Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2753
Peer-review started: February 19, 2023
First decision: February 28, 2023
Revised: March 6, 2023
Accepted: March 24, 2023
Article in press: March 24, 2023
Published online: April 26, 2023
Processing time: 65 Days and 13.1 Hours
Although metaphyseal ulnar shortening osteotomy (MUSO) is safer for the treatment of ulnar impaction syndrome (UIS) than diaphyseal ulnar shortening osteotomy (DUSO), DUSO is widely used for UIS treatment.
To evaluate the effectiveness of DUSO and MUSO for UIS treatment and determine the factors that should be considered when choosing surgical treatment for UIS.
Articles comparing the effectiveness of DUSO and MUSO for UIS treatment were systematically retrieved from MEDLINE (Ovid), PubMed, EMBASE, and Cochrane Library. The demography, incidence of complications, secondary operation rate, postoperative DASH score, wrist pain on the visual analogue scale, and grip strength improvement were also evaluated. In addition, the correlation between the improvement of grip strength and the shortening of osteotomy length of ulna was analyzed. The outcome of the patient was discontinuous, and the odds ratio, risk ratio (RR), and 95%CI were calculated and analyzed via RevMan5.3 software.
Six studies, including 83 patients receiving MUSO (experimental group) and 112 patients receiving DUSO (control group), were included in the meta-analysis. The second operation rate was significantly higher after DUSO than after MUSO. The DASH scores were slightly lower in the MUSO group than in the DUSO group. The patients receiving MUSO had slightly better pain relief effect than patients receiving DUSO. However, the incidence of complications and improvement of grip strength were not significantly different between the two groups.
Although DUSO and MUSO provide similar effects for UIS, MUSO is associated with a lower secondary operation rate, slightly lower postoperative DASH scores and slightly better pain relief effect than DUSO, indicating that MUSO can effectively be used for UIS treatment.
Core Tip: Ulnar impaction syndrome (UIS) is caused by overload of the ulnar wrist joint. This is the common cause of ulnar wrist pain. UIS is related to static or dynamic lateral positive change. If not treated in time, it may lead to the erosion and perforation of the triangular fibrocartilage complex, as well as the degeneration of the triangular, Lunate or ulnar head cartilage. Therefore, the basic treatment of UIS includes mechanical decompression of the overloaded ulnar wrist joint by reducing the ulnar variation. There are many surgical treatments that can reduce the excessive pressure on the ulnar side of the wrist joint, including diaphyseal ulnar shortening osteotomy (DUSO), thin section resection and metaphyseal ulnar shortening osteotomy (MUSO). The Wafer resection site of the distal ulna belongs to MUSO. Compare the effect of DUSO and MUSO ulnar shortening methods. In fact, both of these operations have specific advantages and disadvantages. It should be clear whether the treatment choice of UIS patients depends on the preferences of surgeons.
- Citation: Deng HL, Lu ML, Tang ZM, Mao QL, Zhao JM. Is metaphyseal ulnar shortening osteotomy superior to diaphyseal ulnar shortening osteotomy in the treatment of ulnar impaction syndrome? A meta-analysis. World J Clin Cases 2023; 11(12): 2753-2765
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2753.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2753
Ulnar impaction syndrome (UIS) is a common cause of ulnar-sided wrist pain caused by overload through the ulnocarpal joint. UIS is associated with static or dynamic ulnar positive variance[1,2] and may lead to erosion and perforation of triangular fibrocartilage complex (TFCC) and degeneration of triangular, lunate or ulnar head cartilage if not timely treated[3,4]. The basic UIS treatment involves mechanical decompression of overloaded ulnocarpal joint by decreasing ulnar variance. Many surgical treatments, including diaphyseal ulnar shortening osteotomy (DUSO), wafer resection, and metaphyseal ulnar shortening osteotomy (MUSO), can be used to reduce excessive pressure on the ulnar side of the carpus[5-11]. MUSO is usually performed at the Wafer resection site of the distal ulna. Nonetheless, both DUSO and MUSO have specific advantages and disadvantages[9-13].
Although UIS is usually associated with positive ulnar variance, UIS has been found in patients with neutral or negative ulnar variance. Furthermore, the thickness of TFCC is inversely associated with ulnar variance[1,2]. Previous studies have reported that TFCC debridement alone cannot relieve ulnar wrist pain caused by significant positive ulnar variance or other carpal lesions[14-16]. Besides, positive ulnar variance may increase the risk of TFCC wear or perforation. Bernstein et al[4] showed that arthroscopic TFCC debridement combined with USO can effectively treat UIS. However, Saito et al[17] indicated that ulnar variance may affect the results of TFCC debridement. Therefore, USO can biomechanically unload the ulnocarpal joint and relieve the ulnar wrist pain associated with UIS. Compared with arthroscopic TFCC debridement combined with USO, arthroscopic TFCC debridement combined with wafer distal ulna resection is a more minimally invasive treatment with less secondary surgery rate and tendonitis.
DUSO is a common USO widely used to treat UIS since it can satisfactorily relieve ulnar wrist pain[18,19]. Diaphyseal is the most common site of osteotomy. However, DUSO is associated with many complications, including implant removal[20], catastrophic delayed union or nonunion at the osteotomy site[20-25], postoperative tendinitis[26,27], and accidental residual positive variance[26]. Besides, the position of the plate on the surface of the metacarpal or dorsal ulna may cause different regional responses, such as postoperative tendinitis, symptomatic hardware, and hardware stimulation. Compared with DUSO, MUSO has fewer complications. Nonetheless, MUSO is associated with some complications. Some studies have also shown that DUSO and MUSO have similar treatment effects[1-6,8]. The morphology of the inferior radioulnar joint (DRUJ) can affect the effect of USO for UIS treatment[3]. DRUJ arthritis after USO may cause ulnar wrist pain and even impair wrist function due to the incoordination of DRUJ[28-31]. MUSO is associated with better ulnar wrist pain relief, lower bone nonunion rate, and lower secondary operation rate. However, Claes et al[32] showed that metaphyseal and diaphysis fracture healing follows similar biomechanical progress. Smoking and the site of osteotomy also affect the outcome of postoperative pain relief[33]. Cha et al[34] recommend that patients with osteoporosis in UIS should avoid using DUSO since delayed union or nonunion occasionally occurs after DUSO.
However, it is unknown whether any factor should be considered when choosing DUSO or MUSO for UIS treatment or whether it should be based on surgeon’s decision only. This meta-analysis aimed to assess the effects of DUSO and MUSO for UIS treatment and determine preoperative factors that surgeons should carefully consider when selecting DUSO and MUSO for UIS treatment.
Cochrane Library, MEDLINE (Ovid), PubMed, and EMBASE databases were searched on September 7, 2019, following the Reporting Items for Systematic Reviews and Meta-Analyses guideline[35]. A manual search was also conducted on the relevant research to ensure that no research was omitted.
The key words applied in the literature search are shown in Table 1. The abbreviations "AWP" and "USO" were also used during the search. The keywords were limited to titles and abstracts to ensure a more accurate search for target research.
| Search items |
| Metaphyseal osteotomy and diaphyseal osteotomy |
| Distal metaphyseal ulnar shortening osteotomy and diaphyseal ulnar shortening osteotomy |
| Arthroscopic wafer procedures and ulnar shortening osteotomy |
| Wafer procedures and ulnar shortening osteotomy |
| Arthroscopic distal ulna resections and ulnar shortening osteotomy |
Inclusion criteria: (1) Studies reporting treatment outcomes of UIS and comparing distal MUSO and DUSO for UIS treatment; (2) Studies with patients aged 15-80 years; and (3) Reports with at least one of the following results: ulnar variance, visual analog scale (VAS) pain score, Quick DASH score, contralateral grip strength, incidence of complications, and incidence of secondary surgery.
Exclusion criteria: (1) Studies not comparing distal MUSO and DUSO for UIS treatment; (2) Studies only reporting the results of UIS's DUSO or MUSO; and (3) Duplicates and studies on cadavers, animals, and children (below 14 years). Notably, all research designs were eligible, and exclusion was not based on methodological quality.
UIS patients with or without degenerative TFCC tears and patients diagnosed with ulnocarpal abutment syndrome since ulnocarpal abutment syndrome has the same symptoms as UIS (Table 2).
| Ref. | Types of participants | Selected outcomes |
| Bernstein et al[4], 2004 | MUSO vs DUSO | Ulnar variance; VAS; grip strength; complication rate; secondary procedure rate |
| Marquez-Lara et al[12], 2017 | MUSO vs DUSO | Secondary procedure rate; complication rate; quick DASH score |
| Sennwald et al[10], 2013 | MUSO vs DUSO | Ulnar variance; VAS |
| Constantine et al[41], 2000 | MUSO vs DUSO | Secondary procedure rate; complication rate |
| Smet et al[11], 2014 | MUSO vs DUSO | Secondary procedure rate; complication rate; quick DASH score |
| Oh et al[9], 2018 | MUSO vs DUSO | Secondary procedure rate; complication rate; quick DASH score |
The following information was analyzed: (1) Ulnar variance; (2) Pain score: VAS score; (3) Quick DASH score: quick disabilities of the arm, shoulder, and hand questionnaire scores; (4) Grip strength of the unaffected side; (5) Complication rates: Complication was defined as the need for a subsequent surgical procedure after the first operation. The complication rates were calculated by dividing the number of complications by the number of patients. The patients were treated using a Sauvé-Kapandji procedure. Nonunion patients were treated with iliac crest bone grafting, cubital tunnel release, tendon graft stabilization of the DRUJ. Some patients were treated with arthrolysis of the DRUJ, wrist arthrodesis, osteosynthesis for nonunion of the ulna, refixation for refracture of the ulna, removal of the fixation device for hardware-produced irritation, secondary surgery for unrelieved symptoms, and TFCC repair for iatrogenic rupture of the TFCC during the AWP. Additional complications included the requirement for hospital admission and antibiotics to treat an infection, the presence of an iatrogenic neurovascular deficit or tendinopathy, and the detection of arthritic changes via radiography combined with symptoms, extensor carpi ulnaris tendinitis, hardware loosening, and regional pain; and (6) Secondary procedure rate: Hardware removal, resection ulnocarpal scar, arthrolysis of the DRUJ, arthrodesis, refixation for refracture of the ulna.
Two authors (Deng HL and Lu ML) conducted a systematic electronic search. Duplicates were excluded first, then the authors reviewed the titles and abstracts step by step. Finally, two other authors (Zhao JM and Tang ZM) conducted a full-text review of the identified articles following the inclusion and exclusion criteria. The following data were extracted: Year of publication, name of the author, type of article, average age and gender distribution, type of operation, type of enrollment (experimental group and control group), number of patients in each group, ulnar variance, pain score, Quick DASH score, grip strength, incidence of complications and incidence of secondary operation. In addition, factors that may affect healing (delayed union or nonunion) and pain relief, such as smoking status, osteoporosis, and preoperative use of painkillers, were recorded.
Only the literature related to the efficacy of DUSO and MUSO in IUS treatment was retrieved. The selection of the studies was performed step by step through title, abstract, and full-text review following the predetermined inclusion and exclusion criteria. Non-English published studies were translated before reviewing the reference part of the article. Two reviewers (Tang ZM and Mao QL) made research choices and resolved any differences in the inclusion of the articles through discussion and further review.
Discontinuous data were used for comparison analysis. Odds ratio (OR), risk ratio (RR), and 95%CI were used for (The Cochrane Collaboration, Oxford, UK) for final analysis via RevMan5.3 software. The sources of heterogeneity between studies were assessed in a step-by-step manner. In addition, heterogeneity was extracted for subgroup analysis. A random effects model was used for moderate to high heterogeneity (I2 value > 50%), while fixed effects model was used for low heterogeneity (I2 value < 50%). Pain relief between subgroups was also compared based on ulnar shortening osteotomy of different lengths. The pain score (VAS) and grip strength improvement were compared using a two-sample t-test. A two-sample t-test was also used to analyze the difference of grip strength improvement between different lengths of ulnar shortening osteotomy. The relationship between the length of ulnar osteotomy and grip strength improvement was evaluated using linear regression analysis. Data were expressed as mean ± SD, and the significance level was set at 0.05.
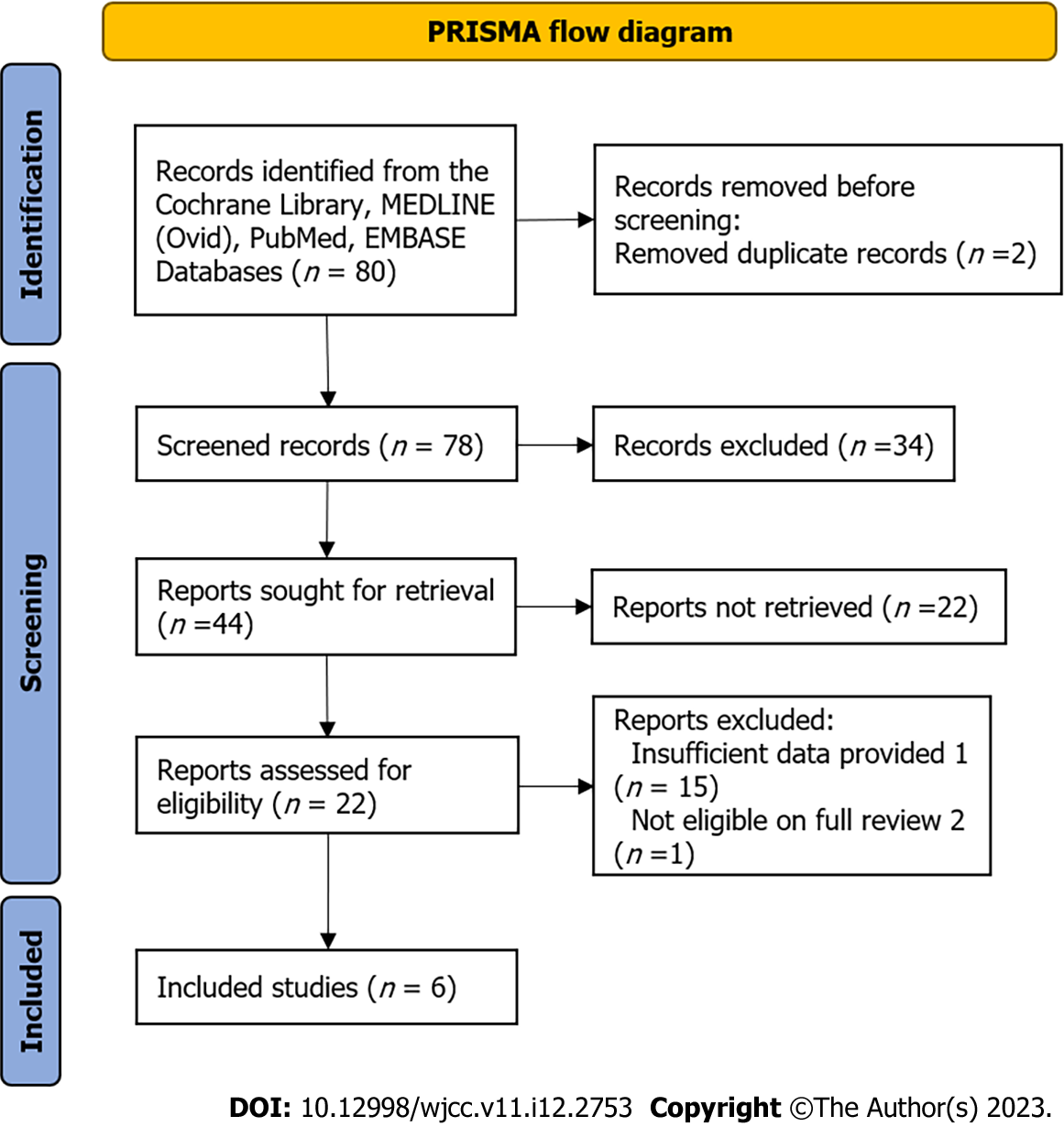
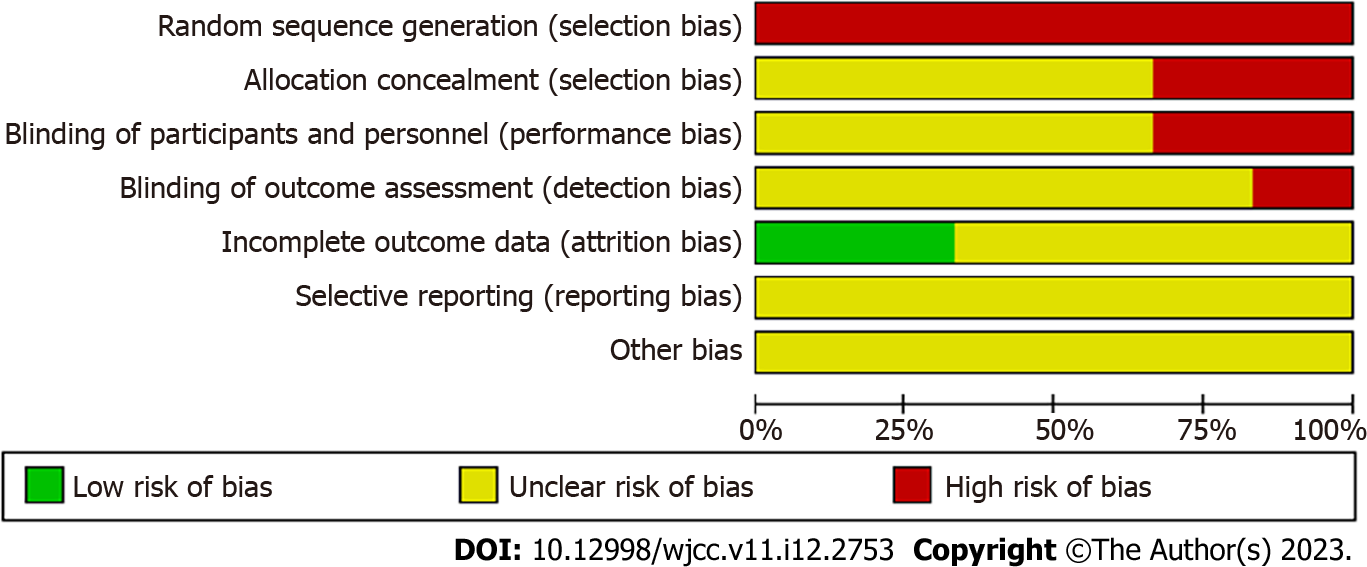
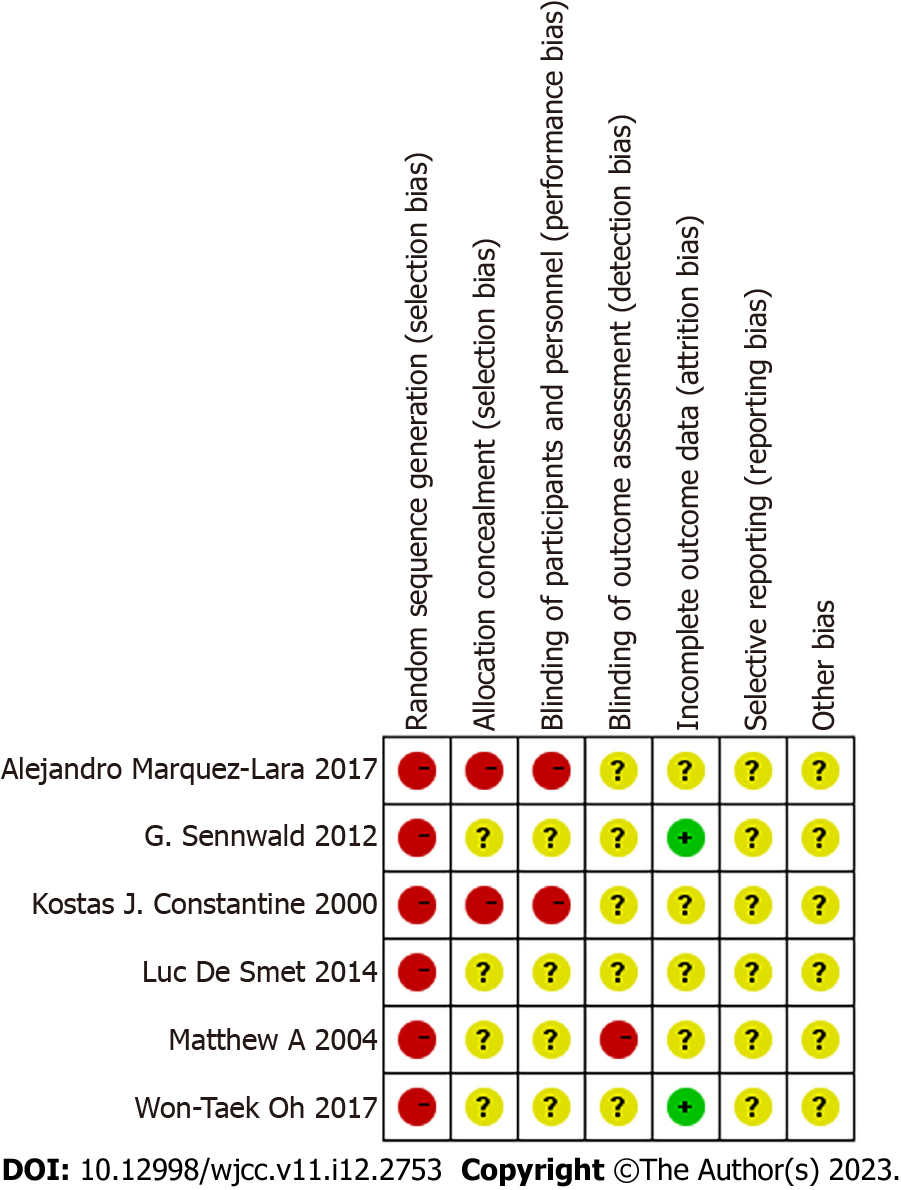
The search results are presented in Figure 1. A total of 80 articles were initially identified from the electronic databases, of which only 44 were considered potentially relevant. A total of 22 of 44 potentially relevant articles were excluded after a careful evaluation of the title and abstract. Also, 15 of the remaining 22 studies were excluded after reviewing full-text studies because they did not provide sufficient data for meta-analysis, and 1 was excluded because it was a systematic review. Finally, six independent studies were included in the final analysis. The bias risk map is shown in Figure 2, and the summary of bias risk is shown in Figure 3.
The main features (study time, number of patients, gender, age, follow-up time, time since the first onset of clinical syndrome, and intervention of participants) are shown in Table 3. The included studies had 195 patients, of which 83 received MUSO (experimental group) and 112 received DUSO (control group) (Table 3). The six studies included 82 men and 113 women with an average age of 43.9 years. The average follow-up period of the included studies was about 31.7 mo. Three studies provided preoperative intervals (mo).
| Ref. | No. of patients | Gender (male/female) | Age (mean yr) | Follow-up time (mo) | After injury (mo) | No. of patients who underwent MUSO | No. of patients who underwent DUSO |
| Bernstein et al[4], 2004 | 27 | 13/14 | 37.6 | 17.4 | 13.8 | 11 | 16 |
| Marquez-Lara et al[12], 2017 | 35 | 17/18 | 43.9 | 18.5 | Not reported | 14 | 21 |
| Sennwald et al[10], 2013 | 29 | 45277 | 42.9 | 54 | 5.5 | 16 | 13 |
| Constantine et al[41], 2000 | 22 | 45152 | 40.5 | 36 | Not reported | 11 | 11 |
| Smet et al[11], 2014 | 40 | 45229 | 40.4 | 29 | Not reported | 12 | 28 |
| Oh et al[9], 2018 | 42 | 17/25 | 53.6 | 35.5 | 29.5 | 19 | 23 |
Some original studies did not provide baseline factors focusing on the comparison. The studies showed that the amount of ulnar shortening osteotomy had a linear relationship with the improvement of grip strength. However, the included studies did not provide raw data for analysis of the aspects of interest since each had different objectives. Therefore, the aspects were analyzed based on the information provided by the included studies. The preoperative ulnar variance, VAS, and contralateral grip strength are shown in Table 4. The preoperative ulnar variance, VAS, and grip strength improvement were not significantly different between the experimental and the control groups. The demographic characteristics of the production subgroup are shown in Table 5. These characteristics were used to analyze the selected results of VAS and grip strength between the MUSO and DUSO groups.
| Ref. | Preoperative ulnar variance (mm) | Pain score (VAS) | Grip strength of the unaffected side (%) | Selected outcomes |
| Bernstein et al[4], 2004 | 1.5 | Not reported | 55.2 | Ulnar variance; VAS; grip strength; complication rate; secondary procedure rate |
| Marquez-Lara et al[12], 2017 | 3.9 | 6.5 | Not reported | Secondary procedure rate; complication rate; quick DASH score |
| Sennwald et al[10], 2013 | 2.6 | 8 | Not reported | Ulnar variance; VAS |
| Constantine et al[41], 2000 | 2 | Not reported | Not reported | Secondary procedure rate; complication rate |
| Smet et al[11], 2014 | 2 | Not reported | Not reported | Secondary procedure rate; complication rate; quick DASH score |
| Oh et al[9], 2018 | 2.9 | 5.9 | 54.1 | Secondary procedure rate; complication rate; quick DASH score |
| Ref. | Preoperative ulnar variance (mm) | Pain score (VAS) | Grip strength of the unaffected side (%) | Selected outcomes |
| Bernstein et al[4], 2004 | 1 | Not reported | 54/56 | Ulnar variance; VAS; grip strength; complication rate; secondary procedure rate |
| Marquez-Lara et al[12], 2017 | 1.285714 | 6.64/6.45 | Not reported | Secondary procedure rate; complication rate; quick DASH score |
| Sennwald et al[10], 2013 | 0.666667 | 7.3/8.2 | Not reported | Ulnar variance; VAS |
| Constantine et al[41], 2000 | 0.6 | Not reported | Not reported | Secondary procedure rate; complication rate |
| Smet et al[11], 2014 | 1.588235 | Not reported | Not reported | Secondary procedure rate; complication rate; quick DASH score |
| Oh et al[9], 2018 | 1.034483 | 5.8/6.0 | 51/ 59 | Secondary procedure rate; complication rate; quick DASH score |
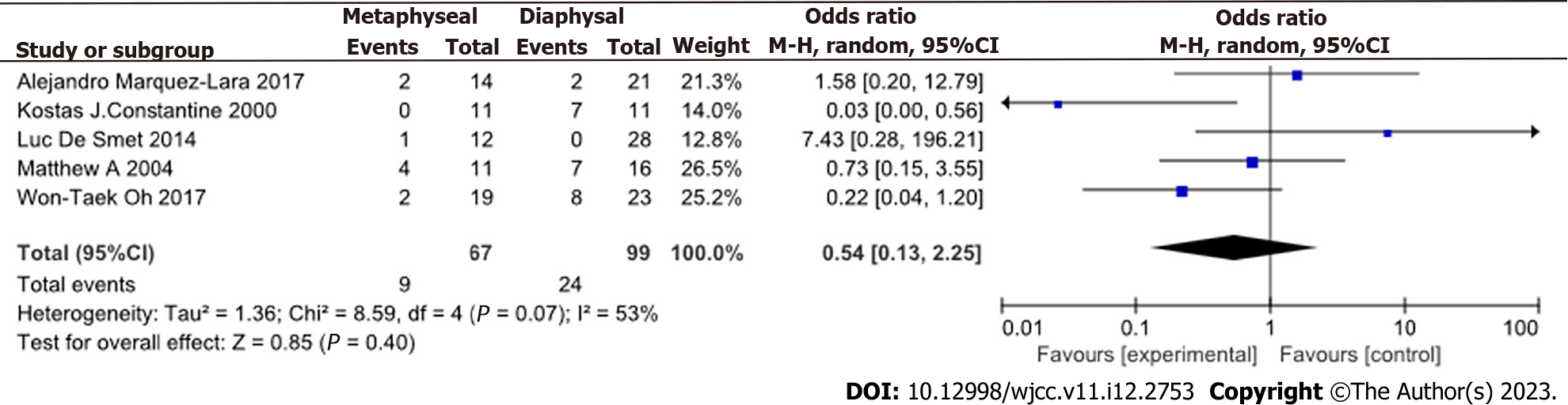
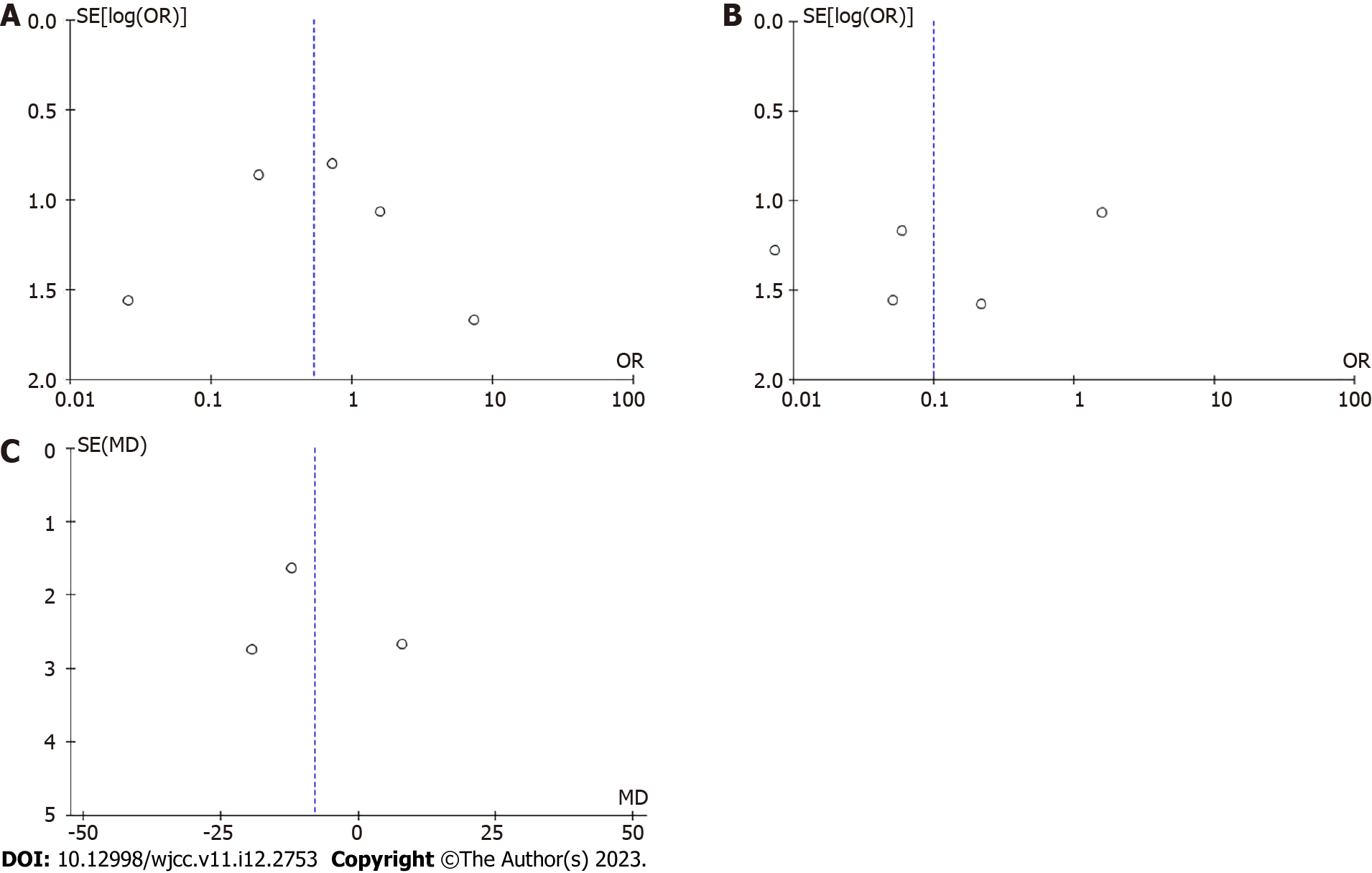
The incidence of complications was slightly higher in the DUSO group than in the MUSO group (Figure 4) (OR = 0.54, 95%CI: 0.13-2.25, P > 0.05, I2 = 53%). The funnel chart showing the incidence of complications is shown in Figure 5A.
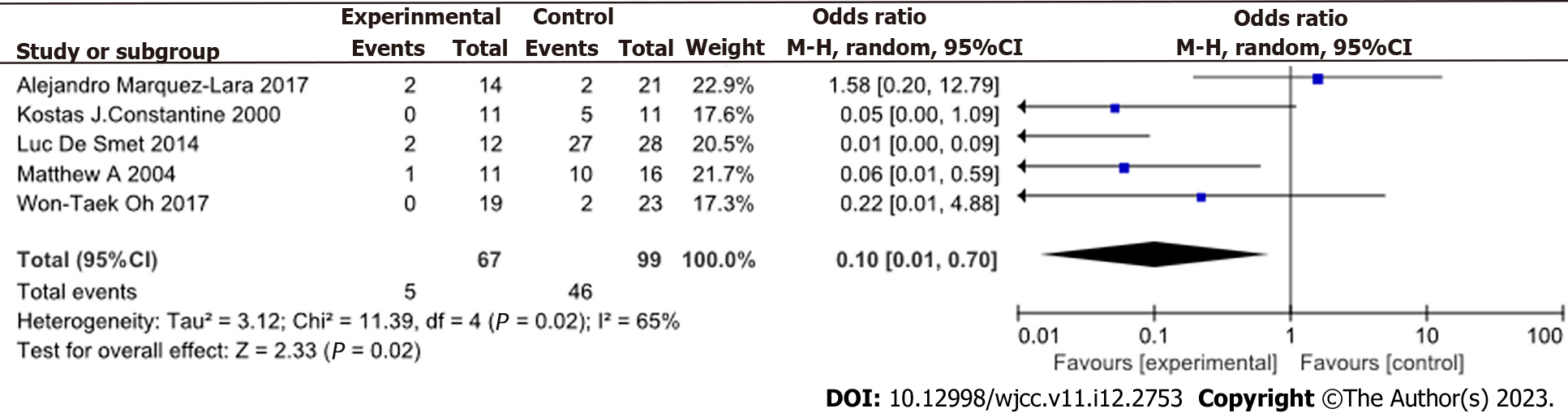
The secondary operation rate was lower in the MUSO group than in the DUSO group (OR = 0.10, 95%CI: 0.01-0.70, P < 0.05, I2 = 65%) (Figure 6). Funnel plot showing the secondary procedure rate is shown in Figure 5B.
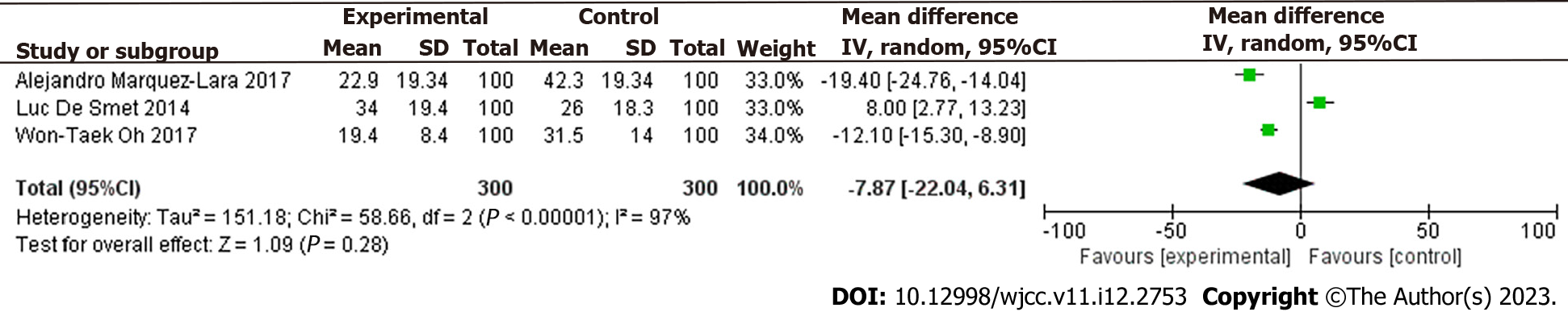
The postoperative DASH score was slightly lower in the MUSO group than in the DUSO group OR =
Two sample t-test showed that the postoperative VAS was slightly lower in the MUSO group than in the DUSO group (T = −0.978, P > 0.05).
Two sample t-test showed that the postoperative grip strength of the unaffected extremity was not significantly different between the two groups (T = 0.252, P > 0.05). Two sample t-test was also applied to compare postoperative grip strength outcomes between two common lengths of ulnar shortening osteotomy (2.5-mm and 3.0-mm USO). The postoperative grip strength outcomes were not significantly different between the 2.5-mm and 3.0-mm groups (P > 0.05). However, the pre- and postoperative percentages of grip strength of the contralateral wrist were significantly different between the two groups. Specifically, grip strength improved by 32% and 28% in the MUSO group (P < 0.05) and DUSO group (P < 0.05), respectively. Linear regression analysis showed that the length of ulnar osteotomy was not significantly associated with grip strength improvement based on Bernstein et al[4] study (F = 0.194 P > 0.05)
To the best of our knowledge, this is the first meta-analysis comparing effectiveness of MUSO and DUSO in UIS treatment. The effects of MUSO and DUSO in UIS treatment are controversial. In this study, the incidence of complications, postoperative DASH scores, pain VAS results, and improved grip strength were similar between the DUSO and MUSO groups. However, the rate of secondary operation was lower after MUSO than after DUSO.
The improvement of grip strength should be evaluated as a percentage of contralateral wrist between groups based on the preoperative and postoperative grip strength. Nonetheless, some studies have reported postoperative grip strength as a percentage of the contralateral wrist. Herein, data from Bernstein et al[4] showed that the grip strength improvement was not significantly different between the 2.5-mm and 3.0-mm ulnar shortening lengths (P = 0.336). Quadlbauer et al[36] also is reported that positive ulnar variance caused by distal radius fracture is associated with decreased grip strength. These studies showed that USO unloading ulnar-wrist hypertension can treat UIS[37]. Furthermore, results showed that preoperative or postoperative pain was not correlated with the degree of ulnar variance, indicating that preoperative ulnar variance should not be considered for procedural decision-making. Bernstein et al[4] suggested that the change of ulna should be reduced to -2.5mm after the operation. Furthermore, the improvement in grip strength was not significantly different between the MUSO group and the DUSO group. Moreover, preoperative and postoperative grip strength were significantly different between the two groups (P < 0.05). Bernstein et al[4] did not analyze the relationship between ulna shortening and grip strength improvement in different lengths. DUSO is associated with high nonunion rate. Schmidle et al[38] promoted bone healing at the osteotomy site using ulnar osteotomy locking plate. The surgical method improves the healing rate of DUSO mainly in the following aspects: (1) Oblique osteotomy expands the bone contact surface of osteotomy; (2) guide saw makes osteotomy more accurate than manual osteotomy; and (3) slide hole design plate can easily close the osteotomy gap and tension screw to compress the osteotomy surface. Meanwhile, Terzis et al[39] recently reported that USO can achieve a 100% healing rate using similar saw blade guide plates and slide hole design plates for the treatment of symptomatic UIS after distal radius fractures. The difference in complication rates between DUSO and MUSO for the treatment of ulnar impaction syndrome has gradually reduced due to the improvement of the instrument and the development of DUSO[37,40]. MUSO and DUSO for UIS treatment may depend on surgeon preference. Although many surgeons prefere DUSO, MUSO may be more suitable for UIS patients with osteoporosis, nonunion risk[23,24], and smoking history[33]. Besides, DUSO patients may be at risk of a second fracture at the osteotomy site after plate removal. Terzis et al[39] showed that excessive ulnar shortening is postoperative risk factor for distal radioulnar joint inconsistency, leading to the development of osteoarthritis. Nuñez et al[33] indicated that the amount of ulnar shortening is balanced with soft tissue. Besides, ulnar shortening should obtain ulnar variance from 0 to 2 mm, indicating that ulnar change larger than 4 mm is suitable for DUSO.
In this study, the pain relief was slightly better in the MUSO than in the DUSO group, inconsistent with Nuñez et al[33]'s study. Specifically, Nuñez et al[33] found that tobacco use and preoperative opioid consumption are risk factors for pain after osteotomy and thus can act as predictors of pain relief. Nuñez et al[33] performed MUSO at distal metaphyseal of ulna to repair the radius-ulnar level (negative variance of the ulna after MUSO; 1-2 mm). Finally, the ulnar osteotomy site at the metaphysis was completely closed, and osteotomy site was fixed with the distal ulnar hook plate[33]. Diaphyseal osteotomy is an extra-articular operation where the pressure of the distal ulnar wrist joint is removed without affecting the distal ulnar wrist joint pressure and radioulnar joint (DRUJ) function. However, diaphysis osteotomy can damage the distal interosseous membrane and cause postoperative tendinitis because of the diaphysis plate. Metaphyseal osteotomy is suitable for the reconstruction of the TFCC fovea attachment and the shortening of the ulna, indicating that MUSO may be more minimally invasive. Wrist arthroscopy-assisted MUSO should start at the tip of the ulnar styloid process, followed by a longitudinal incision of 6-8 cm to the proximal end for the treatment of TFCC injury with ulnar impaction because TFCC attachment avulsion is usually combined with UIS[33]. Compared with wrist arthroscopy-assisted DUSO, minimally invasive method is significantly effective for the treatment of ulnar impaction with TFCC injury. The incision of wrist arthroscopy-assisted DUSO may be larger than 12 cm. Although DUSO and MUSO are both extra-articular surgeries, they may lead to radiologically visible degenerative changes in DRUJ[34]. Cha et al[34] indicated that surgeons should inform patients with type III DRUJ before surgery and the potential risk of changes in DRUJ arthritis. Nonetheless, the relationship between radiological degeneration of DRUJ and USO of UIS is unclear. The removal of the ulnar head is usually performed at the dome of the ulnar head or near the metaphyseal bone. Arthroscopic discectomy involves the removal of the dome of the ulnar head or moving ulnar head, mechanically decompressing the ulnocapal joint load[41], thus avoiding DRUJ damage. Postoperative wrist pain may be caused by pressure tension of ulnocarpal interosseous ligament due to excessive osteotomy. The tensioned ulnocapal ligament, especially at DRUJ, increases the risk of arthritis in DRUJ. Arthroscopic wafer resection has an advantage at the intra-articular ulnar head, making it superior to DUSO or MUSO since it reduces the risk of arthritis changes in DRUJ[4,9,11,41].
DUSO is associated with a higher secondary procedure rate[4,9,11,41], especially the removal of the plate. DUSO is also associated with a risk of a second fracture at the osteotomy site after plate removal. Although DUSO and MUSO have similar effect for UIS treatment, MUSO is associated with a lower secondary procedure rate, slightly lower postoperative DASH score, and slightly better pain relief, and thus is suitable for UIS treatment.
Although metaphyseal ulnar shortening osteotomy (MUSO) is safer for the treatment of ulnar impaction syndrome (UIS) than diaphyseal ulnar shortening osteotomy (DUSO), DUSO is widely used for UIS treatment.
It is unknown whether any factor should be considered when choosing DUSO or MUSO for UIS treatment or whether it should be based on surgeon’s decision only. This study tries to give some references to the surgeons.
This meta-analysis aimed to evaluate the effectiveness of DUSO and MUSO for UIS treatment and determine the factors that should be considered when choosing surgical treatment for UIS.
Cochrane Library, MEDLINE (Ovid), PubMed, and EMBASE databases were searched. A manual search was also conducted on the relevant research to ensure that no research was omitted.
Two sample t-test showed that the postoperative grip strength of the unaffected extremity was not significantly different between the two groups. Two sample t-test was also applied to compare postoperative grip strength outcomes between two common lengths of ulnar shortening osteotomy. The postoperative grip strength outcomes were not significantly different between the 2.5-mm and 3.0-mm groups. However, the pre- and postoperative percentages of grip strength of the contralateral wrist were significantly different between the two groups. Specifically, grip strength improved by 32% and 28% in the MUSO group and DUSO group, respectively.
Although DUSO and MUSO have similar effect for UIS treatment, MUSO is associated with a lower secondary procedure rate, slightly lower postoperative DASH score, and slightly better pain relief, and thus is suitable for UIS treatment.
Although MUSO can be used for UIS treatment, it has not been verified in many patients. A large-scale and appropriate research requires long-term outcomes to distinguish and describe the benefits of one technology over another. Besides, previous retrospective studies had inherent selection biases using different surgical techniques and equipment. Most included studies did not consider or report the etiology of UIS. Therefore, large sample size, multicenter prospective studies are needed to verify the above results. Besides, these studies should use unified surgical techniques and equipment for clearer conclusions. Surgical interventions were not randomly allocated because of ethical reasons. This meta-analysis summarized the bias risk of the included studies, pooled the selected outcomes, and compared the different outcomes between MUSO and DUSO for UIS treatment.
| 1. | Tomaino MM. Ulnar impaction syndrome in the ulnar negative and neutral wrist. Diagnosis and pathoanatomy. J Hand Surg Br. 1998;23:754-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 78] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Tatebe M, Nakamura R, Horii E, Nakao E. Results of ulnar shortening osteotomy for ulnocarpal impaction syndrome in wrists with neutral or negative ulnar variance. J Hand Surg Br. 2005;30:129-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Isa AD, Mcgregor ME, Padmore CE, Langohr DG, Johnson JA, King GJW, Suh N. An In Vitro Study to Determine the Effect of Ulnar Shortening on Distal Forearm Loading During Wrist and Forearm Motion: Implications in the Treatment of Ulnocarpal Impaction. J Hand Surg Am. 2019;44:669-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Bernstein MA, Nagle DJ, Martinez A, Stogin JM Jr, Wiedrich TA. A comparison of combined arthroscopic triangular fibrocartilage complex debridement and arthroscopic wafer distal ulna resection versus arthroscopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ulnocarpal abutment syndrome. Arthroscopy. 2004;20:392-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 91] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Khouri JS, Hammert WC. Distal metaphyseal ulnar shortening osteotomy: technique, pearls, and outcomes. J Wrist Surg. 2014;3:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Yin HW, Qiu YQ, Shen YD, Xu JG, Gu YD, Xu WD. Arthroscopic distal metaphyseal ulnar shortening osteotomy for ulnar impaction syndrome: a different technique. J Hand Surg Am. 2013;38:2257-2262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Papatheodorou LK, Sotereanos DG. Step-Cut Ulnar Shortening Osteotomy for Ulnar Impaction Syndrome. JBJS Essent Surg Tech. 2017;7:e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Honigmann P, Steiger R. Intra-Articular Distal Ulnar Sliding Osteotomy for Ulnar Shortening. JBJS Essent Surg Tech. 2019;9:e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Oh WT, Kang HJ, Chun YM, Koh IH, An HM, Choi YR. Arthroscopic Wafer Procedure Versus Ulnar Shortening Osteotomy as a Surgical Treatment for Idiopathic Ulnar Impaction Syndrome. Arthroscopy. 2018;34:421-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Sennwald G, Della Santa D, Beaulieu JY. A comparison of diaphyseal and metaphyseal techniques of ulna shortening. J Hand Surg Eur Vol. 2013;38:542-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Smet LD, Vandenberghe L, Degreef I. Ulnar Impaction Syndrome: Ulnar Shortening vs. Arthroscopic Wafer Procedure. J Wrist Surg. 2014;3:98-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Marquez-Lara A, Nuñez FA Jr, Kiymaz T, Nuñez FA Sr, Li Z. Metaphyseal Versus Diaphyseal Ulnar Shortening Osteotomy for Treatment of Ulnar Impaction Syndrome: A Comparative Study. J Hand Surg Am. 2017;42:477.e1-477.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Tomaino MM. Editorial Commentary: Wrist Ulnar Impaction Syndrome: When I Use the Wafer Procedure and When I Do Not. Arthroscopy. 2018;34:431-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Nishizuka T, Tatebe M, Hirata H, Shinohara T, Yamamoto M, Iwatsuki K. Simple debridement has little useful value on the clinical course of recalcitrant ulnar wrist pain. Bone Joint J. 2013;95-B:1687-1696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Minami A, Ishikawa J, Suenaga N, Kasashima T. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg Am. 1996;21:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 86] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Möldner M, Unglaub F, Hahn P, Müller LP, Bruckner T, Spies CK. Functionality after arthroscopic debridement of central triangular fibrocartilage tears with central perforations. J Hand Surg Am. 2015;40:252-258.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Saito T, Malay S, Chung KC. A Systematic Review of Outcomes after Arthroscopic Débridement for Triangular Fibrocartilage Complex Tear. Plast Reconstr Surg. 2017;140:697e-708e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Baek GH, Chung MS, Lee YH, Gong HS, Lee S, Kim HH. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. Surgical technique. J Bone Joint Surg Am. 2006;88 Suppl 1 Pt 2:212-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Papatheodorou LK, Baratz ME, Bougioukli S, Ruby T, Weiser RW, Sotereanos DG. Long-Term Outcome of Step-Cut Ulnar Shortening Osteotomy for Ulnar Impaction Syndrome. J Bone Joint Surg Am. 2016;98:1814-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Cha SM, Shin HD, Ahn BK. Refracture after plate removal following ulnar shortening osteotomy for ulnar impaction syndrome - a retrospective case-control study. J Plast Surg Hand Surg. 2021;55:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Kang JW, Cha SM, Kim SG, Choi IC, Suh DH, Park JW. Tips and tricks to achieve osteotomy healing and prevent refracture after ulnar shortening osteotomy. J Orthop Surg Res. 2021;16:110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Chen F, Osterman AL, Mahony K. Smoking and bony union after ulna-shortening osteotomy. Am J Orthop (Belle Mead NJ). 2001;30:486-489. [PubMed] |
| 23. | Xu B, Chen L, Lee JH. Smoking and alcohol drinking and risk of non-union or delayed union after fractures: A protocol for systematic review and dose-response meta-analysis. Medicine (Baltimore). 2020;99:e18744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Cha SM, Shin HD, Lee SH. Inevitable nonunion after ulnar shortening osteotomy in patients with ulnar impaction syndrome and breast cancer under bisphosphonate treatment. Arch Orthop Trauma Surg. 2020;140:1567-1574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Owens J, Compton J, Day M, Glass N, Lawler E. Nonunion Rates Among Ulnar-Shortening Osteotomy for Ulnar Impaction Syndrome: A Systematic Review. J Hand Surg Am. 2019;44:612.e1-612.e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 26. | Rajgopal R, Roth J, King G, Faber K, Grewal R. Outcomes and complications of ulnar shortening osteotomy: an institutional review. Hand (N Y). 2015;10:535-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Das De S, Johnsen PH, Wolfe SW. Soft tissue complications of dorsal versus volar plating for ulnar shortening osteotomy. J Hand Surg Am. 2015;40:928-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Baek GH, Lee HJ, Gong HS, Rhee SH, Kim J, Kim KW, Kong BY, Oh WS. Long-term outcomes of ulnar shortening osteotomy for idiopathic ulnar impaction syndrome: at least 5-years follow-up. Clin Orthop Surg. 2011;3:295-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | de Runz A, Pauchard N, Sorin T, Dap F, Dautel G. Ulna-Shortening Osteotomy: Outcome and Repercussion of the Distal Radioulnar Joint Osteoarthritis. Plast Reconstr Surg. 2016;137:175-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Cha SM, Choi BS, Shin HD. Radiological degenerative changes in the distal radioulnar joint after ulnar shortening osteotomy in patients with idiopathic ulnar impaction syndrome: Analysis of factors affecting degenerative lesions. J Orthop Sci. 2017;22:1042-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Aronson J, Shen X. Experimental healing of distraction osteogenesis comparing metaphyseal with diaphyseal sites. Clin Orthop Relat Res. 1994;25-30. [PubMed] |
| 32. | Claes L, Reusch M, Göckelmann M, Ohnmacht M, Wehner T, Amling M, Beil FT, Ignatius A. Metaphyseal fracture healing follows similar biomechanical rules as diaphyseal healing. J Orthop Res. 2011;29:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 33. | Nuñez FA Jr, Marquez-Lara A, Newman EA, Li Z, Nuñez FA Sr. Determinants of Pain and Predictors of Pain Relief after Ulnar Shortening Osteotomy for Ulnar Impaction Syndrome. J Wrist Surg. 2019;8:395-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Cha SM, Shin HD, Ahn KJ. Prognostic Factors Affecting Union After Ulnar Shortening Osteotomy in Ulnar Impaction Syndrome: A Retrospective Case-Control Study. J Bone Joint Surg Am. 2017;99:638-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9207] [Cited by in RCA: 8360] [Article Influence: 522.5] [Reference Citation Analysis (2)] |
| 36. | Quadlbauer S, Pezzei C, Jurkowitsch J, Rosenauer R, Pichler A, Schättin S, Hausner T, Leixnering M. Functional and radiological outcome of distal radius fractures stabilized by volar-locking plate with a minimum follow-up of 1 year. Arch Orthop Trauma Surg. 2020;140:843-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 37. | Terzis A, Neubrech F, Sebald J, Sauerbier M. [Surgical treatment of ulnar impaction syndrome : Ulnar shortening osteotomy through the ulnopalmar approach using a low-profile, locking plate]. Oper Orthop Traumatol. 2019;31:547-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Schmidle G, Arora R, Gabl M. Ulnar shortening with the ulna osteotomy locking plate. Oper Orthop Traumatol. 2012;24:284-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Terzis A, Koehler S, Sebald J, Sauerbier M. Ulnar shortening osteotomy as a treatment of symptomatic ulnar impaction syndrome after malunited distal radius fractures. Arch Orthop Trauma Surg. 2020;140:681-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 40. | Iniesta A, Bonev B, Curvale C, Legré R, Gay A. Outcomes of ulnar shortening osteotomy using a new compression plate. Hand Surg Rehabil. 2020;39:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 41. | Constantine KJ, Tomaino MM, Herndon JH, Sotereanos DG. Comparison of ulnar shortening osteotomy and the wafer resection procedure as treatment for ulnar impaction syndrome. J Hand Surg Am. 2000;25:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 77] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hung S, Taiwan; Scholtysek C, Germany S-Editor: Wang JL L-Editor: A P-Editor: Yu HG