Published online May 6, 2023. doi: 10.12998/wjcc.v11.i13.3070
Peer-review started: January 31, 2023
First decision: February 17, 2023
Revised: March 1, 2023
Accepted: April 4, 2023
Article in press: April 4, 2023
Published online: May 6, 2023
Processing time: 83 Days and 17.4 Hours
Sealed perforation of colonic diverticulum is a common clinical condition and may be differentiated from an underlying malignant perforation using interval endoscopy. We present an uncommon colonoscopy finding of a healed diver
A middle-aged Chinese female presented with a 3-d history of non-colicky left iliac fossa pain. It was associated with fever (Tmax 37.6 ºC), non-bloody diarrhoea and non-bloody, non-bilious vomiting. She had a history of Type 2 diabetes mellitus, well controlled on metformin. Tenderness was noted on the left iliac fossa region with no guarding or mass. Total white cell count (11.45 × 109/L) and C-reactive protein levels (213.9 mg/L) were elevated. Computed tomography imaging of the abdomen revealed pericolonic fat stranding and extraluminal air pockets fluid density with peritoneal thickening at the sigmoid colon, likely representing a sealed perforation. Six weeks after the episode, she underwent a follow-up colonoscopy. An exophytic polypoid lesion closely associated with a diverticulum was seen in the sigmoid colon. The lesion was easily “pinched” off without much effort using endoscopic forceps and sent for histology which revealed granulation tissue suggesting a healed diverticular perforation.
Granulation tissue associated with healed diverticular perforations resemble polyps. Tattooing around these sites may allow for future targeted colonic resections.
Core Tip: This case report aims to shed light on the possible morphology of a healed diverticular perforation. This is important as patients who have suffered from diverticular perforations are at increased risk of recurrence, with high likelihood of the previously perforated diverticulum being the offending cause. Recognising the appearance of granulation tissue from a possible sealed perforated diverticulum and marking the site with injectable tattoos may allow for targeted resections of the colon if recurrence occurs. This preserves more parenchyma, allows for a potentially faster surgery, and shortens recovery time while achieving an equivalent improvement in quality-of-life.
- Citation: Liew JJL, Lim WS, Koh FH. Unusual phenomenon-“polyp” arising from a diverticulum: A case report. World J Clin Cases 2023; 11(13): 3070-3075
- URL: https://www.wjgnet.com/2307-8960/full/v11/i13/3070.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i13.3070
Diverticular disease is a common benign condition defined by the outpouching of all layers of the intestinal mucosa[1]. Diverticular disease of the colon is common in industrialised countries. The prevalence of diverticular disease is similar in men and women. However, the prevalence of diverticular disease increases with age, ranging from 10% in those younger than 40 to 50 years old, to 70% in those above 80 years of age[2-4]. The anatomic distribution of diverticular disease also varies geographically. In the west, diverticuli are commonly limited to the sigmoid colon in 65%, sigmoid plus other colonic diverticuli in 25%, pan colonic diveritculi in 7%, and diverticuli isolated to a segment proximal to the sigmoid colon in 4% of patients[5]. Conversely, in the East, in Asian populations, the anatomic distribution is different and primarily involves the right colon with a prevalence rate of 13% to 25%[6-9].
Perforation of diverticulitis occurs secondary to bowel wall inflammation, subsequent necrosis and the loss of intestinal wall integrity. The principles for the management of diverticular perforations are dependent on the nature of the perforation. Sealed perforations are treated conservatively with antibiotics while frank and free perforations are treated surgically. Surgical management of perforated diverticuli, for instance the Hartmann Procedure, often results in stoma creation, which reduces a patient’s quality-of-life[10]. Another complication of surgical management is diarrhoea caused by reduced storage capacity in the colon from extensive colonic resection in view of the inability to identify specific perforation sites. Management for a perforated diverticulitis with peritonitis is highly controversial owing to the lack of high quality data backing management options for personalised surgery[11]. Elective segmental colonic resections are commonly performed, as evidenced by an 8% risk of recurrence in one year, and a 20% risk of recurrence within ten years of patients with resolved acute diverticulitis. Nonetheless, routine follow-up colonoscopies post-acute diverticulitis episodes have a role to play in holistic patient care.
To date, the endoscopic morphology of a healed diverticular perforations has not been documented in literature.
This case report aims to educate clinical endoscopists on how to identify healed diverticular perforations. Our aim is to eventually revolutionise the presently practised elective segmental colonic resection, which is indicated in recurrent or complicated diverticulitis, by encouraging parenchymal-sparing surgeries through the demarcation of past perforation sites.
In this paper, we report about a middle-aged Chinese female who presented for a routine follow-up colonoscopy 6 wk after an episode of acute diverticulitis. Novel colonoscopy findings of the site of perforation is described in this report. These colonoscopy findings were confirmed by histology which showed granulation tissue, indicating an ongoing healing process.
A middle-age Chinese lady initially presented with a 3-d history of constant abdominal pain in the left iliac fossa.
This was associated with a fever of Tmax 37.6ºC, non-bloody diarrhoea, and non-bloody, non-bilious vomiting.
She had a past medical history of Type 2 diabetes mellitus which was well controlled on 850 mg Metformin thrice a day.
Family history was unremarkable for gastrointestinal malignancy. She was a non-smoker and non-drinker.
Physical examination on initial presentation for acute diverticulitis revealed tenderness on the left flank with no guarding. Otherwise, physical examination was unremarkable. There were no signs of chronic liver disease-no jaundice, caput medusae, scleral icterus, Dupuytren’s contractures, clubbing, hepatic asterixis, gynaecomastia, spider naevi, shifting dullness or pedal oedema. There are no signs of anaemia-no conjunctival pallor, no palmar crease pallor. There were no signs pointing to any kidney pathology-no renal bruits and kidneys were non-ballotable. There was no hepatomegaly or splenomegaly. Bowel sounds were active.
Laboratory investigations revealed elevated C-reactive protein levels (213.9 mg/L) and white cell count (11.45 × 109/L).
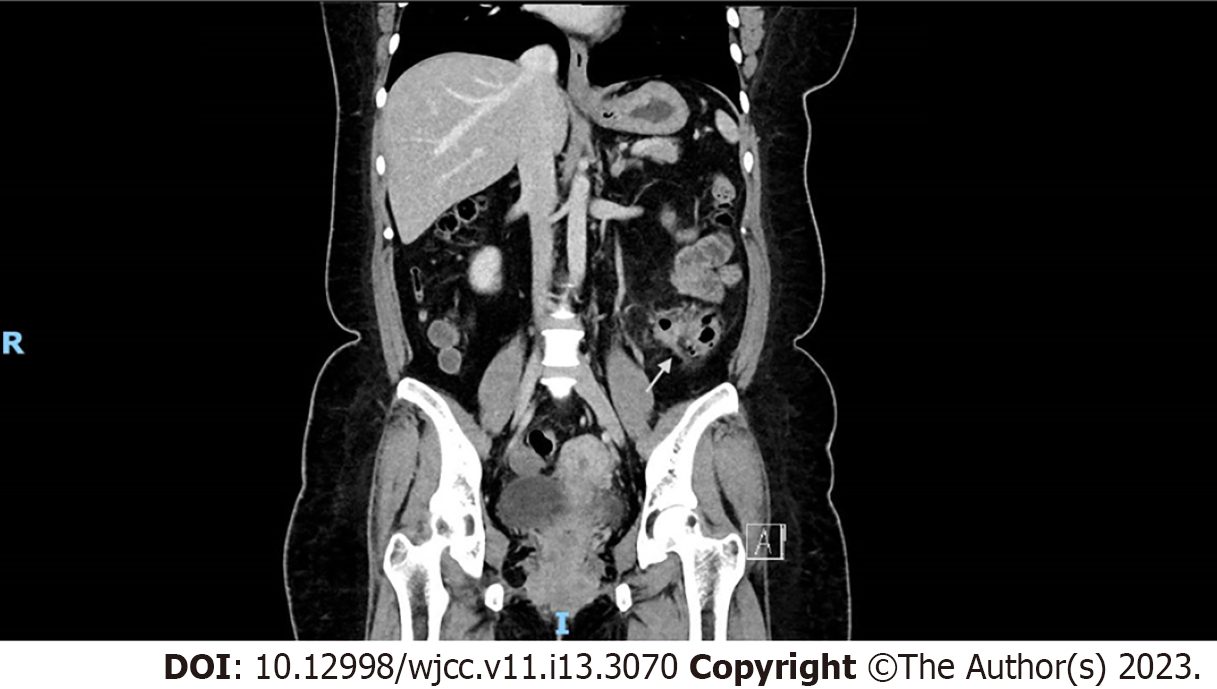
On a computed tomography scan of the abdomen, a confined pericolic abscess was seen (Figure 1).
This confirmed the presence of a Modified Hinchey Ib diverticulitis.
It was managed conservatively with the following course of antibiotics for 5 d–IV ceftriaxone 2 g once a day, and IV metronidazole 500 mg thrice a day. Subsequently, the patient was started on oral co-amoxiclav for a total of 4 wk.
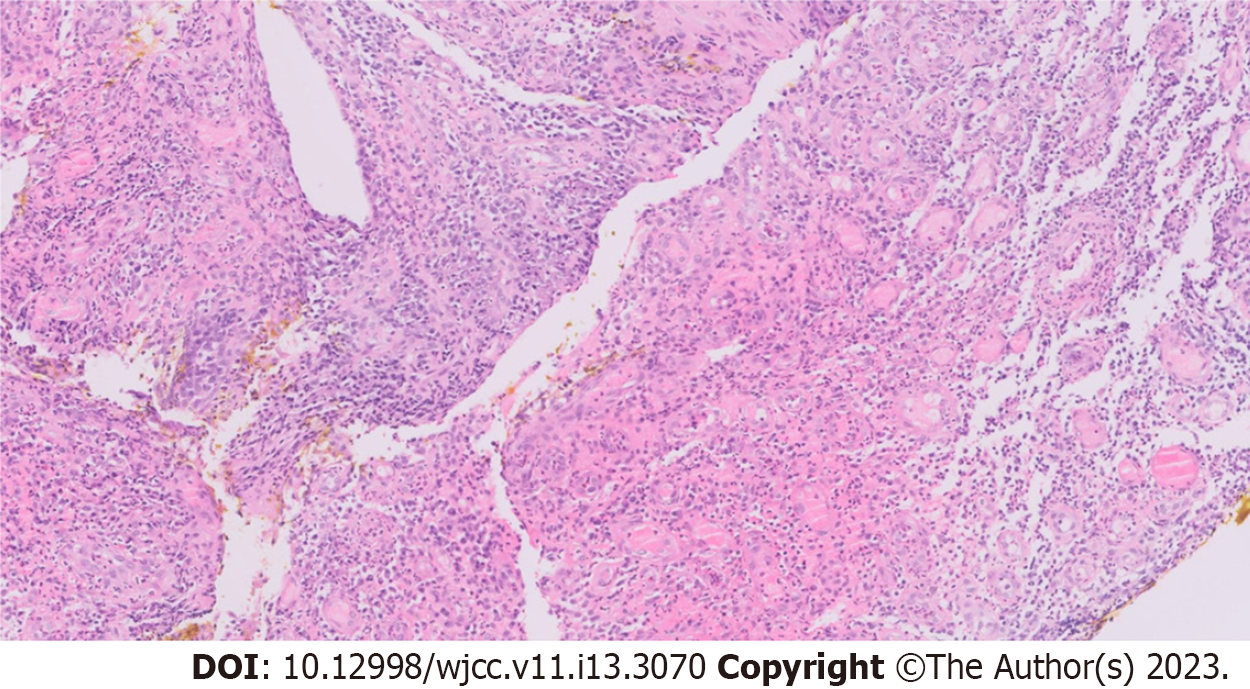
Interval follow-up colonoscopy 6 wk after the acute event revealed polyps in the sigmoid colon. One of the lesions, which was in close proximity to a diverticulum (Figure 2), was easily “pinched” off using endoscopic forceps and sent for histology, revealing an abundance of fibroblasts, keratinocytes, and endothelial cells, characteristic of granulation tissue and consistent with healing (Figure 3)[12]. Neither tubular, nor villous growth patterns were noted, ruling out a diagnosis of adenomatous polyps. Therefore, the “polyp” likely represented the previous site of diverticular perforation.
Currently there is limited literature on the appearance and possible morphologies of healed diverticular perforations. Therefore, with this case report we hope to provide an insight into how healed diverticular perforations may appear. Current literature focuses primarily on the pathophysiology, risk factors, along with the possible acute management methods of a diverticular perforation, and not its endoscopic morphology. Furthermore, reports on the endoscopic appearance of diverticular disease largely play the role of clinching the diagnosis of diverticular disease[13] as opposed to studying the possible different morphologies of diverticular disease, particularly after an episode of perforated diverticulitis. Of those that have described the endoscopic appearance of diverticular disease, some have elaborated on the possible histopathologic resemblance between the non-diverticular mucosa in such patients and other mucosal diseases like Crohn’s disease or ulcerative colitis[14,15]. Therefore, to the best of our knowledge, the presented case is the first in literature to report the development of polyp-resembling granulation tissue at the site of a previous diverticular perforation. This can potentially offer an alternative angle of management of such sealed perforations.
The rate of recurrence of diverticulitis remains relatively modest, Broderick-Villa et al[16] reported on 2366 of 3165 patients (75%) hospitalized with acute diverticulitis and treated nonoperatively in the Kaiser Permanente system. Eighty-six percent of those patients required no further inpatient care for diverticulitis over the 8.9 years of follow-up. Recurrence occurred in only 13.3% of patients and only 3.9% had a second recurrence[17]. Moreover, recurrence of diverticulitis is greater after an episode of complicated diverticulitis at 24%, as opposed to after an episode of uncomplicated diverticulitis at 23.4%[18]. Ultimately, the authors concluded that recurrence overall is rare and there is therefore a decreasing need for elective colectomies following episodes of diverticulitis[19]. However, if a recurrence were to happen often enough, according to the American Society of Gastrointestinal Endoscopy, surgical resection of the offending site of recurrent diverticulitis is recommended[20]. As the actual offending diverticulum is often not identified, anatomical resection of segments of the colon is performed, which leads to significant amount of colonic length loss which may have implications on quality of life for these patients.
The utility of colonic mucosal tattoo placements lies in marking lesions for subsequent surgical resection, for later endoscopic resection, or to mark an endoscopic resection site for easy endoscopic follow-up of the resection site[21]. We propose the utility of such a mucosal tattoo to mark the potential site of a healed diverticular perforation, if successfully identified. This can potentially help guide surgical resection when the need arises with a more targeted resection. In this way, colonic length can potentially be spared to maintain quality-of-life for the affected patients. A proposal of this nature, when supported by further prospective data and larger series, can potentially modify the way we treat recurrent complicated diverticulitis.
This case report displays the morphology of granulation tissue associated with healed diverticular perforations on colonoscopy. This serves to guide endoscopists during colonoscopy to help identify sites of recent perforations. Nonetheless, biopsies of lesions resembling our findings should still be taken, to rule out other pathologies. Tattoo placements may guide clinical treatment by allowing for more targeted colonic resections in the event of recurrence of complicated diverticulitis at the same location. From our preliminary glimpse into the description of the morphology of healed perforated diverticulum, further studies may be conducted to broaden our understanding of the topic.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bustamante-Lopez LA, Brazil; Zhang G, China; Zhao S, China S-Editor: Hu YR L-Editor: A P-Editor: Zhao S
| 1. | Linzay CD, Pandit S. Acute Diverticulitis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459316/. |
| 2. | Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 316] [Article Influence: 16.6] [Reference Citation Analysis (1)] |
| 3. | Ferzoco LB, Raptopoulos V, Silen W. Acute diverticulitis. N Engl J Med. 1998;338:1521-1526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 201] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | Tursi A. Acute diverticulitis of the colon--current medical therapeutic management. Expert Opin Pharmacother. 2004;5:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Parks TG. Natural history of diverticular disease of the colon. Clin Gastroenterol. 1975;4:53-69. [PubMed] |
| 6. | Ngoi SS, Chia J, Goh MY, Sim E, Rauff A. Surgical management of right colon diverticulitis. Dis Colon Rectum. 1992;35:799-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Wang FW, Chuang HY, Tu MS, King TM, Wang JH, Hsu CW, Hsu PI, Chen WC. Prevalence and risk factors of asymptomatic colorectal diverticulosis in Taiwan. BMC Gastroenterol. 2015;15:40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Markham NI, Li AK. Diverticulitis of the right colon--experience from Hong Kong. Gut. 1992;33:547-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 68] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Chan CC, Lo KK, Chung EC, Lo SS, Hon TY. Colonic diverticulosis in Hong Kong: distribution pattern and clinical significance. Clin Radiol. 1998;53:842-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 10. | Moro-Valdezate D, Royo-Aznar A, Martín-Arévalo J, Pla-Martí V, García-Botello S, León-Espinoza C, Fernández-Moreno MC, Espín-Basany E, Espí-Macías A. Outcomes of Hartmann's procedure and subsequent intestinal restoration. Which patients are most likely to undergo reversal? Am J Surg. 2019;218:918-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Nascimbeni R, Amato A, Cirocchi R, Serventi A, Laghi A, Bellini M, Tellan G, Zago M, Scarpignato C, Binda GA. Management of perforated diverticulitis with generalized peritonitis. A multidisciplinary review and position paper. Tech Coloproctol. 2021;25:153-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Reinke JM, Sorg H. Wound repair and regeneration. Eur Surg Res. 2012;49:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 937] [Cited by in RCA: 1256] [Article Influence: 89.7] [Reference Citation Analysis (0)] |
| 13. | Kim YS. [Diagnosis and Treatment of Colonic Diverticular Disease]. Korean J Gastroenterol. 2022;79:233-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 14. | West AB, Losada M. The pathology of diverticulosis coli. J Clin Gastroenterol. 2004;38:S11-S16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 15. | Weizman AV, Nguyen GC. Diverticular disease: epidemiology and management. Can J Gastroenterol. 2011;25:385-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 200] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 16. | Broderick-Villa G, Burchette RJ, Collins JC, Abbas MA, Haigh PI. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-81; discussion 581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 178] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 17. | Rai V, Mishra N. Surgical Management of Recurrent Uncomplicated Diverticulitis. Clin Colon Rectal Surg. 2021;34:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (1)] |
| 18. | Eglinton T, Nguyen T, Raniga S, Dixon L, Dobbs B, Frizelle FA. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97:952-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Morris AM, Regenbogen SE, Hardiman KM, Hendren S. Sigmoid diverticulitis: a systematic review. JAMA. 2014;311:287-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 133] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 20. | Qaseem A, Etxeandia-Ikobaltzeta I, Lin JS, Fitterman N, Shamliyan T, Wilt TJ; Clinical Guidelines Committee of the American College of Physicians*, Crandall CJ, Cooney TG, Cross JT Jr, Hicks LA, Maroto M, Mustafa RA, Obley AJ, Owens DK, Tice J, Williams JW Jr; Clinical Guidelines Committee of the American College of Physicians. Colonoscopy for Diagnostic Evaluation and Interventions to Prevent Recurrence After Acute Left-Sided Colonic Diverticulitis: A Clinical Guideline From the American College of Physicians. Ann Intern Med. 2022;175:416-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Rex DK. The Appropriate Use and Techniques of Tattooing in the Colon. Gastroenterol Hepatol (N Y). 2018;14:314-317. [PubMed] |