Published online May 6, 2023. doi: 10.12998/wjcc.v11.i13.3045
Peer-review started: November 16, 2022
First decision: January 12, 2023
Revised: February 15, 2023
Accepted: March 21, 2023
Article in press: March 21, 2023
Published online: May 6, 2023
Processing time: 160 Days and 2.9 Hours
The fractional flow reserve (FFR) has made the treatment of coronary heart disease more precise. However, there are few reports on the measurement of FFR via the left internal mammary artery (LIMA). Herein, we described the determination of further treatments by measuring FFR via the LIMA in 2 cases after coronary artery bypass grafting (CABG).
Case 1 was a 66-year-old male who was admitted due to “chest tightness after CABG.” The patient underwent CABG 7 years prior due to coronary heart disease. Coronary artery angiography showed complete occlusion of the left anterior descending artery (LAD), and subtotal occlusion of the third segment of the right coronary artery. On arterial angiography, there was 85% stenosis at the distal end of the anastomosis of the LIMA-LAD graft. FFR via LIMA was determined at 0.75. Thus, balloon dilation was performed in Case 1. FFR after balloon dilation was 0.94. Case 2 was a 60-year-old male who was admitted due to “chest tightness after CABG.” The patient underwent CABG 6 years prior due to coronary heart disease. There was 60% segmental stenosis in the middle segment of LAD and 75% anastomotic stenosis. FFR measured via LIMA was 0.83 (negative); thus the intervention was not performed. Case 2 was given drug treatments. At the 3-mo follow-up, there was no recurrence of chest tightness or shortness of breath in both cases. They are currently under continual follow-up.
We provided evidence that FFR measurement via grafted blood vessels, especially LIMA, after CABG is a good method to determine the intervention course.
Core Tip: We reported the determination of intervention by fractional flow reserve value measured via the left internal mammary artery after coronary artery bypass grafting in 2 cases. We provided evidence that fractional flow reserve measurement via grafted blood vessels, especially the left internal mammary artery, after coronary artery bypass grafting is a good method to determine whether to intervene.
- Citation: Zhang LY, Gan YR, Wang YZ, Xie DX, Kou ZK, Kou XQ, Zhang YL, Li B, Mao R, Liang TX, Xie J, Jin JJ, Yang JM. Fractional flow reserve measured via left internal mammary artery after coronary artery bypass grafting: Two case reports. World J Clin Cases 2023; 11(13): 3045-3051
- URL: https://www.wjgnet.com/2307-8960/full/v11/i13/3045.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i13.3045
Coronary angiography can only perform anatomical evaluation of the stenosis degree and cannot functionally evaluate the effect of the stenosis on the distal blood flow or identify the extent of myocardial ischemia. This causes overestimation or underestimation of the lesion severity and results in over-treatment or under-treatment of lesions[1]. Fractional flow reserve (FFR), which was first proposed in 1993[2], is an index for estimating coronary blood flow by pressure measurement. In recent years, the wide application of FFR has enabled patients with coronary heart disease to receive precise treatment[3,4]. The left internal mammary artery (LIMA) has an excellent long-term patency rate and is the preferred vessel for coronary artery bypass grafting (CABG)[5]. However, the measurement of FFR via the LIMA is rarely reported. Herein, we reported the determination of further treatments in 2 patients by measuring FFR through the LIMA. These patients received CABG for coronary heart disease and had graft occlusion after CABG.
Case 1: A 66-year-old male was admitted to Gansu Institute of Cardiovascular Diseases due to “chest tightness after CABG.”
Case 2: A 60-year-old male was admitted to Gansu Institute of Cardiovascular Diseases because of “chest tightness after CABG.”
Case 1: The patient experienced intermittent chest tightness and shortness of breath in the prior 3 years. The symptoms worsened in the 3 mo prior to admission.
Case 2: The patient suffered from chest tightness and shortness of breath in the week prior to admission.
Case 1: The patient underwent CABG 7 years prior due to coronary heart disease. The coronary artery bypass grafts included the graft from LIMA to the left anterior descending artery (LAD), the graft from the ascending aorta (AO) to the right posterior descending coronary artery and the graft from the AO to the first diagonal branch of the left coronary artery.
Case 2: The patient received CABG 6 years prior due to coronary heart disease. The coronary artery bypass grafts included the LIMA-LAD graft and the saphenous vein-obtuse marginal branch graft.
Case 1: The patient denied any family history of heart disease or genetic disease. The patient had a smoking history of 30 years (3 cigarettes a day).
Case 2: The patient denied any family history of heart disease or genetic disease. The patient had a smoking history of 30 years (20 cigarettes a day).
Case 1: Physical examination showed blood pressure of 152/93 mmHg and heart rate of 61 beats/min. There was no arrhythmia or pathological murmur.
Case 2: Physical examination showed blood pressure of 135/85 mmHg and heart rate of 77 beats/min. No arrhythmia or pathological murmur was observed.
Case 1: Laboratory examinations showed that low density lipoprotein was 3.80 mmol/L, and total cholesterol was 5.70 mmol/L. No obvious abnormality was observed in other blood biochemical indicators.
Case 2: Laboratory examinations showed that low density lipoprotein was 2.06 mmol/L, and total cholesterol was 3.59 mmol/L. There was no obvious abnormality in other blood biochemical indicators.
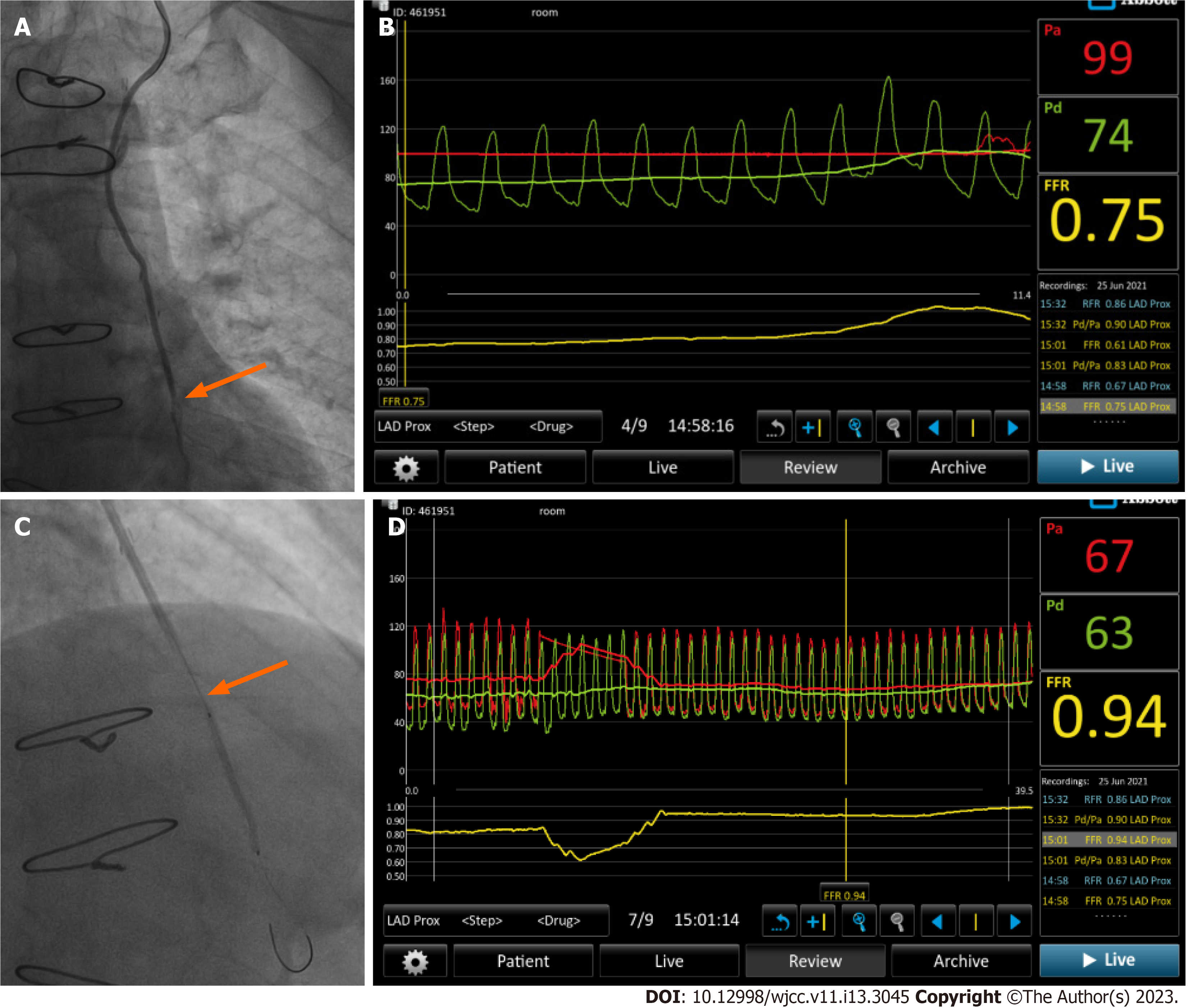
Case 1: Coronary artery angiography showed complete occlusion of LAD and subtotal occlusion of the third segment of the right coronary artery (RCA). The angiography also showed that the AO-first diagonal branch of the left coronary artery and the AO-posterior descending coronary artery grafts had smooth blood flow and had no anastomotic stenosis. On the arterial angiography, it was observed that the LIMA-LAD graft had smooth blood flow and had no anastomotic stenosis. However, there was 85% stenosis at the distal end of the anastomosis of the LIMA-LAD graft (Figure 1A). Cardiac ultrasound showed that the left ventricular ejection fraction was 54%.
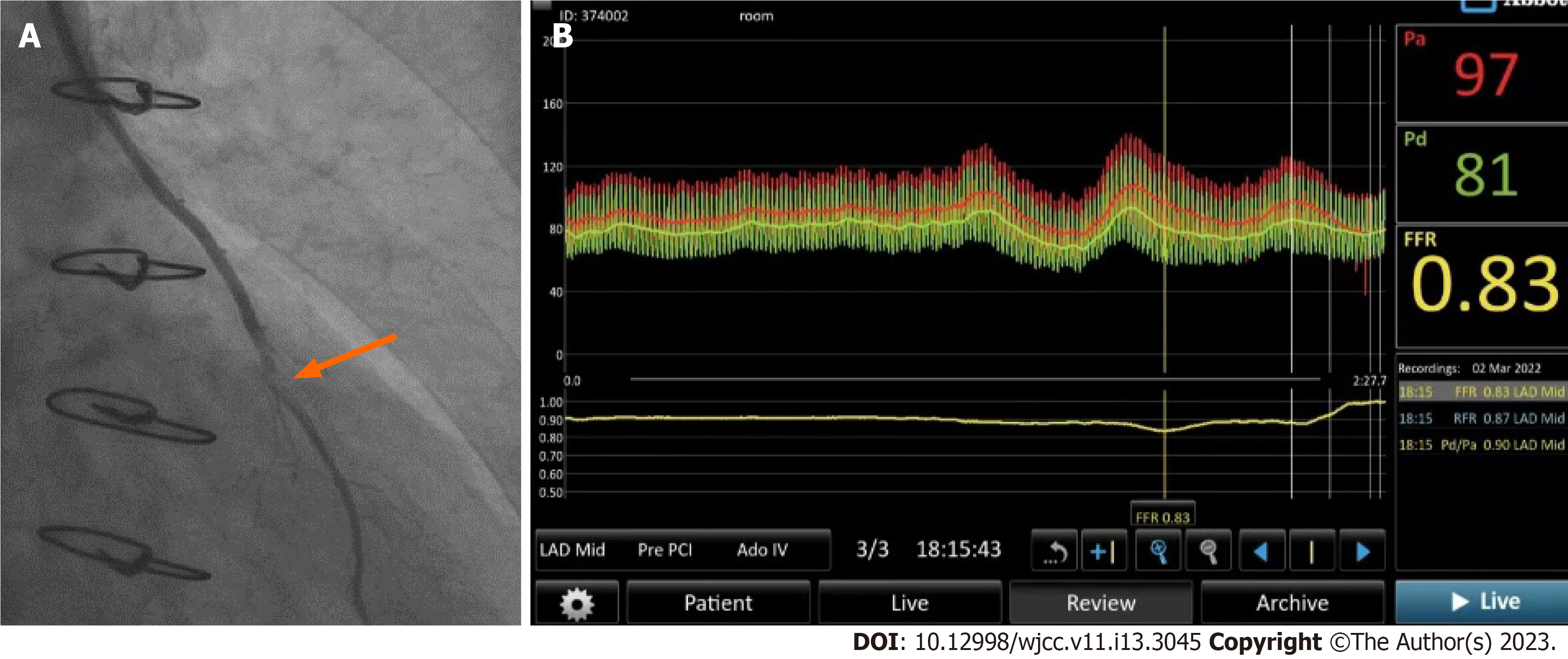
Case 2: Coronary artery angiography observed that the left coronary artery was dominant. There was no abnormality in the left main coronary artery. However, there was 60% segmental stenosis in the middle segment of LAD and chronic occlusion of the RCA from the opening with visible collateral circulation. The LIMA-LAD graft was unobstructed. However, there was 75% anastomotic stenosis (Figure 2A). Additionally, the saphenous vein-obtuse marginal branch graft was unobstructed. On cardiac ultrasound, the left ventricular ejection fraction was 50%, consistent with the changes of old myocardial infarction at the inferior and posterior heart walls.
Case 1: The pressure measuring guide wire was inserted into the stenotic segment of LAD through the LIMA, and the FFR value was measured to be 0.75 (positive) (Figure 1B).
Case 2: The FFR measured from the LIMA to the distal end of the anastomosis was 0.83 (negative) (Figure 2B).
The final diagnosis was stenosis at the distal end of the anastomosis of the LIMA-LAD graft.
The final diagnosis was segmental stenosis in the middle segment of LAD, chronic occlusion of the RCA and anastomotic stenosis.
Based on the positive FFR value, intervention was performed. In detail, dilation with a 2.0 mm × 31.0 mm balloon containing drugs was performed at the stenotic segment of the LAD via the LIMA (Figure 1C).
Based on the negative FFR value, the intervention was not performed. The patient was given drug treatments according to traditional Chinese medicine and Western medicine.
Remeasurement of pressure showed that the FFR after balloon dilation was 0.94 (Figure 1D). There was no residual stenosis as shown on coronary angiography. Three days after intervention, the symptoms of chest tightness were significantly relieved, and the patient was discharged. At the 3-mo follow-up, the patient had no recurrence of chest tightness or shortness of breath. The patient is currently under continual follow-up.
One week after drug treatment, the symptoms of chest tightness and shortness of breath were significantly relieved and the patient was discharged. At the 3-mo follow-up, there was no recurrence of chest tightness or shortness of breath. The patient is currently under continual follow-up.
LIMA is a commonly used vessel for CABG. Its advantages[6] are as follows: (1) The pedicled LIMA can regulate blood flow according to physiological needs; (2) The LIMA can produce prostaglandins, which can dilate blood vessels and resist platelet aggregation; and (3) The LIMA has less possibility of atherosclerosis, ensuring a high long-term patency rate. The 2 patients in this report had occlusion in the proximal segment of the anterior descending artery and occlusion in the middle segment of the anterior descending artery. The blood supply of the anterior myocardium mainly came from the LIMA graft. Thus, intervention may be performed through the LIMA. However, re-intervention therapy should be performed with caution after recurrence. It is shown that nearly 25% of patients with coronary angiography stenosis above 70% do not have myocardial ischemia[7]. For these patients, stenting or coronary bypass based on the results of coronary angiography alone will not only have no effect but also increase the financial and psychological burden of patients, leading to over-treatment.
FFR can objectively and accurately evaluate coronary function, thus providing evidence for interventional therapy and assisting in making precise treatment plans during interventional therapy[8,9]. A multicenter clinical trial[7] showed that compared with traditional percutaneous coronary intervention using FFR as the gold standard to guide patients with coronary artery diseases for revascularization intervention significantly improved the prognosis of patients and significantly reduced the incidence of adverse events. The 3-year follow-up results from the Compare-Acute study showed that FFR-guided complete revascularization in patients with ST-segment elevation myocardial infarction and multivessel disease could significantly reduce costs[10]. FFR measurement is currently the optimal method to confirm whether coronary stenosis is complicated with myocardial ischemia. The latest international views believe that coronary angiography + FFR measurement is the “gold standard” for the diagnosis and treatment of coronary heart disease[11]. Clinically, an FFR value greater than 0.8 indicates no myocardial ischemia, and an FFR value less than 0.8 indicates myocardial ischemia[12]. Under this gold standard, the precise treatment of coronary heart disease by stenting or bypass grafting can be achieved[13].
In patients with chest tightness and shortness of breath after CABG, it should be first considered whether there is a problem with the grafted blood vessels, especially the LIMA-LAD graft. There may be factors such as atherosclerotic stenosis in LIMA, anastomotic stenosis and stenosis in LAD at the distal end of the anastomosis[14]. Previously, intervention was determined by the stenosis degree assessed by the angiography of LIMA. However, angiography cannot determine whether there is ischemia in the distal myocardium. Thus, the intervention may have some blindness to a certain extent[7]. The measurement of FFR enables the quantitative evaluation of the degree of myocardial ischemia at the distal end of the anastomosis and can more accurately determine whether to intervene.
In this report, Case 1 had 85% stenosis in the LAD at the distal end of the anastomosis of the LIMA-LAD graft. The measured FFR value was 0.75 (positive), and then balloon dilation was performed. The measured FFR value after drug balloon dilation was 0.94 (negative). The patient’s symptoms were significantly relieved after intervention. In Case 2, although there was 75% stenosis at the anastomosis between the LIMA and the LAD, the FFR value was 0.83 (negative). This indicated that there may be no myocardial ischemia. Thus, intervention was not performed in Case 2, avoiding over-treatment. Case 2 was discharged after drug therapy.
Notably, this report is limited in that the measurement of FFR via LIMA was invasive and that we did not compare the FFR measured via LIMA with that measured by cardiac color Doppler.
In conclusion, we provided evidence that FFR measurement of grafted blood vessels, especially LIMA grafts, after CABG is a good method to determine the intervention course.
| 1. | Song CX, Dou KF. [Research progress of coronary function diagnosis]. Zhongguo Xunhuan Zazhi. 2017;32:403-405. [DOI] [Full Text] |
| 2. | Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993;87:1354-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 807] [Cited by in RCA: 821] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 3. | De Bruyne B, Fearon WF, Pijls NH, Barbato E, Tonino P, Piroth Z, Jagic N, Mobius-Winckler S, Rioufol G, Witt N, Kala P, MacCarthy P, Engström T, Oldroyd K, Mavromatis K, Manoharan G, Verlee P, Frobert O, Curzen N, Johnson JB, Limacher A, Nüesch E, Jüni P; FAME 2 Trial Investigators. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med. 2014;371:1208-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 772] [Cited by in RCA: 844] [Article Influence: 70.3] [Reference Citation Analysis (0)] |
| 4. | Driessen RS, Danad I, Stuijfzand WJ, Raijmakers PG, Schumacher SP, van Diemen PA, Leipsic JA, Knuuti J, Underwood SR, van de Ven PM, van Rossum AC, Taylor CA, Knaapen P. Comparison of Coronary Computed Tomography Angiography, Fractional Flow Reserve, and Perfusion Imaging for Ischemia Diagnosis. J Am Coll Cardiol. 2019;73:161-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 332] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 5. | Zhao Q, Yang Y, Zhu YP. [The state of the art for arterial coronary artery bypass grafting]. Zhonghua Waike Zazhi. 2020;58:337-340. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Harky A, Sankaranarayanan V, Kong QG. Internal mammary artery: the primary conduit for surgical revascularization. Coron Artery Dis. 2021;32:64-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van' t Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2974] [Cited by in RCA: 3164] [Article Influence: 186.1] [Reference Citation Analysis (0)] |
| 8. | Chen J, Wetzel LH, Pope KL, Meek LJ, Rosamond T, Walker CM. FFR(CT): Current Status. AJR Am J Roentgenol. 2021;216:640-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Mangiacapra F, Bressi E, Sticchi A, Morisco C, Barbato E. Fractional flow reserve (FFR) as a guide to treat coronary artery disease. Expert Rev Cardiovasc Ther. 2018;16:465-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Smits PC, Laforgia PL, Abdel-Wahab M, Neumann FJ, Richardt G, Boxma-de Klerk B, Lunde K, Schotborgh CE, Piroth Z, Horak D, Wlodarczak A, Frederix GW, Omerovic E. Fractional flow reserve-guided multivessel angioplasty in myocardial infarction: three-year follow-up with cost benefit analysis of the Compare-Acute trial. EuroIntervention. 2020;16:225-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, Maccarthy PA, Van't Veer M, Pijls NH. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816-2821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 893] [Cited by in RCA: 959] [Article Influence: 59.9] [Reference Citation Analysis (0)] |
| 12. | Muller O, Mangiacapra F, Ntalianis A, Verhamme KM, Trana C, Hamilos M, Bartunek J, Vanderheyden M, Wyffels E, Heyndrickx GR, van Rooij FJ, Witteman JC, Hofman A, Wijns W, Barbato E, De Bruyne B. Long-term follow-up after fractional flow reserve-guided treatment strategy in patients with an isolated proximal left anterior descending coronary artery stenosis. JACC Cardiovasc Interv. 2011;4:1175-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Wardziak Ł, Kruk M, Pleban W, Demkow M, Rużyłło W, Dzielińska Z, Kępka C. Coronary CTA enhanced with CTA based FFR analysis provides higher diagnostic value than invasive coronary angiography in patients with intermediate coronary stenosis. J Cardiovasc Comput Tomogr. 2019;13:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Higami T, Yamashita T, Nohara H, Iwahashi K, Shida T, Ogawa K. Early results of coronary grafting using ultrasonically skeletonized internal thoracic arteries. Ann Thorac Surg. 2001;71:1224-1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Dabla PK, India; He YH, China S-Editor: Li L L-Editor: Filipodia P-Editor: Yu HG