Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2811
Peer-review started: December 26, 2022
First decision: January 17, 2023
Revised: January 26, 2023
Accepted: March 9, 2023
Article in press: March 9, 2023
Published online: April 26, 2023
Processing time: 120 Days and 12.3 Hours
In the modern era of endovascular surgery percutaneous interventions are being widely used to treat a number of vascular disorders including arteriovenous fistulas (AVF). Still, patients with hostile anatomy or complicated cases such as large post-traumatic AVFs may be successfully treated using conventional vascular surgery.
This paper presents state-of-the-art treatment options in subjects with post-traumatic AVFs and a case-report of a successful open surgical approach in a patient with a 25 year old history of a post-traumatic AVF between the common femoral artery and common femoral vein.
Open surgery is still a great option to treat patients with post-traumatic arteriovenous fistulas with hostile anatomy or in complicated cases. Concomitant conditions and complications should be addressed promptly.
Core Tip: Conventional open vascular surgery is a great option in treatment of post-traumatic arterio-venous fistulas involving femoral vessels in patients with hostile anatomy or complicated cases leading to aneurysm formation and limb ischemia.
- Citation: Kalinin R, Suchkov I, Mzhavanadze N, Borisova Y, Panin I. Open surgery: Still a great option to treat patients with post-traumatic arteriovenous fistulas: A case report. World J Clin Cases 2023; 11(12): 2811-2816
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2811.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2811
Stab, gunshot wounds or other traumas to the groin may lead to the discrete injury to the femoral vessels and nerve with delayed complications. Exact rates of post-traumatic arterio-venous fistulas (AVF) of the lower extremity arteries are not known. When not diagnosed in a timely manner, certain AVF complications may develop. Among them are lower leg edema, heart failure[1], vein dilation and chronic venous insufficiency[2], lower leg ischemia, trophic ulcers.
Percutaneous interventions are being widely used to treat a number of vascular disorders including AVF[3,4]. Still, patients with hostile anatomy or complicated cases such as large post-traumatic AVFs may be successfully treated using conventional vascular surgery.
We present a case of a male patient with a 25 year old history of a post-traumatic AVF between the common femoral artery and common femoral vein.
Non-healing left leg ulcers and a pulsatile mass in the left groin.
A 62 - year old male was admitted to the vascular surgery department with complaints on the lower limb trophic ulcers (Figure 1) and a pulsatile mass in the left groin. The patient had a history of a single stab wound to his left groin 25 years prior to admission. The subject recalled undergoing a surgical exploration of the left groin back in 1997, and had not contacted any medical professionals ever since.
No apparent history of past illnesses.
No history of cardiovascular disease in the family.
A physical examination at admission showed that the patient was in a stable condition. Blood pressure was 130/80 mmHg, pulse rate 75 beats per minute, regular, respiratory rate 16, temperature 36.5°C. There were a large pulsatile mass in the left inguinal area, signs of lower leg ischemia, varicose veins and post-thrombotic syndrome, lower leg trophic ulcers, peripheral neuropathy.
Laboratory tests were within normal values.
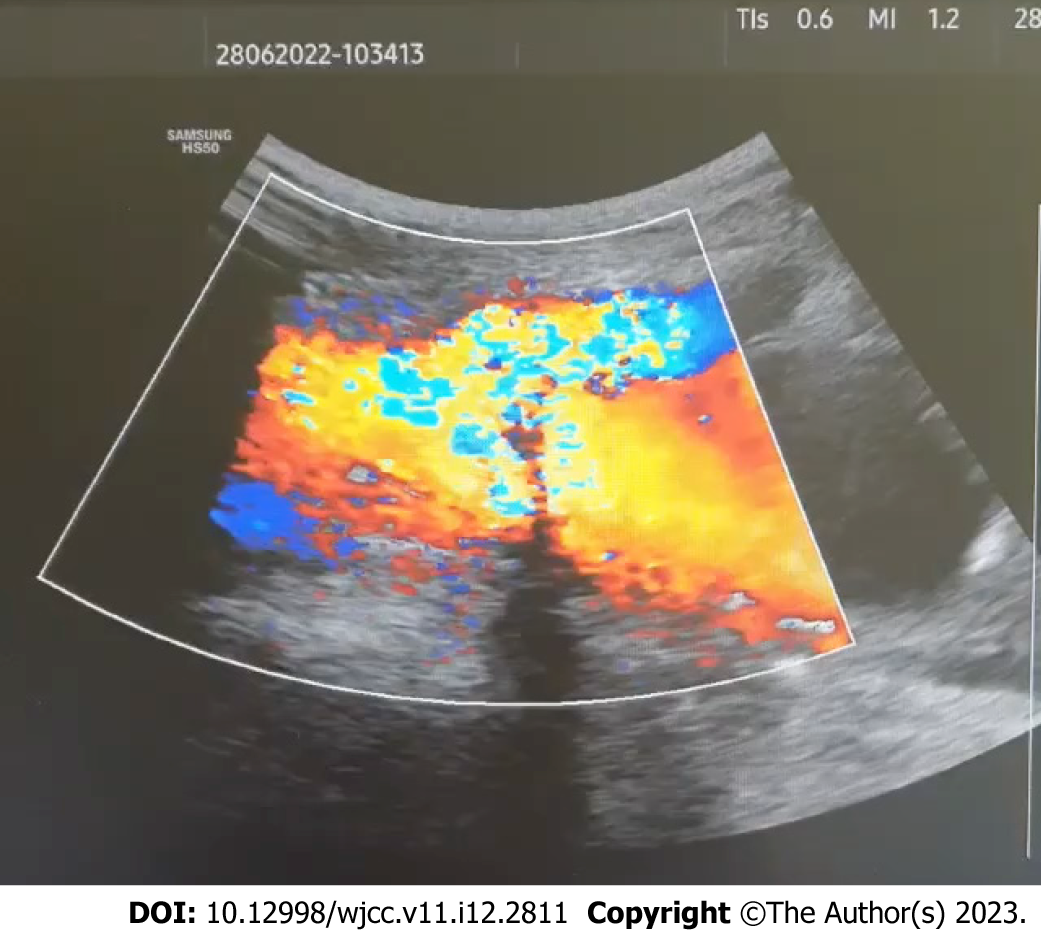
Duplex ultrasonography (DUS) revealed a communication and turbulent blood flow between the left common femoral artery and left common femoral vein (Figure 2), an aneurysm of the left common femoral vein with calcification of posterior and medial walls (Figure 3), occlusion of the femoral and deep femoral vein distal to their confluence with common femoral vein, and multiple varicose veins on the left thigh.
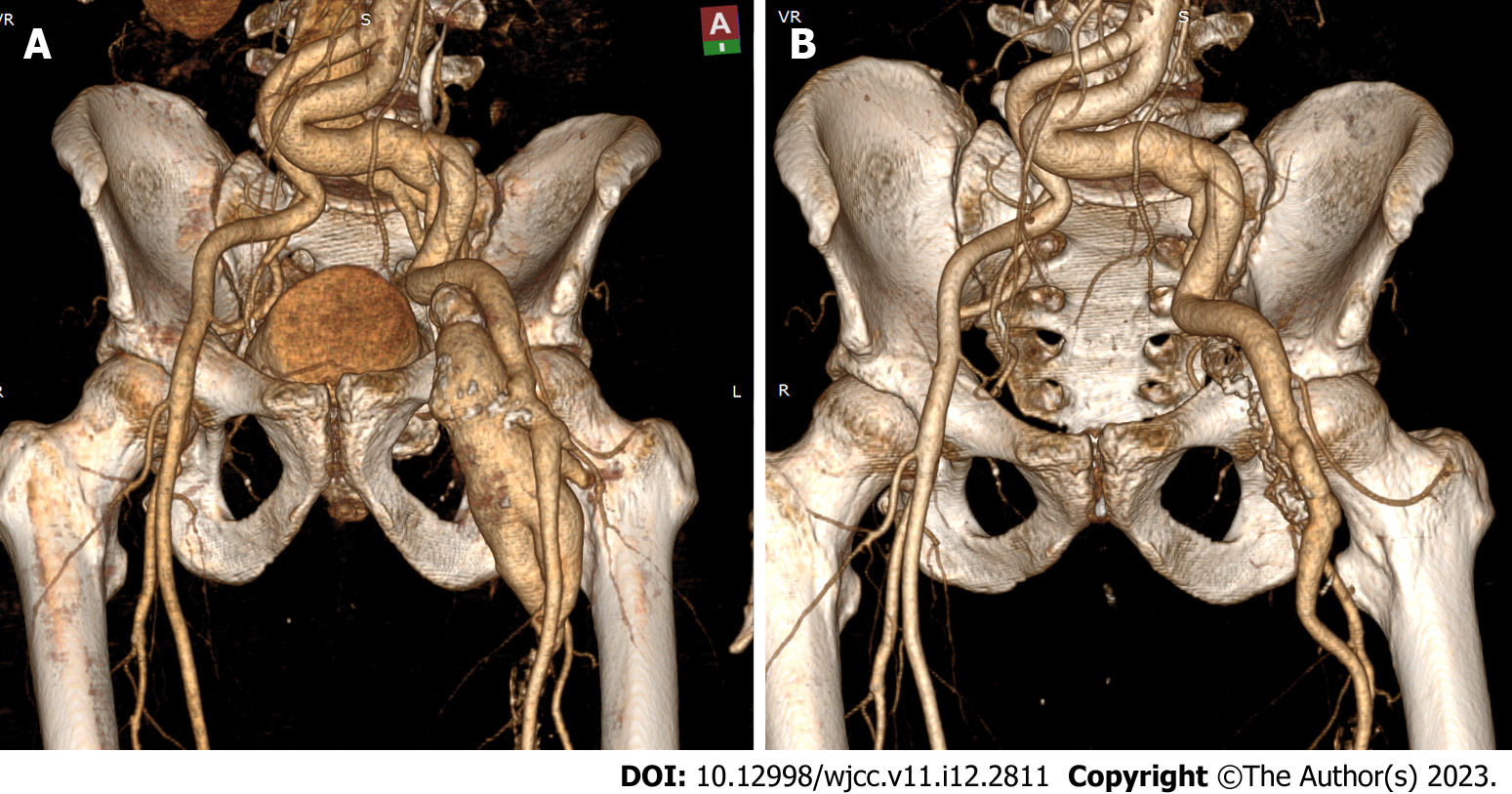
Contrast enhanced computed tomography angiography (CT-angiography) performed at admission revealed an arteriovenous fistula between the left common femoral artery and left common femoral vein with an aneurysm of the latter, aneurysms of the proximal parts of the left deep femoral vein, femoral vein with further venous occlusion; CT-angiography also revealed dilated left iliac arteries (Figure 4).
Echocardiography was also performed and showed a normal ejection fraction, insignificant right and left atrial enlargement, mild left ventricular hypertrophy.
Post-traumatic arteriovenous fistula between left common femoral artery and left common femoral vein (after a single stab wound to the groin 25 years prior to admission). Aneurysm of the left common femoral vein. Post-thrombotic disease. Secondary varicose veins. Chronic lower limb ischemia. Trophic ulcers of the lower leg. Peripheral neuropathy.
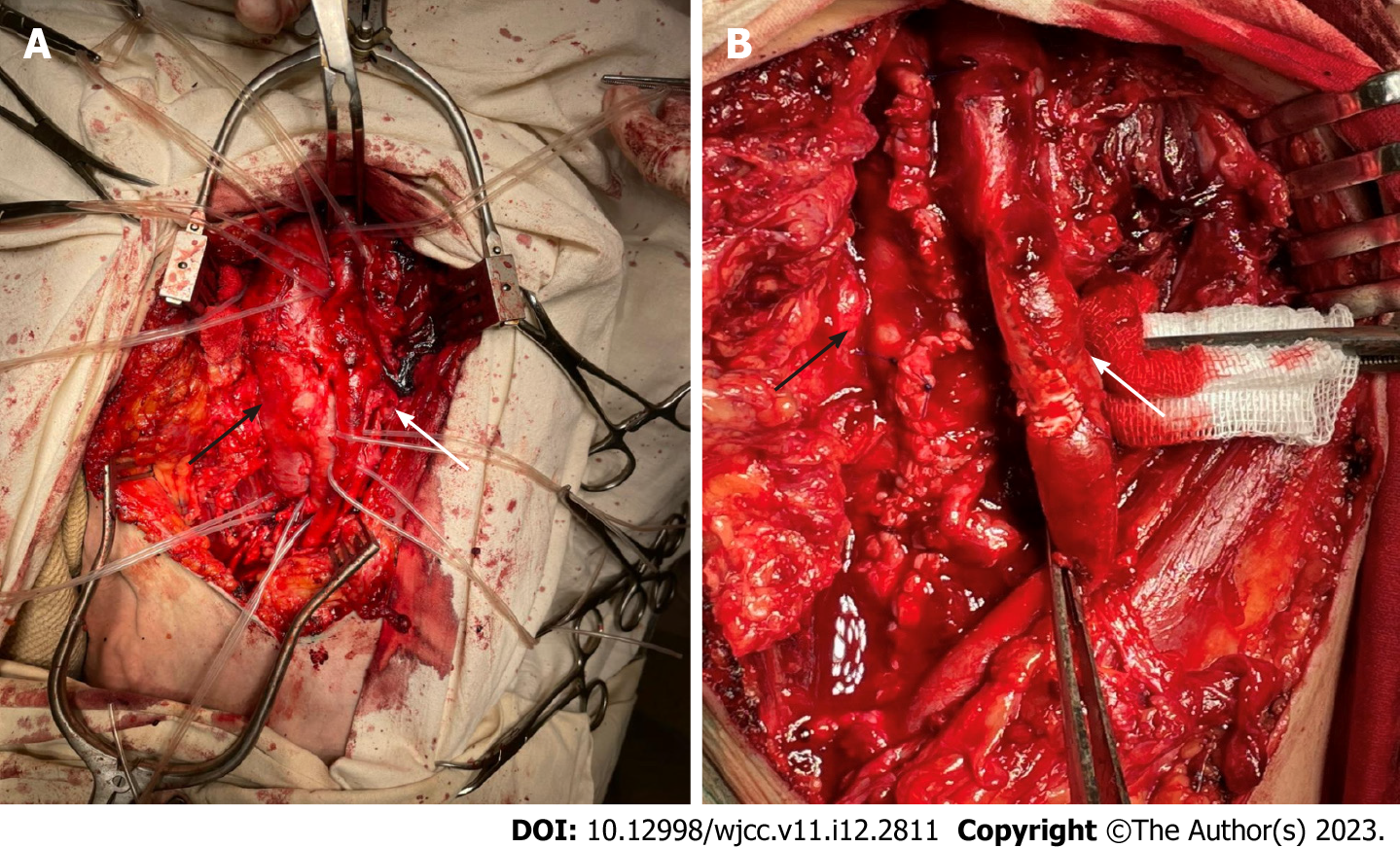
We performed an open procedure. An open access to the femoral vessels in the left infrainguinal area (Figure 5A) with some technical difficulties due to extended fibrotic lesions at the sight of the AVF and left common femoral vein aneurysm, closure of the AVF with a synthetic PTFE patch, aneurysmorrhaphy of the left common femoral vein (Figure 5B). We decided to keep the dilated iliac arteries intact in order to avoid the use of extended synthetic grafts in the settings of multiple trophic ulcers. Intraoperative blood loss was 250 mL. The patient was started on aspirin 75 mg QD, atorvastatin 20mg QD, heparin 1000 units per hour IV for 24 h followed by enoxaparin 40 mg SC QD, famotidine 40 mg QD, amoxicillin/clavulanic acid 875 mg/125 mg IV BID, thioctic acid 600 mg IV QD.
Endovascular treatment was avoided in this case due to the following reasons: placement of a stent graft into the common femoral artery would have put the patient at the potential risk of stent fracture related to hip joint flexion; blood flow to the deep femoral artery would have been compromised, too.
Post-operative period was uneventful. On the 7th day following the procedure we performed a repeat CT-scanning with contrast enhancement, which revealed the absence of arteriovenous fistula between the left common femoral artery and left common femoral vein with successfully preserved flow through both femoral and deep femoral arteries. Trophic ulcers healed within 2 mo following the procedure.
Endovascular surgery has been a leading trend in vascular surgery for the past decades. Arterio-venous fistulas of different nature and localization can be successfully treated using transcutaneous techniques such as endovascular coiling, embolization or placement of a stent-graft depending on the clinical settings[5-7].
As the AVF was located directly across the orifice of the deep femoral artery and was accompanied by a large aneurysm of the left common femoral vein, we decided to perform an open procedure as the placement of an endovascular stent graft might have caused diminished flow through the deep femoral artery and led to the possibility of a thrombus formation in a dilated common femoral vein with subsequent risks of pulmonary embolism.
Stab, gunshot wounds or other traumas to the groin should be carefully evaluated to exclude injury to the femoral vessels and nerve, which eventually may lead to the formation of arteriovenous fistulas and vascular aneurysms. A misdiagnosis may occur due to simple wound exploration with no prior or further DUS, CT-angiography, or digital subtraction angiography, which are necessary in order to avoid delayed complications[8].
In the era of endovascular procedures, conventional open vascular surgery is still a great option in treatment of post-traumatic arteriovenous fistulas involving femoral vessels in patients with complicated cases leading to aneurysm formation and lower limb ischemia. Possible concomitant conditions or complications such as heart failure or peripheral neuropathy should be addressed promptly.
| 1. | Zhang HY, Chai DZ. Post-traumatic Femoral Arteriovenous Fistula. Eur J Vasc Endovasc Surg. 2017;54:377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Kalinin RE, Suchkov IA, Kaydakova EY, Mzhavanadze ND, Shanaev IN. Chronic venous insufficiency as a possible clinical manifestation of a post-traumatic lower limb arteriovenous fistula. Acta Phlebologica. 2021;22:100-4. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Rogel-Rodríguez JF, Zaragoza-Salas T, Díaz-Castillo L, Noriega-Salas L, Rogel-Rodríguez J, Rodríguez-Martínez JC. [Post-traumatic femoral arteriovenous fistula, endovascular treatment]. Cir Cir. 2017;85:158-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Gorsi U, Agarwal V, Savlania A, Behra A, Sandhu MS. Endovascular Management of Lower Limb Arteriovenous Fistula Presenting 8 Years After Gunshot Injury. Vasc Endovascular Surg. 2019;53:670-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | De Martino RR, Nolan BW, Powell RJ, Walsh DB, Stone DH. Stent graft repair of iatrogenic femoral arteriovenous fistula: a useful therapeutic approach in a hostile groin. Vasc Endovascular Surg. 2010;44:40-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Tufano A, Asero V, Proietti F, Flammia RS, Franco G, Leonardo C. Arteriovenous fistula after robotic partial nephrectomy: Case report and narrative review. Radiol Case Rep. 2022;17:2550-2553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 7. | Tufano A, Minelli R, Rossi E, Brillantino C, Di Serafino M, Zeccolini M, Cantisani V, Vallone G. Inferior epigastric artery pseudoaneurysm secondary to port placement during a robot-assisted laparoscopic radical cystectomy. J Ultrasound. 2021;24:535-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Nagpal K, Ahmed K, Cuschieri R. Diagnosis and management of acute traumatic arteriovenous fistula. Int J Angiol. 2008;17:214-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Peripheral vascular disease
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Haddadi S, Algeria; Tufano A, Italy S-Editor: Liu JH L-Editor: A P-Editor: Liu JH