Published online May 6, 2023. doi: 10.12998/wjcc.v11.i13.3038
Peer-review started: November 16, 2022
First decision: February 14, 2023
Revised: February 19, 2023
Accepted: April 4, 2023
Article in press: April 4, 2023
Published online: May 6, 2023
Processing time: 159 Days and 0.5 Hours
Closed rupture of the little and ring finger flexor tendons caused by the hamate is mostly associated with a fracture or nonunion of the hamate hook. Only one case of a closed rupture of the finger flexor tendon caused by osteochondroma in the hamate has been reported. Here, we present a case study to highlight the possibility of hamate osteochondroma as a rare cause of finger closed flexor tendon rupture based on our clinical experience and literature review.
A 48-year-old man who had been a rice-field farmer for 7–8 h a day for the past 30 years visited our clinic due to the loss of right little finger and ring finger flexion involving both the proximal and distal interphalangeal joints. The patient was diagnosed with a complete rupture of the ring and little finger flexors because of the hamate and was pathologically diagnosed with an osteochondroma. Exploratory surgery was performed, and a complete rupture of the ring and little finger flexors due to an osteophyte-like lesion of the hamate was observed, which was pathologically diagnosed as an osteochondroma.
One should consider that osteochondroma in the hamate may be the cause of closed tendon ruptures.
Core Tip: It is not easy to diagnose osteochondroma in the hamate. Therefore, osteochondroma in the hamate should be considered as a cause when dealing with patients with closed ruptures of the finger flexor tendon. Based on our experience, we also suggest that the surgical treatment of these patients requires careful pre-operative planning and preparation.
- Citation: Kwon TY, Lee YK. Multiple flexor tendon ruptures due to osteochondroma of the hamate: A case report. World J Clin Cases 2023; 11(13): 3038-3044
- URL: https://www.wjgnet.com/2307-8960/full/v11/i13/3038.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i13.3038
Closed ruptures of the flexor tendons other than in nonrheumatic patients are uncommon. These ruptures are frequently caused by intrinsic tendon pathology or structural deformities[1]. Closed rupture of the finger flexor tendons caused by the hamate is mostly associated with a fracture or nonunion of the hamate hook[2,3]. Only one case of a closed rupture of the finger flexor tendon caused by osteochondroma in the hamate has been reported[4]. An osteochondroma is a tumor that arises mainly from the metaphyses of long bones and is the most common form of primary benign bone tumor. However, it is rarely found in carpal bones[5-8]. In this report, we present a case study to highlight the possibility of hamate osteochondroma as a rare cause of finger closed flexor tendon rupture based on our clinical experience and literature review.
A 48-year-old man complained of the inability to flex his right ring finger (RRF) and right small finger (RSF).
The patient was unable to perform active flexion of the RSF for about 2 wk and active flexion of the RRF for about one week. The condition occurred without pain or a definite episode of trauma.
He had been a rice-field farmer for 7−8 h a day for the past 30 years.
There was no history or evidence of rheumatoid or other inflammatory arthritis conditions.
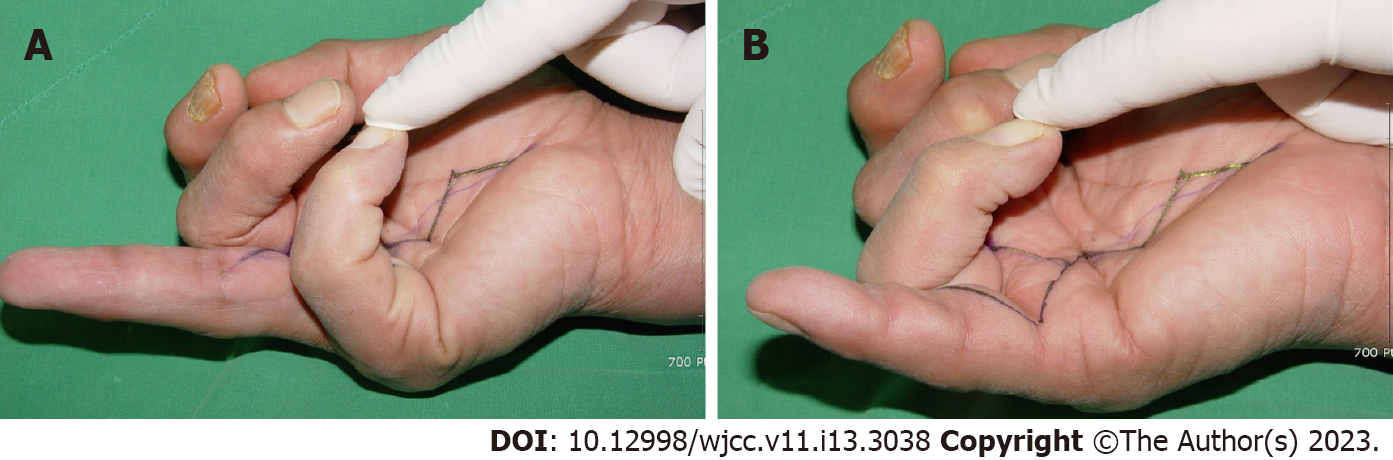
Physical examination revealed no swelling or tenderness of the palm. However, he could not actively flex either the proximal or distal interphalangeal joint of the RRF and RSF (Figure 1A and B).
The patient’s rheumatoid serology results were normal.
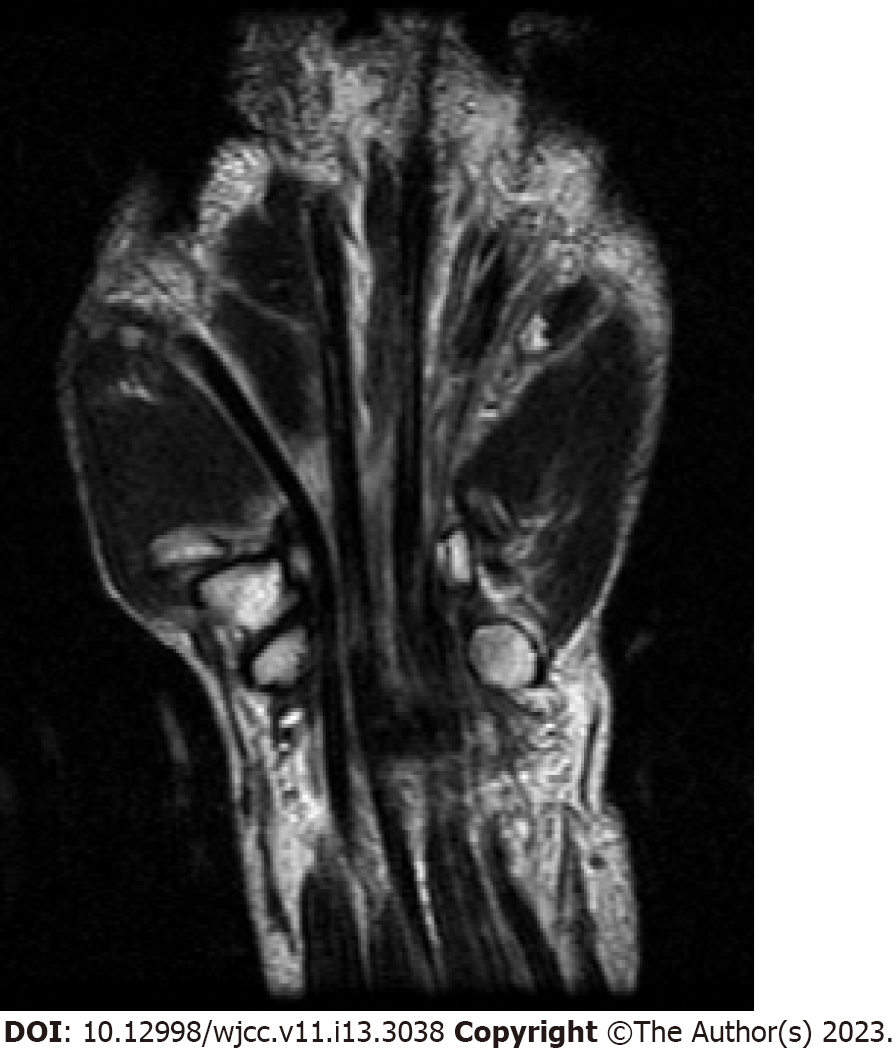
The radiologist reported no specific findings on preoperative magnetic resonance imaging (MRI) other than ring finger and small finger flexor tendon ruptures (Figure 2).
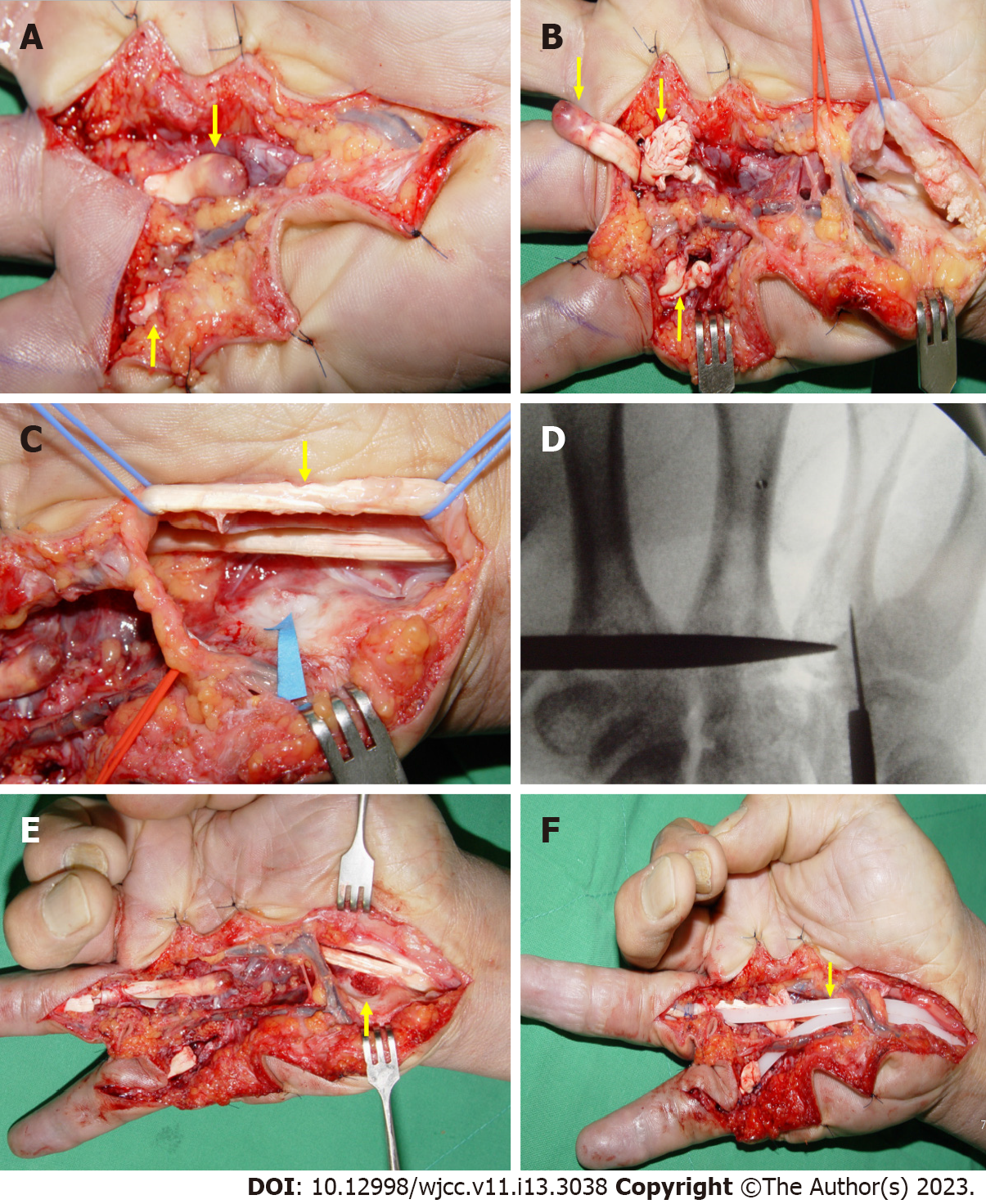
The flexor tendons were explored under regional anesthesia through a volar zig-zag incision. During surgery, the flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS) tendons of the RRF and RSF were found to be completely ruptured (Figure 3A and B). Additionally, the flexor tendons of the long finger were attenuated and frayed. On the side of the hamate in the carpal tunnel, a protruding bony structure like an osteophyte was identified, which was covered by cartilage (Figure 3C). The flexor tendons were determined to be worn and ruptured by this structure. We used a C-arm image intensifier to identify this area during surgery (Figure 3D). It was excised and sent for histological examination (Figure 3E). Although we knew that primary reconstruction through tendon transfer or a free tendon graft was the best treatment for ruptured flexor tendons, we decided to perform staged tendon reconstruction after considering various factors. The ruptured flexor tendons were debrided, and Hunter rods (Wright Medical Technology, Inc., Arlington, TN, USA) were inserted (Figure 3F).
The final diagnosis was multiple flexor tendon ruptures due to osteochondroma of the hamate
Postoperatively, the wrist was immobilized with dorsal block short arm splint for 2 wk.
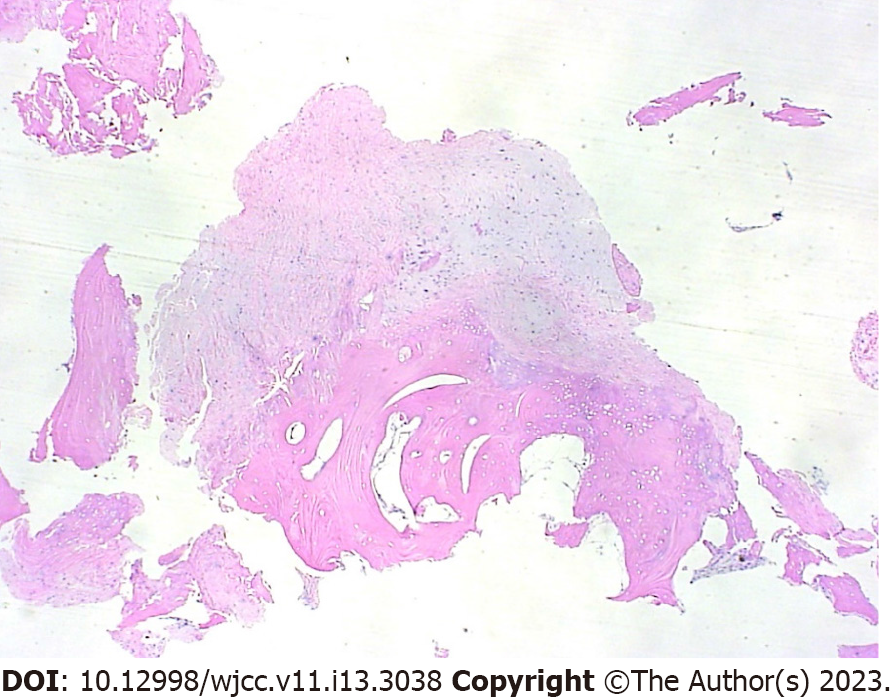
The histopathological examination revealed osteochondroma of the hamate with no malignant changes (Figure 4). However, tendon reconstruction could not be performed because the patient did not return to the hospital as he was busy with work.
An osteochondroma is a common tumor that accounts for 30% of benign bone tumors and 10%−15% of all bone tumors[9]. Since most cases are asymptomatic, they are often detected incidentally on radiographs and are commonly found around the knee area. Carpal osteochondroma is very rare and only three cases involving the hamate have been reported[4,6,8]. Only one case of carpal osteo
Closed injuries to the flexor tendon are rare and, therefore, can be easily missed initially. The causes of closed rupture of the flexor tendons reported in previous papers were distal radius fractures, nonunions of the scaphoid, tendolipomatosis, dislocations of the lunate, Kienböck's disease, osteoarthritis of the pisotriquetral joint, and fractures or nonunions of the hamate hook[2,3,11-15]. Sometimes, closed ruptures of the flexor tendon occur without any underlying pathological conditions. Although the etiology of closed ruptures is unclear, these injuries likely depend on the interplay of several factors, including vascular alterations, repetitive microtrauma, local anatomic features, tendon anomalies, and genetic or other endogenous influences[16].
Closed ruptures of the flexor tendons are usually treated with primary reconstruction through tendon graft interposition or tendon transfer[17]. In addition, since osteochondroma is a benign and slow-growing tumor, it has been reported that there is no problem with primary treatment has been reported, even if accompanied by tendon rupture[7]. However, we have limited hand surgery experience at the time of this case. Initially, we planned primary tendon reconstruction via tendon transfer from the third FDS. However, since the third FDS tendon was also frayed and attenuated, tendon transfer could not be performed. As an alternative treatment method, we considered reconstruction using free tendon graft interposition. Two palmaris longus tendons should be harvested to ensure the success of this treatment, but we found this option unsuitable since surgery on this patient was not performed under general anesthesia. Moreover, if the grafted tendon passes through the osteochondroma removal site, there is a possibility of re-rupture due to wear of the tendon. Thus, we performed a Hunter rod insertion instead. However, this was done because of our lack of both experience and thorough preoperative preparation, which would have discovered the osteochondroma before surgery. In this regard, we suggest that careful planning and preparation are needed before surgery for patients with closed ruptures of the flexor tendon.
Rice-field farmers frequently work in small-scale agricultural settings using hand hoes and small sickles. Repetitive movements of the wrist are required to use these tools, and there is full wrist flexion with ulnar deviation. Thus, the FDP tendons of the ulnar digits deviate to an acute angle at the hamate in the carpal tunnel. Moreover, repetition of these movements can produce friction between the flexor tendon and the surface of the hamate, leading to attrition of both the tendon and the surface of the hamate[18]. Our patient had been a rice-field farmer for the past 30 years. Long-term repeated movements led to the attrition of both the tendon and the surface of the hamate. Moreover, microtrauma of the hamate because of its irregularity due to an osteochondroma was the main cause of flexor tendon rupture.
One limitation of this case report is that secondary tendon reconstruction could not be performed because the patient did not return to the hospital as he was busy with work. Therefore, we could not show the final result of his reconstructed fingers, and there was no final follow-up to determine whether the hamate osteochondroma recurred.
In the present case, repetitive friction between the flexor tendons and osteochondroma of the hamate may have caused tendon rupture. However, given that it is not easy to diagnose osteochondroma in the hamate, osteochondroma in the hamate should be considered as the cause when dealing with patients with closed ruptures of the finger flexor tendon. Based on our experience, we also suggest that surgical treatment requires careful pre-operative planning and preparation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Modi N, India S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | De Smet L, Baeten Y. Closed rupture of both flexor tendons of the fifth finger due to a calcium hydroxyapatite deposit in the carpal tunnel. Acta Orthop Belg. 1998;64:336-338. [PubMed] |
| 2. | Yamazaki H, Kato H, Nakatsuchi Y, Murakami N, Hata Y. Closed rupture of the flexor tendons of the little finger secondary to non-union of fractures of the hook of the hamate. J Hand Surg Br. 2006;31:337-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Stark HH, Chao EK, Zemel NP, Rickard TA, Ashworth CR. Fracture of the hook of the hamate. J Bone Joint Surg Am. 1989;71:1202-1207. [PubMed] |
| 4. | Motomiya M, Sakazaki T, Iwasaki N. Atypical osteochondroma of the hamate that presented clinically as carpal tunnel syndrome: report of an extremely rare case and literature review. BMC Musculoskelet Disord. 2020;21:231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Malhotra R, Maheshwari J, Dinda AK. A solitary osteochondroma of the capitate bone: a case report. J Hand Surg Am. 1992;17:1082-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Koti M, Honakeri SP, Thomas A. A multilobed osteochondroma of the hamate: case report. J Hand Surg Am. 2009;34:1515-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Shah NR, Wilczynski M, Gelberman R. Osteochondroma of the capitate causing rupture of the extensor digiti minimi: case report. J Hand Surg Am. 2009;34:46-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Cha SM, Shin HD, Kim DY. A solitary unilobed osteochondroma of the hamate: a case report. J Pediatr Orthop B. 2017;26:274-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, Bai M. Osteochondromas: review of the clinical, radiological and pathological features. In Vivo. 2008;22:633-646. [PubMed] |
| 10. | Göçmen S, Topuz AK, Atabey C, Şimşek H, Keklikçi K, Rodop O. Peripheral nerve injuries due to osteochondromas: analysis of 20 cases and review of the literature. J Neurosurg. 2014;120:1105-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Takami H, Takahashi S, Ando M. Attritional flexor tendon ruptures after a malunited intra-articular fracture of the distal radius. Arch Orthop Trauma Surg. 1997;116:507-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Johnston GH, Bowen CV. Attritional flexor tendon ruptures by an old lunate dislocation. J Hand Surg Am. 1988;13:701-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Inoué G. Attritional rupture of the extensor tendon due to longstanding Kienböck's disease. Ann Chir Main Memb Super. 1994;13:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Crosby EB, Linscheid RL. Rupture of the flexor profundus tendon of the ring finger secondary to ancient fracture of the hook of the hamate. Review of the literature and report of two cases. J Bone Joint Surg Am. 1974;56:1076-1078. [PubMed] |
| 15. | Lee YK, Lee M. Spontaneous rupture of flexor pollicis longus tendon by tendolipomatosis in proximal phalanx: A case report. Medicine (Baltimore). 2018;97:e12157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Bois AJ, Johnston G, Classen D. Spontaneous flexor tendon ruptures of the hand: case series and review of the literature. J Hand Surg Am. 2007;32:1061-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Netscher DT, Badal JJ. Closed flexor tendon ruptures. J Hand Surg Am. 2014;39:2315-23; quiz 2323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Lee GJ, Kwak S, Kim HK, Ha SH, Lee HJ, Baek GH. Spontaneous Zone III rupture of the flexor tendons of the ulnar three digits in elderly Korean farmers. J Hand Surg Eur Vol. 2015;40:281-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |