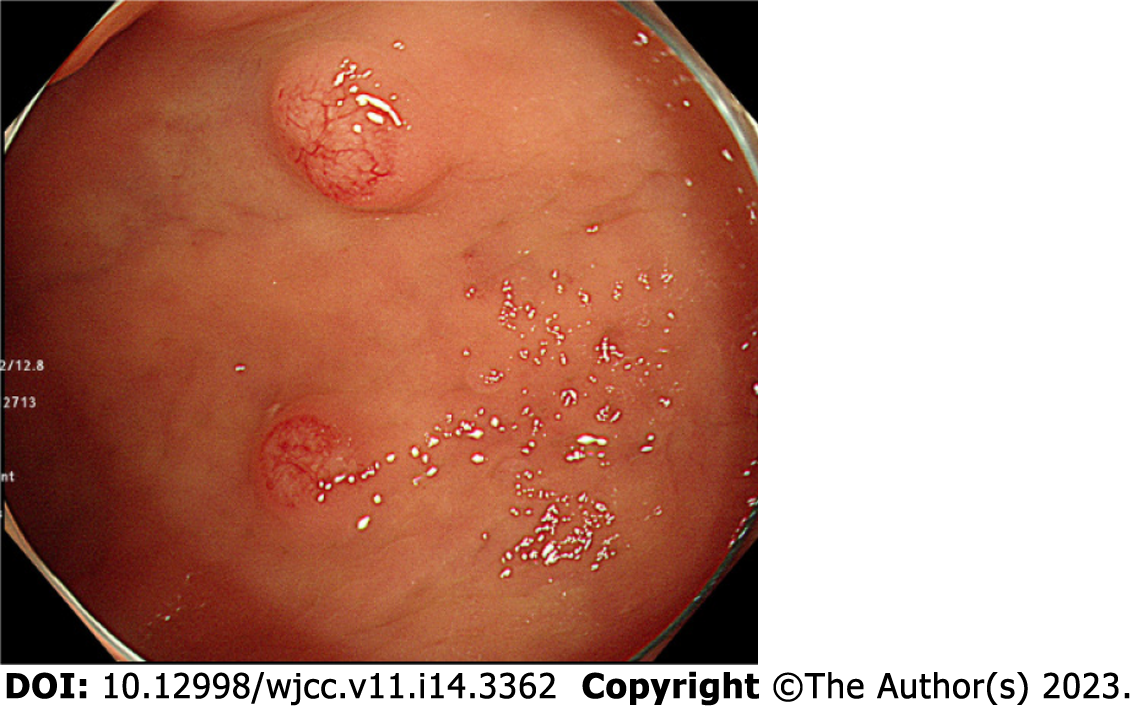
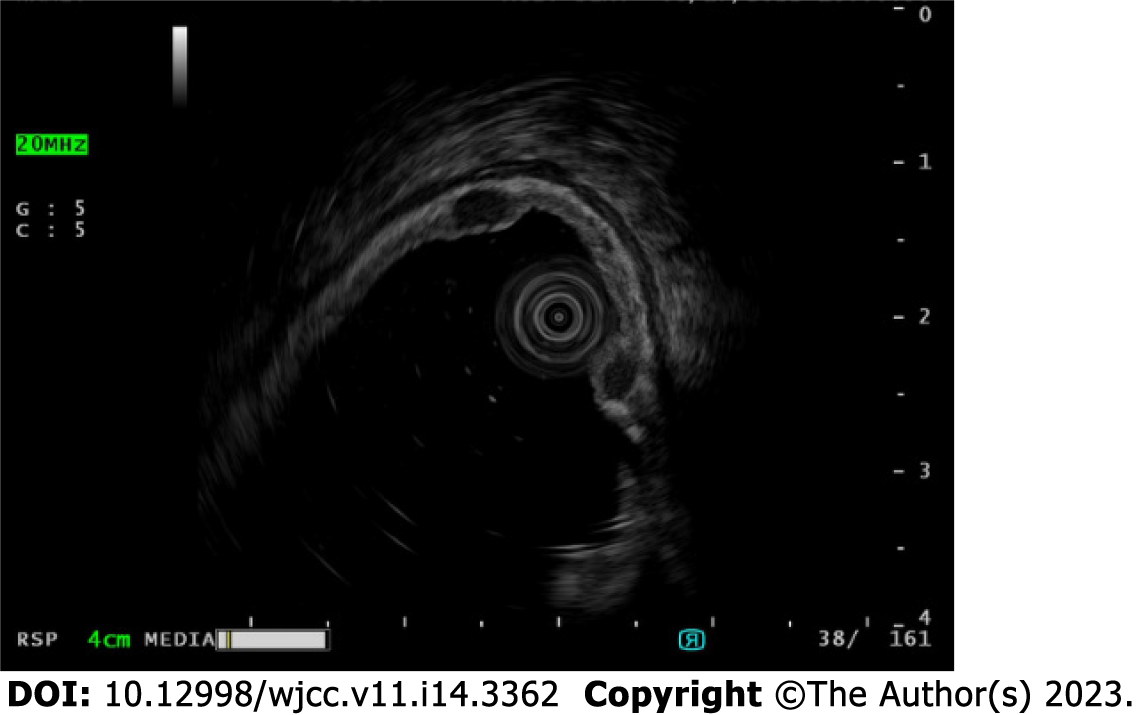
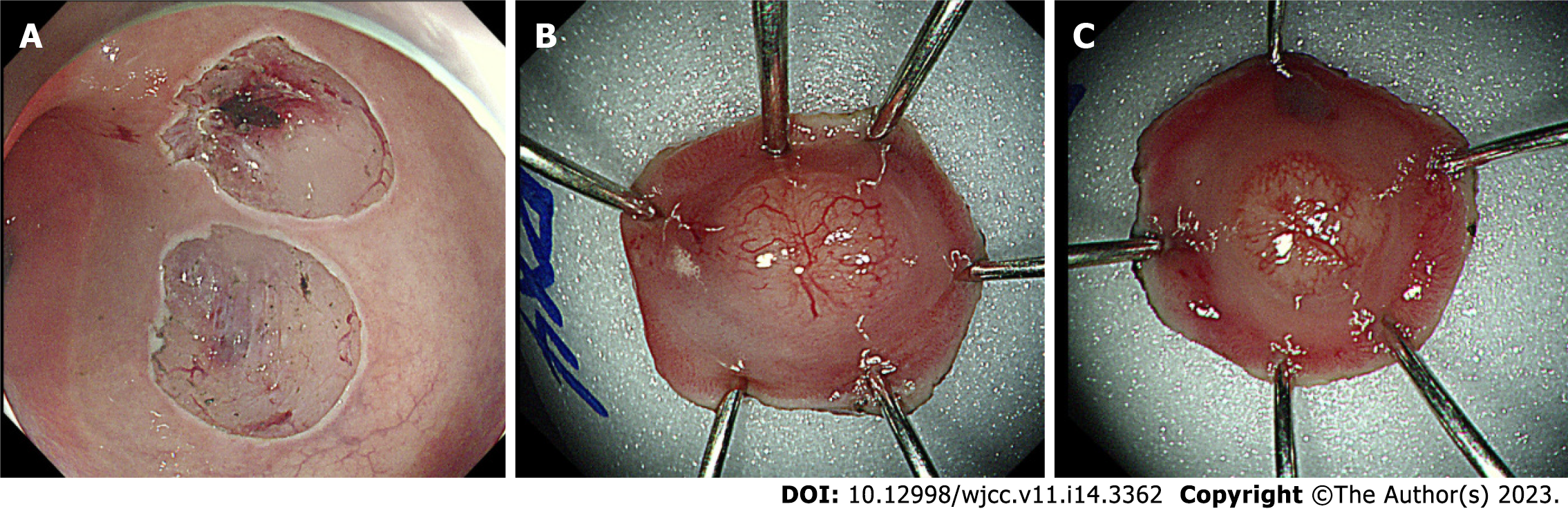
Esophagogastroduodenoscopy showed atrophic gastritis with intestinal metaplasia, and the Campylobacter-like organism test was negative for Helicobacter pylori (H. pylori) infection and the patient didn’t have history of previous H. pylori eradication therapy. Colonoscopy showed two subepithelial tumours, measuring 4 and 5 mm and arising from the superficial capillary bed into the lower rectum (Figure 1), that seemed to be neuroendocrine tumours. Endoscopic ultrasonography revealed two homogenous hypoechoic lesions in the deep mucosal layer (Figure 2). As rectal neuroendocrine tumor was suspected according to the endoscopic ultrasonography, the two rectal lesions were removed en bloc via ESD for accurate histological diagnosis and treatment (Figure 3).
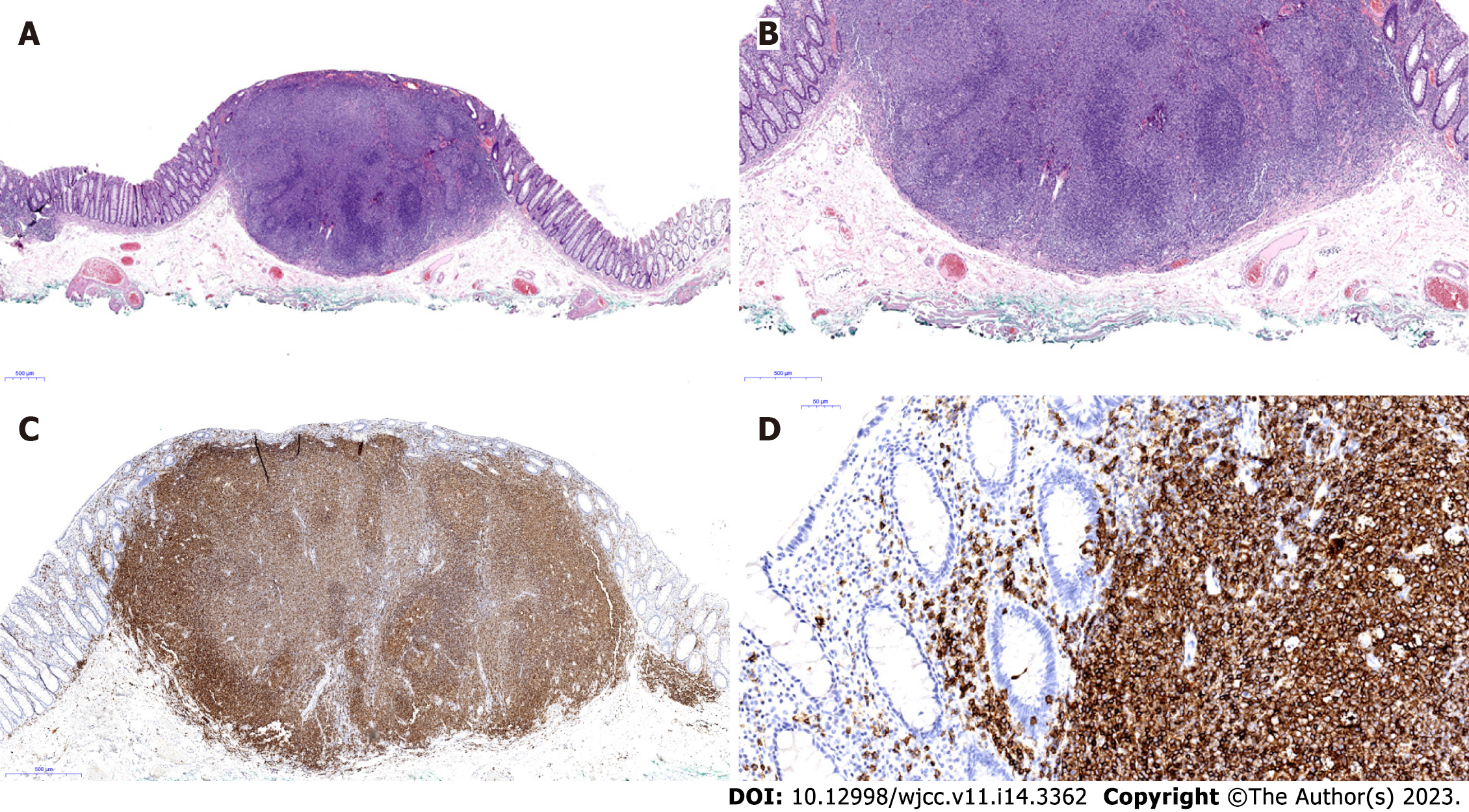
On routine histology, haematoxylin–eosin staining showed a dense aggregate of lymphoid cell in the lamina propria layer forming polypoid-lesion (Figure 4A). These lymphoid cells that had small-to-intermediate nuclei and focally clear cytoplasm, infiltrated into muscularis mucosae but did not infiltrate into submucosa (Figure 4B). Immunohistochemistry to ascertain the nature of tumour cells showed positive staining for CD20 (Figure 4C), but negative results for CD3 and Bcl-6. The Ki-67 Labelling index was 5%. Characteristic lymphocyte-epithelial infiltration of CD20-positive tumor cells was also observed (Figure 4D). The biopsy specimens indicated a diagnosis of MALT lymphoma. In accordance with the Ann Arbor staging system, the tumour was diagnosed as a stage IE primary rectal MALT lymphoma.
The two rectal lesions were removed en bloc via ESD.
The patient has been followed-up regularly at the outpatient clinic. Although follow-up period of the patient has been only 12 mo, there was no evidence of recurrence at 12 mo after the ESD.
MALT lymphoma is classified as an extranodal marginal zone B-cell lymphoma of the MALT type[1-3] that frequently involves the gastrointestinal tract, including stomach and small bowel, and very rarely involves the colorectal structures[4-7]. Therefore, the clinical characteristics, treatment, and outcome of primary colorectal MALT lymphoma have not been clearly established yet.
The median age at diagnosis of colorectal MALT lymphoma is approximately 60 years, with a slight female predisposition, and the clinical presentation is most often asymptomatic, followed by abdominal discomfort/pain, positive result on a stool occult blood test, constipation, diarrhoea, tenesmus, and obstruction. The most common lesion site is the rectum, followed by the terminal ileum, cecum, and sigmoid colon. The main endoscopic appearance is of a subepithelial tumour, followed by polyposis, ileitis, and epithelial mass type[7]. Our patient is a 68-year-old woman with an asymptomatic rectal MALT lymphoma that comprised two subepithelial tumours that were found incidentally on screening colonoscopy.
Gastric MALT lymphoma is strongly associated with H. pylori infection, and H. pylori eradication is the main therapeutic strategy in primary gastric MALT lymphoma[1-3]. However, the association between colorectal MALT lymphoma and H. pylori infection is unclear. In our patient, the rectal MALT lymphoma was not associated with an H. pylori infection.
Colorectal MALT lymphomas were treated by various modalities, including single or a combination of endoscopic resection, surgery, H. pylori eradication with antibiotics, radiation therapy, or chemotherapy. The overall prognosis of colonic MALT lymphoma showed an indolent nature and favourable clinical behaviour[4-7]. However, because of its rarity and indolent nature, the treatment and outcome of colorectal MALT lymphoma is not well established.
In our case, ESD was undertaken for accurate histological diagnosis and treatment. Rectal lesions were completely resected en bloc by ESD and were pathologically confirmed as a rectal MALT lymphoma. Given the stage IE status of lesions limited to only the rectum, based on a discussion with our multidisciplinary medical team, observation without additional treatment was planned. Twelve months after the ESD, the patient had no tumour recurrence.
The first case of endoscopic resection with a hot-snare guillotine technique was reported in primary rectal MALT lymphoma in 2009, wherein empirical H. pylori eradication therapy was added despite a negative result on the H. pylori test[8]. Another case of stage IE primary rectal MALT lymphoma was diagnosed by endoscopic mucosal resection (EMR) and treated with radiation therapy[9].
To date, only six cases of primary colorectal MALT lymphomas treated with endoscopic resection alone, including our patient, have been documented in the medical literature (Table 1)[10-14]. The patients were aged 46 to 72 years (mean age, 64.2 years) and included three men and three women. On clinical presentation, three cases were asymptomatic, two had bleeding, and one had weight loss. Two cases are treated with EMR, two with ESD, one with EMR with ligation, and one with endoscopic full-thickness resection. The mean follow-up period was 30.2 mo (range, 12–60 mo). Among the reported cases, there was no recurrence during follow-up.
| Patient No. | Ref. | Age (yr)/Sex | Symptoms (duration) | Location | Size (cm) | Endoscopic findings | Treatment | Follow up period (mo) | Outcome |
| 1 | Lin et al[10], 2016 | 59/M | Positive fecal occult blood test | Colon (25 cm from anal verge) | 2.0 | Polypoid lesion with wide base, slightly irregular border, and an irregular vascular pattern with mild inflammatory changes | EMR | 36 | No recurrence |
| 2 | Shah et al[11], 2021 | 72/M | Asymptomatic | Mid rectum | 2.0 | Raised erythematous lesion | EMR | 60 | No recurrence |
| 3 | Yoon et al[12],2021 | 69/F | Weight loss (3 mo) | Lower rectum | 1.0 | Subepithelial tumor | EMR with ligation | 37 | No recurrence |
| 4 | Tao et al[13],2022 | 46/M | Asymptomatic | Rectum (10 cm from anal verge) | 3.5 | Laterally spreading tumor-like lesion | ESD | 24 | No recurrence |
| 5 | Li et al[14], 2022 | 71/F | Hematochezia (1 mo) | Lower rectum | 6.0 | Hemispheric mass with rough and hyperemic mucosa | Endoscopic full-thickness resection | 12 | No recurrence |
| 6 | Present case | 68/F | Asymptomatic | Lower rectum | 0.5, 0.3 | Two subepithelial tumors with superficial capillary bed | ESD | 12 | No recurrence |
These results of our case and previous reports suggest that endoscopic resection alone may be a feasible and safe treatment for primary colorectal MALT lymphoma and allows organ preservation. However, long-term follow-up data are needed to determine the efficacy of this treatment approach in a larger number of cases that have been treated with endoscopic resection alone.
| 1. | Violeta Filip P, Cuciureanu D, Sorina Diaconu L, Maria Vladareanu A, Silvia Pop C. MALT lymphoma: epidemiology, clinical diagnosis and treatment. J Med Life. 2018;11:187-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 82] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 2. | Thieblemont C, Zucca E. Clinical aspects and therapy of gastrointestinal MALT lymphoma. Best Pract Res Clin Haematol. 2017;30:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Ishikawa E, Nakamura M, Satou A, Shimada K, Nakamura S. Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma in the Gastrointestinal Tract in the Modern Era. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Hollie N, Asakrah S. MALT lymphoma of the colon: a clinicopathological review. J Clin Pathol. 2020;73:378-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Won JH, Kim SM, Kim JW, Park JH, Kim JY. Clinical features, treatment and outcomes of colorectal mucosa-associated lymphoid tissue (MALT) lymphoma: literature reviews published in English between 1993 and 2017. Cancer Manag Res. 2019;11:8577-8587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Tannoury J, Amiot A, Lemonnier F, Dupuis J, Gagnière C, Belhadj K, Bras FL, Sobhani I, Haioun C, Copie-Bergman C, Lévy M. Colonic mucosa-associated lymphoid tissue lymphoma: a case series. Leuk Lymphoma. 2020;61:582-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Jeon MK, So H, Huh J, Hwang HS, Hwang SW, Park SH, Yang DH, Choi KD, Ye BD, Myung SJ, Yang SK, Byeon JS. Endoscopic features and clinical outcomes of colorectal mucosa-associated lymphoid tissue lymphoma. Gastrointest Endosc. 2018;87:529-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Mathew A, Humburg BC, Bayer MG. A case of rectal MALT lymphoma treated by endoscopic resection. Am J Gastroenterol. 2009;104:255-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Hayakawa T, Nonaka T, Mizoguchi N, Hagiwara Y, Shibata S, Sakai R, Nakayama N, Yokose T, Nakayama Y. Radiotherapy for mucosa-associated lymphoid tissue (MALT) lymphoma of the rectum: a case report. Clin J Gastroenterol. 2017;10:431-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Lin PC, Chen JS, Deng P, Wang CW, Huang CH, Tang R, Chiang JM, Yeh CY, Hsieh PS, Tsai WS, Chiang SF. Concurrent colonic mucosa-associated lymphoid tissue lymphoma and adenoma diagnosed after a positive fecal occult blood test: a case report. J Med Case Rep. 2016;10:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Shah RM, Kuo V, Schwartz A. Endoscopic mucosal resection and cure for rectal mucosa-associated lymphoid tissue lymphoma. Proc (Bayl Univ Med Cent). 2020;34:305-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Yoon BH, Huh CW. [Rectal Mucosa-associated Lymphoid Tissue Lymphoma Treated with Endoscopic Resection]. Korean J Gastroenterol. 2021;78:344-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 13. | Tao Y, Nan Q, Lei Z, Miao YL, Niu JK. Rare primary rectal mucosa-associated lymphoid tissue lymphoma with curative resection by endoscopic submucosal dissection: A case report and review of literature. World J Clin Cases. 2022;10:7599-7608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Li FY, Zhang XL, Zhang QD, Wang YH. Successful treatment of an enormous rectal mucosa-associated lymphoid tissue lymphoma by endoscopic full-thickness resection: A case report. World J Gastroenterol. 2022;28:1078-1084. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li XB, China; Osawa S, Japan; Sugimoto M, Japan S-Editor: Ma YJ L-Editor: A P-Editor: Zhao S