Published online Apr 16, 2023. doi: 10.12998/wjcc.v11.i11.2541
Peer-review started: December 26, 2022
First decision: January 12, 2023
Revised: January 27, 2023
Accepted: March 17, 2023
Article in press: March 17, 2023
Published online: April 16, 2023
Processing time: 100 Days and 21.8 Hours
Juxtaglomerular cell tumor (JGCT) of the kidney, also known as reninoma, is a rare renal tumor that typically clinically manifests as hypertension, hypokalemia, high renin, and high aldosterone. It is a cause of secondary hypertension. Pregnancy with JGCT is rarer and easily misdiagnosed as pregnancy-induced hypertension, thus affecting treatment.
A 28-year-old woman presented in early pregnancy with hypertension (blood pressure of 229/159 mmHg), nausea, and occasional dizziness and headache. The patient was diagnosed with pregnancy-induced hypertension, and no relief was found after symptomatic treatment; hence, the pregnancy was terminated by artificial abortion. Her blood pressure remained high following termination of pregnancy. Blood tests suggested hypokalemia (2.997 mmol/L), blood aldo
Patients with pregnancy complicated by JGCT are difficult to diagnose. Herein, we advise surgeons on proper handling of such situations.
Core Tip: Juxtaglomerular cell tumor (JGCT) is a rare endocrine tumor of the kidney. Typical JGCTs are characterized by high serum renin, high aldosterone secretion, severe hypertension, and severe hypokalemia, known as the “three high and one low” phenomenon. The mainstream treatment is surgery. We report an even rarer case of pregnancy complicated with JGCT, who was misdiagnosed with pregnancy-induced hypertension in a primary hospital, and the pregnancy was terminated artificially due to poor response to conservative treatment. The patient was admitted to our hospital for further treatment because her blood pressure remained high after termination of pregnancy and she was diagnosed with JGCT. The patient recovered well after surgery to remove the tumor. In this article, the case is analyzed retrospectively in the context of the literature in an attempt to explore the diagnosis, treatment, and prognosis of this rare disease.
- Citation: Fu X, Deng G, Wang K, Shao C, Xie LP. Pregnancy complicated by juxtaglomerular cell tumor of the kidney: A case report. World J Clin Cases 2023; 11(11): 2541-2548
- URL: https://www.wjgnet.com/2307-8960/full/v11/i11/2541.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i11.2541
Juxtaglomerular cell tumor (JGCT) is a very rare renin-secreting tumor of the kidney. The tumor is typically found in young adults, with a peak incidence in the second and third decades of life. It was first reported by Robertson et al[1] in 1967, who first described it as a special type of juxtamedullary angiomyocytoma. Subsequently, Kihara reported a second case, calling it the Robertson Kihara syndrome[1,2]. At present, approximately only 100 JGCT cases have been reported worldwide, among which pregnancy complicated by JGCT is even rarer[3]. JGCT can independently secrete large amounts of renin, resulting in excessive secretion of angiotensin and aldosterone, and causing patients to have severe hypertension and hypokalemia that produce a series of symptoms, including headache, dizziness, blurred vision, hypertension-induced nausea and vomiting, muscle weakness, edema, and arrhythmia caused by hypokalemia. Severe target organ damage and cardiovascular disease occur in a short period of time. The severity of these symptoms is independent of tumor size[4,5]. Expression of renin and intracytoplasmatic rhomboid crystals or granules on electron microscopic images are diagnostic features of JGCT. The immunohistochemical profile of JGCT has been recently reported as being immunoreactive for vimentin, focally immunoreactive for smooth muscle actin, and negative for cytokeratin. CD34 and CD117 immunoreactivities have been reported as helpful markers of JGCT[2,6].
JGCT may be associated with hypertension, which may lead to a misdiagnosis as pregnancy-induced hypertension in patients with JGCT during pregnancy, thus affecting treatment[7]. In this article, the clinical data and imaging findings of a patient with pregnancy complicated by JGCT are analyzed retrospectively in the context of the literature in an attempt to explore the diagnosis, treatment, and prognosis of this rare disease.
A 28-year-old pregnant woman was first admitted to Department of Obstetrics of a primary hospital with vaginal bleeding and high blood pressure for 2 d at 7 wk of gestation.
One month previously, the patient presented with vaginal bleeding and high blood pressure of 229/159 mmHg at 7 wk of gestation, with nausea, occasionally accompanied by dizziness and a headache. The primary diagnosis was threatened abortion from pregnancy-induced hypertension. Antihypertensive therapy performed after admission was not beneficial; thus, the pregnancy was terminated by artificial abortion. However, blood pressure remained high (151/110 mmHg). For further treatment, the patient was admitted to the Department of Cardiology of our hospital. During hospitalization in the Cardiology Department, adrenal-enhanced computed tomography (CT) examination was performed to identify the cause of hypertension. CT examination revealed no adrenal abnormalities, but a tumor of the right kidney was detected, and the patient was referred to our Urology Department for further treatment.
The patient had no history of hypertension, diabetes, cardiovascular or cerebrovascular diseases, and also no history of surgery. The patient had no history of viral or bacterial infection of the urinary system.
The patient was marriageable, had normal menstruation in the past, and had no history of pregnancy or abortion, and no smoking and drinking habits. Her family history was ordinary, and there was no history of genetic heritability of cancer. The patient had no history of viral or bacterial infection of the urinary system.
No tenderness in the bilateral kidneys, ureters, or bladder was observed on examination. Furthermore, no obvious abnormality was found upon gynecological physical examination, and there was no vaginal bleeding when the patient was transferred to our department.
Laboratory studies showed a blood aldosterone level of 121 ng/L (decubitus reference value, 30-236) and 613 ng/L (orthostatic reference value, 30-353), and the blood renin level was 352.2 mIU/L (decubitus reference value, 2.8-39.9) and 487.9 mIU/L (orthostatic reference value, 4.4-46.1). Meanwhile, serum potassium level was 2.97 mmol/L (reference value, 3.5-5.5). Levels of other hormones, such as adrenaline, dopamine, norepinephrine, and cortisol, were normal. Urine cell analysis and urine culture for bacteria were negative. There were no obvious abnormalities in routine blood tests, coagulation function, hepatitis B, acquired immunodeficiency syndrome, syphilis, liver and kidney function, or other blood biochemical tests.
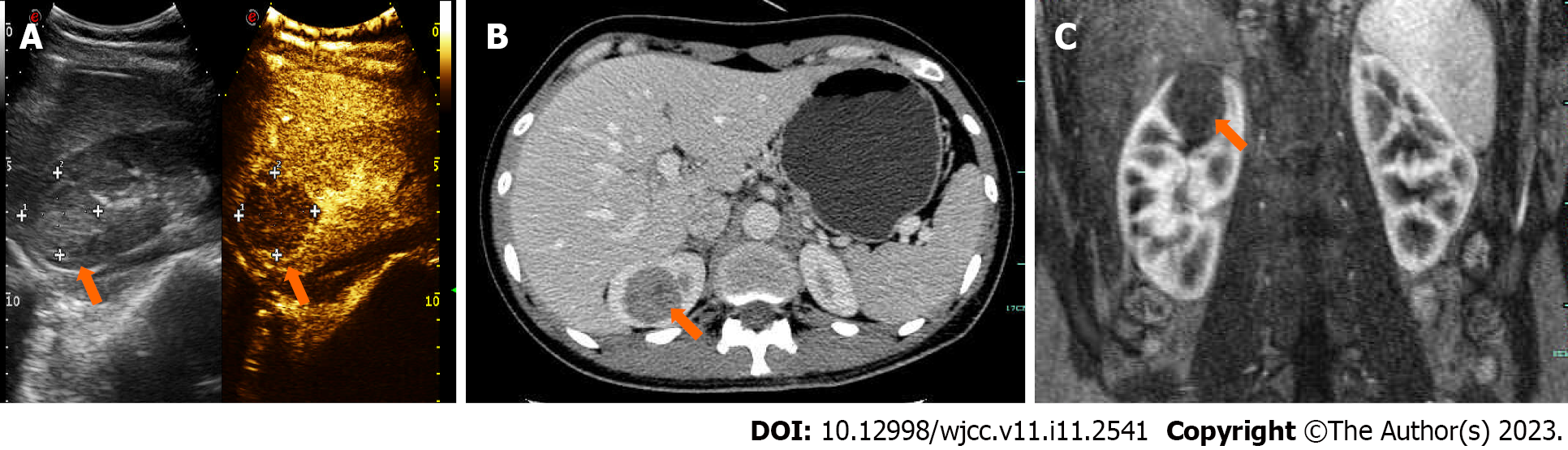
Contrast-enhanced ultrasound of the kidney showed a moderately echogenic mass with low enhancement that was characterized by a “slow in and fast out” pattern (Figure 1A). Both computed tomography urography (CTU) and magnetic resonance imaging (MRI) showed a right upper pole renal mass measuring approximately 3.5 cm × 3 cm × 2.5 cm (endogenic type) in size, without significant abnormalities in the bilateral adrenal glands (Figure 1B and C).
The final diagnosis of the presented case was JGCT of the kidney.
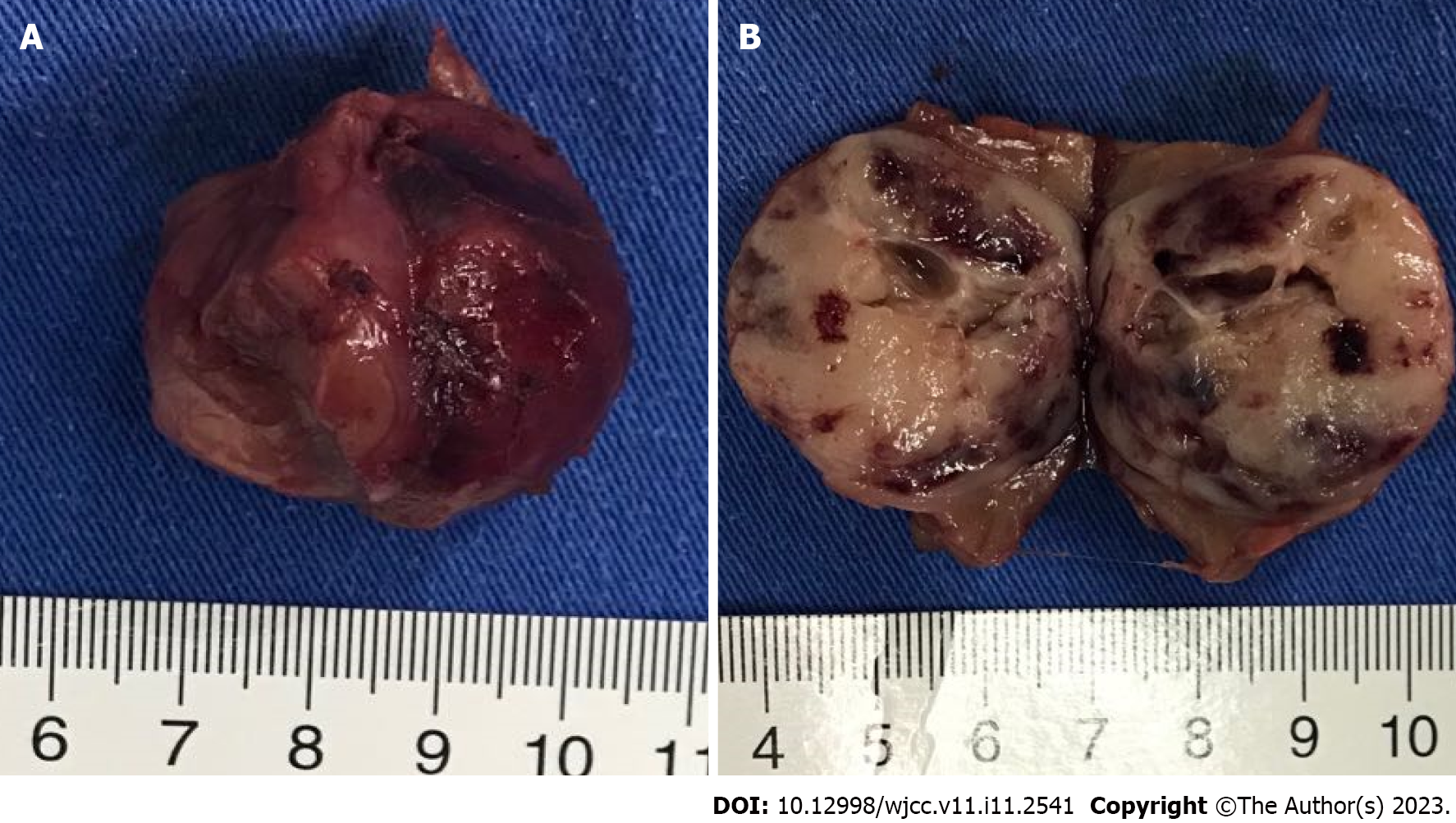
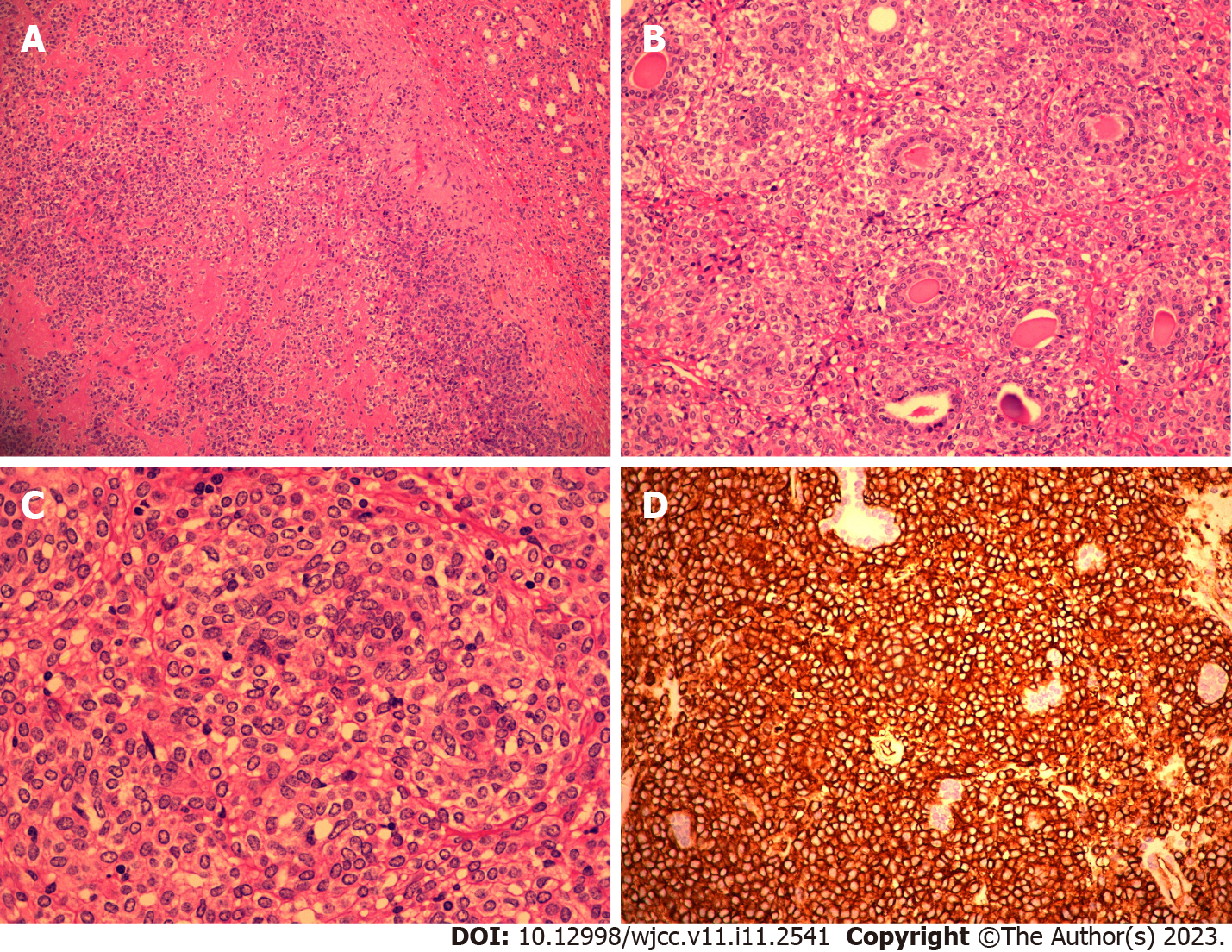
Considering possible malignancy, tumor size and location, experience of the chief surgeon, and will of the patient’s family members, retroperitoneoscopic partial nephrectomy of the right kidney was performed. During surgery, laparoscopic ultrasound was used to accurately locate the tumor, which was successfully resected (Figure 2). Both frozen pathological examination and postoperative pathological analyses of the surgical specimen reported JGCT, and immunohistochemistry highlighted the following: CD34 (+), vimentin (+), CK117 (-), and Ki-67 (< 5% positivity) (Figure 3).
The patient was discharged on the seventh day after surgery. One month post-surgery, the patient’s blood pressure decreased to normal without dizziness, headache, nausea, vomiting, or other discomfort. Blood potassium, aldosterone, and renin levels normalized after re-examination. Four months post-surgery, contrasted-enhanced CT revealed no tumor recurrence.
After long-term follow-up, the patient became pregnant again 6 mo after surgery; no hypertension occurred during the pregnancy. Eventually, the patient delivered a healthy female neonate.
JGCT, also known as reninoma, is a rare endocrine tumor of the kidney, which causes secondary hypertension. Current studies suggest that JGCT may be associated with an increased number of chromosome 10 and deletion of chromosome 9, X, and the long arm of chromosome 11[8]. Wong et al[9] statistically analyzed 89 JGCT cases, and the results showed that these tumors were more common in the 20-30 year age group, with an average age of 27 years, and most occurred in females, with a male-to-female ratio of approximately 1:2[9]. Dong et al[10] proposed to divide JGCTs into three categories according to the blood pressure and blood potassium status of the patient: The first category is typical JGCTs, where patients have symptoms of hypertension and hypokalemia; the second type is atypical JGCTs, where patients have one of the two symptoms; the third type is nonfunctional JGCTs, which is confirmed by postoperative pathology despite the absence of both symptoms. Typical renin tumors are the most common type, characterized by high serum renin, high aldosterone secretion, severe hypertension, and severe hypokalemia; this is known as the “three high and one low” phenomenon. Excess renin secreted by JGCT activates the renin-angiotensin-aldosterone system (RAAS), resulting in an abnormal increase of angiotensin II and aldosterone, constriction of peripheral blood vessels, and promotion of water and sodium retention, which often leads to uncontrolled hypertension, accompanied by dizziness, headache, nausea and vomiting, blurred vision, and even fundal hemorrhage, proteinuria, and other manifestations of hypertensive target organ dysfunction. JGCT-induced hypertension often requires the combined use of multiple antihypertensive drugs, mainly angiotensin converting enzyme inhibitors, to effectively control blood pressure[11]. In addition, a secondary increase in aldosterone boosts urinary potassium excretion by promoting exchange of sodium and potassium in the collecting duct of the main cells, leading to hypokalemia, which may lead to limb weakness and other corresponding symptoms[12]. A 24-h urine potassium test is helpful in detecting secondary aldosteronism during the course of the disease.
Consistent with previous observations reported in the literature, our patient was a 28-year-old woman who presented with recurrent hypertension and hypokalemia before surgery-a typical case of JGCT. In our case, preoperative antihypertensive therapy was ineffective, and there was accompanying dizziness, headache, and nausea, with hypokalemia, which was consistent with descriptions in the literature. It should be noted that although the patient’s 24-h urine potassium level was within the normal range, abnormal potassium excretion was still present because the patient had been in a low potassium state, under which urinary potassium excretion was reduced, suggesting a secondary increase in aldosterone.
The diagnosis of JGCT should be combined with clinical manifestations, laboratory examination, and imaging examination, such as ultrasonography, CT, and MRI. Serum electrolyte, renin, and aldosterone levels should be tested in cases of suspected JGCT. Patients with typical JGCT present with hypokalemia, high renin, and high aldosterone, with a normal aldosterone-renin ratio (ARR), which can be distinguished from primary aldosteronism (high aldosterone levels, normal or elevated renin levels, and increased ARR) because renin secretion is inhibited by abnormally high aldosterone levels[13]. RAAS inhibitors should be avoided as far as possible before detection, because they may affect the secretion of renin, aldosterone, and other hormones, thus covering up the disease. Comparison of renin activity in bilateral renal venous blood by selective or segmental renal venous blood sampling may be helpful in diagnosing JGCT; however, it is not recommended clinically due to its high false-negative rate. Previous studies have shown that the positive rate of this test was about 62.5%; meanwhile, in a study of 14 cases of JGCTs in China, it was only 21.4%[14]. Our case did not use RAAS inhibitors before the test, and blood test showed hypokalemia, hyperreninemia, and elevated aldosterone; ARR was normal, which was consistent with literature reports. Considering the low positive rate of bilateral renin activity compared to renal venous blood sampling, this test was not performed.
In ultrasonography images, JGCTs mostly present as round masses with low or slightly high echogenicity; however, due to their rarity and typically small volume, they are easily undiagnosed and misdiagnosed on ultrasonography[15]. On a plain CT scan, low to iso-dense circular masses with capsules were mostly found, most of which were located inside the renal parenchyma. Enhanced CT showed no significant enhancement of tumor in the early stage; however, mild to moderate enhancement in delayed stage or portal vein stage was seen. MRI images are characterized by low to equal signal intensity in T1W1 and high signal intensity in T2W2. At present, many experts believe that MRI may lead to misdiagnosis. Compared to MRI, CT scan is more sensitive for JGCT and has more diagnostic value[16]. However, small JGCTs are sometimes left undiagnosed by CT. Faucon et al[17] compared CT and MRI images of ten patients with JGCTs and suggested that MRI examination should be performed for patients with suspected JGCTs if no abnormality was found on CT[17].
A definitive diagnosis of JGCTs requires pathological examination. Microscopically, the tumor tissue shows closely arranged round or polygonal cells, which are rich in small blood vessels. The tumor cells are mostly of the same size and might have focal low-to-moderate atypia. Immunohistochemistry shows that tumor cells are positive for CD34 and vimentin, and CD117 is positive in some cases[18]. Immunohistochemical results of this case were positive for CD34 and vimentin, and negative for CD117, which was consistent with literature reports. Pregnancy complicated by reninoma is rarely reported, and patients are often misdiagnosed as eclamptic or preeclamptic. Mismanagement often leads to premature delivery, abortion, or stillbirth[19]. In the case reported by Ohashi et al[20], undiagnosed JGCT caused uncontrolled hypertension. The patient had been diagnosed with pre-eclampsia before termination of pregnancy, and pregnancy was terminated at 25 wk due to congestive heart failure and acute kidney injury. Further examination after termination of pregnancy revealed a tumor in the left kidney, which was confirmed as JGCT on pathological examination after surgical resection[20].
Regarding the relationship between pregnancy and renin tumor development, studies have reported that the change of immune status that occurs during pregnancy makes pregnant women vulnerable to pathogenic infections, including those caused by carcinogenic viruses[21,22]. For example, oncogenic polyomavirus BK can promote the proliferation, invasion, and migration of bladder cancer in immunocompromised patients[23,24]. Regarding Merkel cell polyomavirus, whose DNA sequences have been detected in blood samples from immunocompetent and immunosuppressed patients with kidney disease, pregnant females have been reported to present a decrease in antibody response to this virus[21,25]. Therefore, whether pregnancy complicated by reninoma is associated with viral or bacterial infections is also an aspect to be considered. However, in this case, the pregnant woman had no history of viral or bacterial infection of the urinary system, so we do not believe that the patient’s JGCT was related to viral or bacterial infection.
RAAS inhibitors are helpful in relieving hypertension and hypokalemia caused by JGCT, and it has been reported that aliskiren can effectively improve hypertension and hypokalemia in patients before surgery[16]. When the diagnosis of JGCT is confirmed, surgery is the preferred treatment. Previous studies have shown that the average size of JGCTs is approximately 3 cm, and partial nephrectomy can be considered for most small JGCTs to protect renal function as much as possible[16]. Currently, with the advances in laparoscopic technology, laparoscopic partial peritoneal nephrectomy or retroperitoneal partial nephrectomy has been gradually promoted, and studies have shown that the latter has the advantages of lower risk, shorter operation time, faster postoperative recovery, and relatively easy learning compared to the former, thus fast becoming the conventional surgical choice[14], and Da Vinci robot-assisted laparoscopic partial nephrectomy is certain to be more advantageous[26]. According to literature reviews, most JGCTs are endogenous, which may be related to their origin from paraveral cells. In our case, the retroperitoneal approach was adopted. Since the tumor was endogenous, intraoperative ultrasound was used to locate the tumor, which greatly accelerated the surgical progress. JGCTs are mostly benign tumors with a good prognosis, and blood pressure and potassium of patients can return to normalcy after resection; however, a few malignant cases have been reported. In a case reported by Professor Shera et al[27] from India, an 8-year-old boy was admitted to the hospital in emergency due to intractable hypertension (blood pressure 210/140 mmHg). Examination revealed an 8 cm × 8 cm mass in the left hilum of the kidney, and pathology after total nephrectomy suggested JGCT. Close follow-up and review after surgery revealed that the patient developed hypertension again a year later, and CT examination revealed a mass about 5 cm × 4 cm in the left renal fossa. Blood pressure returned to normal after another surgical excision. The overall features of the recurrent tumor were suggestive of a malignant and invasive form of JGCT[27]. Therefore, patients with JGCTs should be followed for as long as possible to monitor for tumor recurrence.
In the present case, the pregnant woman was initially misdiagnosed with pregnancy-induced hypertension in a primary hospital. As the pregnancy was at an early stage, she opted for induced abortion. Reasons for misdiagnosis were as follows: The patient could not undergo CT because of the pregnancy and doctors in other hospitals did not routinely perform Doppler ultrasound examination of the urinary system. However, the patient’s hypertension did not resolve after abortion, which necessitated further CT examination that found the renal tumor. This case reminds us that if refractory hypertension is present during pregnancy, JGCT should be considered, and ultrasonography of the kidney and adrenal gland, MRI scan, or other endocrine hormone examinations need to be completed for further diagnosis. In addition, although most cases of JGCT present as benign tumors of the kidney and are treated with partial nephrectomy or nephrectomy, there are isolated cases of malignant infiltration, and JGCT may also co-exist with other forms of cancer, such as leukemia and breast cancer. JGCT may play a mediating role in these other forms of cancer, for example by regulating renin overexpression[28]. Therefore, we should further encourage the study of JGCT related pathological systems.
The authors thank the patient for allowing us to publish this case report.
| 1. | Robertson PW, Klidjian A, Harding LK, Walters G, Lee MR, Robb-Smith AH. Hypertension due to a renin-secreting renal tumour. Am J Med. 1967;43:963-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 247] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Kim HJ, Kim CH, Choi YJ, Ayala AG, Amirikachi M, Ro JY. Juxtaglomerular cell tumor of kidney with CD34 and CD117 immunoreactivity: report of 5 cases. Arch Pathol Lab Med. 2006;130:707-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Lin SY, Liu WY, Chen WC, Chen RH. Secondary hypertension due to a renin-secreting juxtaglomerular cell tumor. J Formos Med Assoc. 2010;109:237-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Conn JW, Cohen EL, Lucas CP, McDonald WJ, Mayor GH, Blough WM Jr, Eveland WC, Bookstein JJ, Lapides J. Primary reninism. Hypertension, hyperreninemia, and secondary aldosteronism due to renin-producing juxtaglomerular cell tumors. Arch Intern Med. 1972;130:682-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Skarakis NS, Papadimitriou I, Papanastasiou L, Pappa S, Dimitriadi A, Glykas I, Ntoumas K, Lampropoulou P, Kounadi T. Juxtaglomerular cell tumour of the kidney: a rare cause of resistant hypertension. Endocrinol Diabetes Metab Case Rep. 2022;2022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Gupta S, Folpe AL, Torres-Mora J, Reuter VE, Zuckerman JE, Falk N, Stanton ML, Muthusamy S, Smith SC, Sharma V, Sethi S, Herrera-Hernandez L, Jimenez RE, Cheville JC. Immunohistochemical expression of renin and GATA3 help distinguish juxtaglomerular cell tumors from renal glomus tumors. Hum Pathol. 2022;128:110-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 7. | Xue M, Chen Y, Zhang J, Guan Y, Yang L, Wu B. Reninoma coexisting with adrenal adenoma during pregnancy: A case report. Oncol Lett. 2017;13:3186-3190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Brandal P, Busund LT, Heim S. Chromosome abnormalities in juxtaglomerular cell tumors. Cancer. 2005;104:504-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Wong L, Hsu TH, Perlroth MG, Hofmann LV, Haynes CM, Katznelson L. Reninoma: case report and literature review. J Hypertens. 2008;26:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 81] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Dong D, Li H, Yan W, Xu W. Juxtaglomerular cell tumor of the kidney--a new classification scheme. Urol Oncol. 2010;28:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Yu ZQ, Wang JW, Ma LL. [Summary and analysis of diagnostic data of 110 cases of juxtaglomerular cell tumers and introduction of typical cases]. Zhonghua Gaoxueya Zazhi. 2018;26:693-697. [DOI] [Full Text] |
| 12. | Kang S, Chen F, Zhong Y, Han B, Cheng G, Guo A, Tian Y, Tong X, Dou J, Ye H. Preoperative Diagnosis of Juxtaglomerular Cell Tumors in Eight Patients. J Clin Hypertens (Greenwich). 2016;18:982-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Piaditis G, Markou A, Papanastasiou L, Androulakis II, Kaltsas G. Progress in aldosteronism: a review of the prevalence of primary aldosteronism in pre-hypertension and hypertension. Eur J Endocrinol. 2015;172:R191-R203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 14. | Liu K, Wang B, Ma X, Li H, Zhang Y, Li J, Yao Y, Tang L, Xuan Y, Guo A, Zhang X. Minimally Invasive Surgery-Based Multidisciplinary Clinical Management of Reninoma: A Single-Center Study. Med Sci Monit. 2019;25:1600-1610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Osawa S, Hosokawa Y, Soda T, Yasuda T, Kaneto H, Kitamura T, Kozawa J, Otsuki M, Imagawa A, Okumi M, Miyagawa Y, Nonomura N, Shimomura I. Juxtaglomerular cell tumor that was preoperatively diagnosed using selective renal venous sampling. Intern Med. 2013;52:1937-1942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Rosei CA, Giacomelli L, Salvetti M, Paini A, Corbellini C, Tiberio G, Muiesan ML. Advantages of renin inhibition in a patient with reninoma. Int J Cardiol. 2015;187:240-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Faucon AL, Bourillon C, Grataloup C, Baron S, Bernadet-Monrozies P, Vidal-Petiot E, Azizi M, Amar L. Usefulness of Magnetic Resonance Imaging in the Diagnosis of Juxtaglomerular Cell Tumors: A Report of 10 Cases and Review of the Literature. Am J Kidney Dis. 2019;73:566-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Vidal-Petiot E, Bens M, Choudat L, Fernandez P, Rouzet F, Hermieu JF, Bruneval P, Goujon JM, Flamant M, Vandewalle A. A case report of reninoma: radiological and pathological features of the tumour and characterization of tumour-derived juxtaglomerular cells in culture. J Hypertens. 2015;33:1709-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Lachvac L, Svajdler M, Valansky L, Nagy V, Benicky M, Frohlichova L, Nyitrayova O. Juxtaglomerular cell tumor, causing fetal demise. Int Urol Nephrol. 2011;43:365-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Ohashi Y, Kobayashi S, Arai T, Nemoto T, Aoki C, Nagata M, Sakai K. Focal Segmental Glomerulosclerosis Secondary to Juxtaglomerular Cell Tumor during Pregnancy: A Case Report. Case Rep Nephrol Urol. 2014;4:88-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Mazziotta C, Pellielo G, Tognon M, Martini F, Rotondo JC. Significantly Low Levels of IgG Antibodies Against Oncogenic Merkel Cell Polyomavirus in Sera From Females Affected by Spontaneous Abortion. Front Microbiol. 2021;12:789991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 22. | Cheungpasitporn W, Thongprayoon C, Craici IM, Sharma K, Chesdachai S, Khoury NJ, Ettore AS. Reactivation of BK polyomavirus during pregnancy, vertical transmission, and clinical significance: A meta-analysis. J Clin Virol. 2018;102:56-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Zeng Y, Sun J, Bao J, Zhu T. BK polyomavirus infection promotes growth and aggressiveness in bladder cancer. Virol J. 2020;17:139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Shen CL, Wu BS, Lien TJ, Yang AH, Yang CY. BK Polyomavirus Nephropathy in Kidney Transplantation: Balancing Rejection and Infection. Viruses. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 25. | Jin HT, Park SJ, Choi EK, Kim YS. The frequency of Merkel cell polyomavirus in whole blood from immunocompetent and immunosuppressed patients with kidney disease and healthy donors. Microb Pathog. 2019;131:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Kweon OJ, Lim YK, Kim HR, Lee MK, Lee TJ, Won H, Choi SY, Kim JW, Chi BH, Chang IH, Moon YT, Kim KD, Kim TH. Robot-Assisted Partial Nephrectomy for Treatment of Juxtaglomerular Cell Tumor of the Kidney: A Case Report. J Endourol Case Rep. 2020;6:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Shera AH, Baba AA, Bakshi IH, Lone IA. Recurrent malignant juxtaglomerular cell tumor: A rare cause of malignant hypertension in a child. J Indian Assoc Pediatr Surg. 2011;16:152-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 28. | Inam R, Gandhi J, Joshi G, Smith NL, Khan SA. Juxtaglomerular Cell Tumor: Reviewing a Cryptic Cause of Surgically Correctable Hypertension. Curr Urol. 2019;13:7-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Ait Addi R, Morocco; Gica N, Romania; Rotondo JC, Italy S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR