Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2796
Peer-review started: November 15, 2022
First decision: February 14, 2023
Revised: March 3, 2023
Accepted: March 22, 2023
Article in press: March 22, 2023
Published online: April 26, 2023
Processing time: 161 Days and 13.6 Hours
Inferior oblique anterior transposition (IOAT) has emerged as an effective surgery in the management of dissociated vertical deviation (DVD) combined with superior oblique palsy (SOP). Traditional IOAT usually provides satisfactory pri
We report the outcomes of the modified unilateral IOAT in two patients with unilateral DVD combined with SOP. The anterior-nasal fibers of the inferior oblique muscle were attached at 9 mm posterior to the corneal limbus along the temporal board of the inferior rectus muscle, the other fibers were attached a further 5 mm temporal to the anterior-nasal fibers. Postoperatively, both hype
In these cases, the modified unilateral IOAT was an effective and safe surgical method for treating DVD with SOP.
Core Tip: Inferior oblique anterior transposition (IOAT) is effective for dissociated vertical deviation combined with superior oblique palsy; however, unilateral IOAT also increases the risk of the anti-elevation syndrome. This modified unilateral IOAT involves a more backward new insertion and the new insertion line perpendicular to the inferior rectus muscle axis, which provides satisfactory primary position alignment and restricts the superior floating phenomenon without obvious postoperative complications.
- Citation: Zong Y, Wang Z, Jiang WL, Yang X. Modified inferior oblique anterior transposition for dissociated vertical deviation combined with superior oblique palsy: A case report. World J Clin Cases 2023; 11(12): 2796-2802
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2796.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2796
The clinical features of dissociated vertical deviation (DVD) with superior oblique palsy (SOP) are variable and include unstable vertical strabismus after covering in the primary position due to significant DVD; spontaneous upward drifting of one or both eyes when binocularity is blocked after neutralizing the hypertropia; and superior oblique muscle (SO) paralysis[1,2]. The goals of surgery are improvement of primary position hypertropia and reduction of upward floating. Inferior oblique anterior transposition (IOAT) has been recognized as the standard surgical procedure[1,2]. The complications after this procedure remain a difficult problem, such as the anti-elevation syndrome (AES)[3] and eyelid fission narrowing in straight-ahead gaze[4], especially after unilateral surgery. We here report the results of a modified unilateral IOAT in two patients with DVD and SOP.
IOAT was first proposed by Gobin[5] in 1964 and used in the treatment of esotropia with V sign, the inferior oblique muscle (IO) was transposed to the equatorial sclera (about 14 mm from the corneal limbus) and approximately 50% of patients were orthotropic after the procedure. The application of IOAT in the treatment of inferior oblique overaction (IOOA) and DVD was first proposed by Elliott and Nankin[6] in 1981. IOAT is a more effective treatment for IOOA and DVD than simple IO recession, with the anterior fibers of the IO fixed temporally at the inferior rectus (IR) insertion (Elliott’s point). It was reported that 67% (14/21) of patients’ hypertropia was corrected, but it was easily overcorrected, resulting in restricted elevation in 24% of the patients.
This novel unilateral IOAT method involves a more backward reinsertion line perpendicular to the IR axis with J-deformity. The anterior-nasal fibers of the IO were attached at 9 mm posterior to the corneal limbus along the temporal board of the IR, and the posterior fibers were attached a further 5 mm temporal to the first suture.
This procedure was performed by a single surgeon (YX) for DVD with SOP in the two patients between June and August 2020. One day after surgery, they were orthotropic in primary gaze without diplopia and remained orthotropic one year after the procedure without obvious AES. This approach ensured surgical effectiveness and prevented the onset of AES, especially after unilateral surgery.
This study was approved by the Medical Ethics Committee of Qingdao University. This report complies with all local laws and the principles of the Declaration of Helsinki.
Case 1: An 11-year-old Chinese girl presented with persistent exotropia after a strabismus procedure five years earlier.
Case 2: A 17-year-old Chinese girl presented with intermittent exotropia of the left eye. She had been tilting her head to the left since infancy.
Case 1: The patient had been tilting her head to the right since infancy and, in 2015, was diagnosed with constant exotropia. She underwent lateral rectus recession (6 mm) with medial rectus resection (5 mm) in her right eye, but residual exotropia and abnormal head position persisted postoperatively through to the current presentation.
Case 2: The patient presented with intermittent exotropia of the left eye. She had been tilting her head to the right since infancy without any prior treatment.
The patients had no previous medical history.
Case 1: The patient’s parents and sister are healthy and have no family history of similar disease.
Case 2: The patient’s parents, sister and brother are healthy and have no family history of similar disease.
Case 1: The patient’s temperature was 36.3 °C, heart rate was 92 bpm, respiratory rate was 23 breaths/min, and blood pressure was 94/54 mmHg.
Case 2: The patient’s temperature was 36.5 °C, heart rate was 98 bpm, respiratory rate was 20 breaths/min, and blood pressure was 104/67 mmHg.
Routine blood and biochemical tests were normal in both cases.
Ultrasonography did not indicate intraocular disease in both cases.
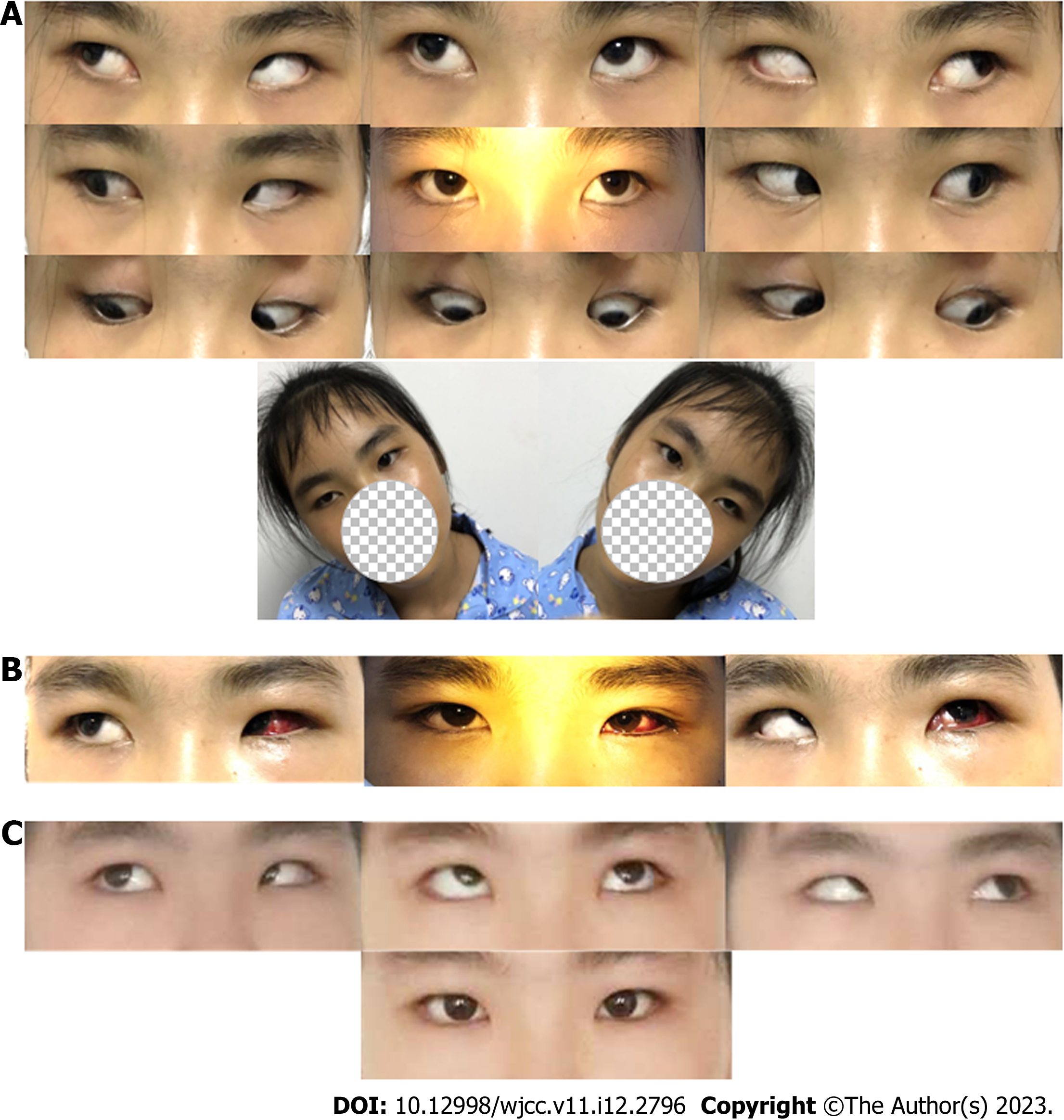
Case 1: On examination, the patient’s best-corrected visual acuity (BCVA) was 1.0 in both eyes. She had primary position exotropia of 40∆ at both distance and near, and a hypertropia of 10∆ in the left eye by alternate prism cover test. DVD was observed in both eyes, although more pronounced in the left, and only appearing when covering one eye. There was bilateral IOOA (+3) and a significant V-pattern. A positive Bielschowsky tilt test was found in both sides[7] (Figure 1A).
Case 2: The patient’s BCVA was 1.0 in both eyes, with refractions of −3.00 for the right and +3.00 +0.25 × 65° for the left eye. Exodeviation and hypertropia were highly variable due to significant dissociated horizontal deviation[8] in the left eye and DVD in the right. Exotropia of 10-20∆ and right hypertropia of 15-30∆ were observed on alternate prism cover test in the primary position at distance and near. She had latent nystagmus in both eyes and an anomalous head posture. There was unilateral superior oblique underaction (−2) along with IOOA (+2) in the right eye, and a positive Bielschowsky tilt test on the right-hand side (Figure 2A).
The final diagnosis for both cases were DVD with SOP.
Levofloxacin eye drops were applied to prevent infection in both eyes 2 d before the surgery. With the patient and her mother’s consent, she underwent the modified unilateral IOAT with lateral rectus recession (5 mm) and medial rectus resection (4 mm) in her left eye under general anesthesia.
The anterior-nasal fibers of the left IO were attached at 9 mm posterior to the corneal limbus along the temporal board of the left IR, and the posterior fibers were attached a further 5 mm temporal to the first suture using an absorbable 6/0 suture. The left lateral rectus (LR) was backward to 5 mm from the original insertion site and the left medial rectus was resected about 4 mm and re-sutured to the original insertion site using an absorbable 6/0 sutures. At the end of the surgery, the surgeon applied tobramycin dexamethasone ointment to the left eye, bandaged it and waited for the patient to wake up before sending the patient back to the ward. After the surgery, the patient was instructed to apply levofloxacin eye drops and tobramycin dexamethasone drops to the left eye.
Levofloxacin eye drops were applied to prevent infection in both eyes 2 d before the surgery. With the patient and her mother’s consent, she underwent the modified unilateral IOAT in her right eye with lateral rectus recession 7 mm in her left eye under general anesthesia.
The anterior-nasal fibers of the right IO were attached at 9 mm posterior to the corneal limbus along the temporal board of the right IR, and the posterior fibers were attached a further 5 mm temporal to the first suture using an absorbable 6/0 suture. The left LR was backward to 7 mm from the original insertion site using an absorbable 6/0 suture. At the end of the surgery, the surgeon applied tobramycin dexamethasone ointment to both eyes, bandaged them and waited for the patient to wake up before sending the patient back to the ward. After the surgery, the patient was instructed to apply antibiotic eye drops to the both eyes.
SOP is the most common paralysis of single cyclovertical muscle and is the fourth cranial nerve (trochlear nerve) palsy, which involves the SO[9]. The incidence of SOP is approximately 12.9 (95% confidence interval 9.0–16.9) per 100000 adolescents younger than 19 years of age[10] and 54.1 (95% confidence interval 50.2–58.0) per 100000 adults[11]. In SOP, there is hypertropia of the paralytic eye with abnormal head position. Examination of version shows underaction of the SO and overaction of the antagonist IO. The main surgical methods are to weaken the antagonist muscle of the paralytic muscle; to weaken the yoke muscle of the another eye; to strengthen the paralytic muscle; and to weaken the superior rectus (SR) of the paralytic eye[9]. DVD is an innervation disorder which occurs in more than 50% of infantile strabismus[12]. The main clinical feature is either eye slowly drifting upward and outward with extortion when occluded. Traditional surgical treatment for DVD focuses on the SR recession, and for patients with IOOA, IOAT is also considered[13].
By displacing the IO insertion to anterior to the temporal insertion site of the IR (Elliott point) in a crossed-swords manner, IOAT was more effective improvement of IOOA and DVD compared with the standard recession of IO[6]. This IOAT has been widely employed; however, the risks of overaction and AES were high, especially in unilateral IOAT (more than half). AES is an elevation restriction in abduction, that might be contributed by both suturing the IO anterior to the IR insertion, and spreading the posterior lateral corner of the IO out temporally[14].
Stager[15,16] established that the neurovascular bundle of the IO was an ancillary origin of the posterior-temporal fibers of the IO following IOAT for limiting eye upturn, and the neurofibrovascular bundle attaches to the IO 2 mm temporal to the IR, 12 mm from the insertion of the IO. Based on the autopsy results from cadaveric eyes by Apt L[17], the temporal length of the IO was about 14 mm, so the Elliott point might increase the risk of excessive muscle tension of temporal IO fibers. Kushner[18] suggested that AES might be an “innervational restriction,” as opposed to a mechanical restriction and appears to be caused by tautness of the lateral fibers of the transposed IO. Therefore, they sutured the anterior nasal corner of the IO to the temporal corner of the IR insertion and let the posterior temporal corner hang back. This approach is better for preventing AES, but less powerful for reducing DVD.
To avoid AES, some have suggested that the insertion line should be oriented parallel to the IR axis, the anterior IO nasal fibers should be at or just (≤ 2 mm) anterior to the temporal IR insertion in a “crossed-swords” manner, and the posterior temporal fibers should be folded and buried under the fixed anterior IO nasal fibers[19]. This transposition has been seen to weaken mild to moderate IOOA and correct small primary position hypertropia. Guemes and Wright[20] suggested that the bilateral graded IOAT was effective in normalizing versions and correcting vertical deviations in primary position, and the new insertion (the temporal insertion site of the IR or 1-2 mm behind) line perpendicular to the IR axis with a “J” deformity for the IOOA combined with DVD (6 to 15 PD), without long-term observation of complications.
Thus, the reattachment points and attachment line directions are the key factors affecting operative outcomes and complications. Based on the above study, we chose a new anterior transposition to 9 mm posterior to the corneal limbus along the temporal board of the IR to reduce the risk of AES, with the wider insertion (about 5 mm) perpendicular to the IR axis to enhance the orthotic effects on vertical strabismus and spontaneous upward drifting.
The basic idea of IO transposition surgery according to the degree of IOOA is gradually moving the insertion of the IO anteriorly; if 1-mm anterior IR insertion still does not sufficiently improve the vertical strabismus and spontaneous upward drifting, a new line of attachment perpendicular to the IR insertion will be used. This surgical approach chose the new insertion line perpendicular to the IR axis to decline the upward drift of the DVD and vertical strabismus, weakening the effect of the anterior transposition of the new insertion of the IOAT, thus preventing the onset of AES. This approach ensured surgical effectiveness and prevented the onset of AES, especially after unilateral surgery.
Other advantages to this version of the IOAT procedure is that using the limbus as a reference point is more accurate and reasonable than the IR, and nasal transposition is not necessarily required which reduces operating difficulty.
In the cases presented here, the modified unilateral IOAT improved the patients’ primary position hypertropia and superior floating phenomenon, with no obvious postoperative anti-elevation syndrome and no significant effect on lower lid configuration and function for 1 year. Therefore, this procedure is an effective and safe surgical methodfor t reating DVD with SOP. Certainly, more data are required to corroborate these findings and a controlled comparative study is necessary to draw definitive conclusions. In addition, a cohort study is in progress to better assess the procedure.
Thanks to Professor Ze Wang for his valuable advice on surgical design and article writing.
| 1. | Yang SH. Dissociated vertical deviation and paralytic vertical strabismus. Zhongguo Xieshi Yu Xiaoer Yanke Zazhi. 2010. [DOI] [Full Text] |
| 2. | Yang HK, Kim JH, Hwang JM. Congenital superior oblique palsy and trochlear nerve absence: a clinical and radiological study. Ophthalmology. 2012;119:170-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Cho YA, Kim JH, Kim S. Antielevation syndrome after unilateral anteriorization of the inferior oblique muscle. Korean J Ophthalmol. 2006;20:118-123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Kushner BJ. The effect of anterior transposition of the inferior oblique muscle on the palpebral fissure. Arch Ophthalmol. 2000;118:1542-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Gobin MH. Anteroposion of the inferior oblique muscle in V-esotropia. Ophthalmologica. 1964;148:325-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Elliott RL, Nankin SJ. Anterior transposition of the inferior oblique. J Pediatr Ophthalmol Strabismus. 1981;18:35-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 92] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Wright KW, Yi N. Torticollis, Nystagmus and Incomitant Strabismus. In: Color Atlas Of Strabismus Surgery: Color Atlas Of Strabismus Surgery. New York: Springer New York, 2015: 52-55. |
| 8. | Brodsky MC. Dissociated horizontal deviation: clinical spectrum, pathogenesis, evolutionary underpinnings, diagnosis, treatment, and potential role in the development of infantile esotropia (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007;105:272-293. [PubMed] |
| 9. | Chang MY, Coleman AL, Tseng VL, Demer JL. Surgical interventions for vertical strabismus in superior oblique palsy. Cochrane Database Syst Rev. 2017;11:CD012447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Tollefson MM, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood hypertropia: a population-based study. Ophthalmology. 2006;113:1142-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Martinez-Thompson JM, Diehl NN, Holmes JM, Mohney BG. Incidence, types, and lifetime risk of adult-onset strabismus. Ophthalmology. 2014;121:877-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 100] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 12. | The American Academy of Ophthalmology. Section 06: Pediatric Ophthalmology and Strabismus. In 2018-2019 Basic and Clinical Science Course (BCSC). San Francisco: The American Academy of Ophthalmology, 2019: 129-130. |
| 13. | Hatt SR, Wang X, Holmes JM. Interventions for dissociated vertical deviation. Cochrane Database Syst Rev. 2015;2015:CD010868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Kushner BJ. Restriction of elevation in abduction after inferior oblique anteriorization. J AAPOS. 1997;1:55-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 73] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Stager DR. Costenbader lecture. Anatomy and surgery of the inferior oblique muscle: recent findings. J AAPOS. 2001;5:203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Stager DR. The neurofibrovascular bundle of the inferior oblique muscle as the ancillary origin of that muscle. J AAPOS. 1997;1:216-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Apt L, Call NB. Inferior oblique muscle recession. Am J Ophthalmol. 1978;85:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 49] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Kushner BJ. How to Perform Superior Surgery on the Inferior Oblique and Avoid Inferior Surgery on the Superior Oblique. In: Strabismus: Practical Pearls You Won't Find in Textbooks. Switzerland: Springer Nature, 2017: 221-231. |
| 19. | Jeon H, Kwon H, Choi HY. Modified anterior transposition of the inferior oblique muscle. J AAPOS. 2018;22:361-365.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Guemes A, Wright KW. Effect of graded anterior transposition of the inferior oblique muscle on versions and vertical deviation in primary position. J AAPOS. 1998;2:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bernardes A, Portugal; Nambi G, Saudi Arabia S-Editor: Hu YR L-Editor: A P-Editor: Cai YX