Published online Mar 6, 2022. doi: 10.12998/wjcc.v10.i7.2357
Peer-review started: October 17, 2021
First decision: December 17, 2021
Revised: December 18, 2021
Accepted: January 19, 2022
Article in press: January 19, 2022
Published online: March 6, 2022
Processing time: 135 Days and 17.4 Hours
Anterior cutaneous nerve entrapment syndrome is defined as abdominal pain due to entrapped intercostal nerves. This is the first report of a patient successfully treated for anterior cutaneous nerve entrapment syndrome after laparoscopic surgery with an ultrasound-guided rectus sheath block. The rectus sheath block physically lysed adhesions and relieved pain from anterior cutaneous nerve entrapment syndrome.
The patient is a 44-year-old man who presented with severe left upper abdominal pain at an operative scar one month after laparoscopic ulcer repair. Diagnosis and treatment were performed using an ultrasound-guided rectus sheath block with 0.1% lidocaine 20 mL. The pain was relieved after the block. The diagnosis was anterior cutaneous nerve entrapment syndrome. Rectus sheath block may be effective for patients with anterior cutaneous nerve entrapment syndrome.
Ultrasound-guided rectus sheath block is a promising treatment modality for patients with postoperative anterior cutaneous nerve entrapment syndrome due to adhesions.
Core Tip: Anterior cutaneous nerve entrapment syndrome (ACNES) is defined as chronic abdominal wall pain caused by entrapment of cutaneous branches of the lower thoracoabdominal intercostal nerves. In the present report, ACNES after a laparoscopic procedure was successfully treated with ultrasound-guided rectus sheath block. Ultrasound-guided rectus sheath block may become an important part of the armamentarium.
- Citation: Sawada R, Watanabe K, Tokumine J, Lefor AK, Ando T, Yorozu T. Ultrasound-guided rectus sheath block for anterior cutaneous nerve entrapment syndrome after laparoscopic surgery: A case report. World J Clin Cases 2022; 10(7): 2357-2362
- URL: https://www.wjgnet.com/2307-8960/full/v10/i7/2357.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i7.2357
Laparoscopic surgery is generally less invasive than open surgery. Recently, laparoscopic repair of perforated peptic gastroduodenal ulcers has become more commonly performed. Advantages of the laparoscopic repair of a perforated peptic ulcer are less postoperative pain[1,2], a lower rate of surgical site infection[2], and shorter postoperative hospital stay[1].
Even though laparoscopic surgery is less invasive, chronic abdominal wall pain after laparoscopic surgery can complicate postoperative recovery and be debilitating to the patient[3]. Chronic abdominal wall pain is thought to be caused either by a viscus and/or the abdominal wall. The differential diagnosis depends on the origin of the pain. Anterior cutaneous nerve entrapment syndrome (ACNES) is defined as abdominal pain due to entrapped intercostal nerves[4]. We successfully treated a patient with ACNES, which developed after laparoscopic repair of a perforated gastroduodenal ulcer, using ultrasound-guided rectus sheath block. Written informed consent was obtained from the patient for the publication.
A 44-year-old man underwent emergency laparoscopic repair of a perforated gastroduodenal ulcer. Laparoscopic repair was performed successfully, and he was discharged without complications on postoperative day nine. One month later, he experienced severe pain in the left upper abdomen.
The pain was sharp, with a stabbing sensation two or three times per day without obvious cause and lasted for at least two hours. The pain disturbed his work and degraded his quality of life. Endoscopic examination and computed tomography scan showed no abnormal findings. Treatment with acetaminophen 800 mg daily was started, but the pain continued.
He had a past medical history of urolithiasis treated with medication.
No special notes.
The operating surgeon consulted with a pain specialist about the patient’s pain. The pain was characterized by sudden onset, continuing for a long time, and the pain intensity was reported as 5-6/10. The patient could indicate the location where the pain began, which was at the operative scar (Figure 1). Hypoesthesia was recognized using the cold test compared to the contralateral side (6/10). There was no numbness or allodynia at the location. Carnett’s test[4] was negative.
Ultrasound examination.
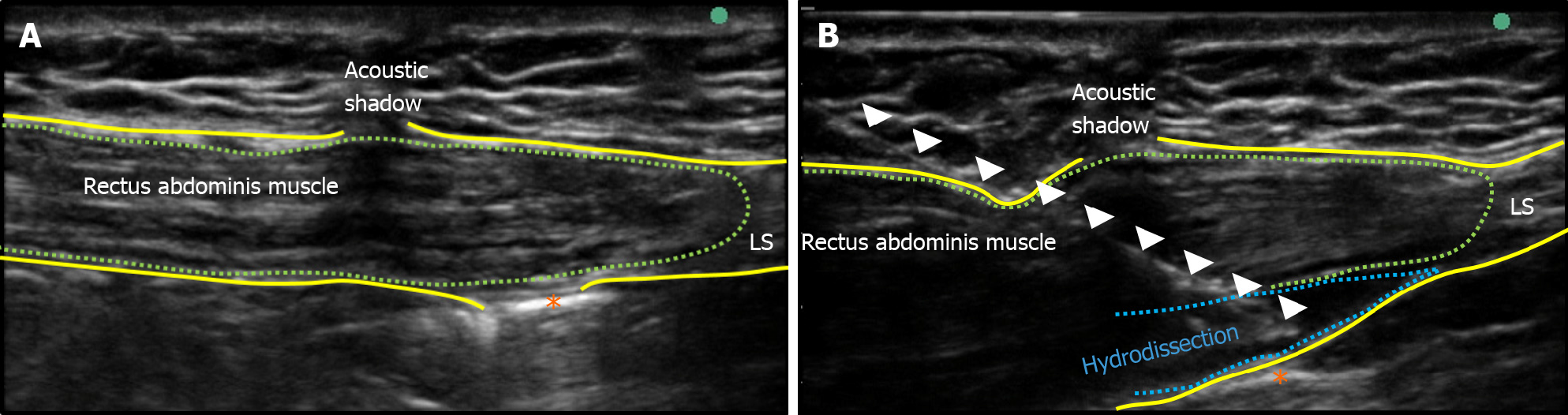
The pain specialist imaged the operative scar with ultrasound and found an adhesion-like area on the posterior sheath of the rectus abdominis muscle (Figure 2A).
No expert consultation was conducted.
ACNES was diagnosed in this patient.
A rectus sheath block was performed with 20 mL of 0.1% lidocaine. The adhesion-like area was detached from the rectus abdominis muscle by hydrodissection (Figure 2B).
After hydrodissection, the pain was immediately relieved. The frequency of pain decreased to 0-1 episodes per month, and the duration of the pain decreased to several minutes for each episode. The patient was satisfied with the treatment and did not want any more nerve blocks.
The pain specialist conducted a Carnett’s test again. Interestingly, these tests were positive this time, but the evoked pain was minimal.
ACNES is defined as chronic abdominal wall pain caused by entrapment of cutaneous branches of the lower thoracoabdominal intercostal nerves[4,5]. The pain due to ACNES is refractory to treatment, can be sharp, dull or burning in character[4-6]. Diagnosis of ACNES is based on clinical findings and excluding other diagnoses, which include bowel-related (functional abdominal pain; irritable bowel syndrome, constipation), gynecologic (ovarian cyst etc.), pain after trauma or surgery, urologic (infection, etc.), posture-related pain (orthopedic, etc.)[4,7] and psychogenic abdominal pain[8]. Therefore, routine postoperative pain should be excluded from consideration as ACNES[4]. However, surgery was reported to cause ACNES in some patients[4]. In the present patient, entrapment of an anterior cutaneous nerve by the operative scar was thought to be the most likely cause. The commonly held definition (above) of ACNES may be incomplete. The clinical entity of ACNES is a syndrome of the same type of pain. We would like to propose a new definition, in which ACNES is classified into primary and secondary types. Primary ACNES is defined as the originally characterized ACNES which is idiopathic in nature, and secondary ACNES is defined as anterior cutaneous nerve entrapment caused during the healing process after surgery or a traumatic injury.
Clinical findings of ACNES are characterized as a specific type of pain[4-8]. The pain is always in the same location, just lateral to the middle of the abdomen, and provoked by daily activities[6]. A special maneuver for diagnosis is Carnett’s test[4,7]. A positive Carnett’s test means that tenderness is present when placing a finger on the pain location during abdominal muscle tensing caused by lifting the head or legs[4,7]. In the present patient, the Carnett’s test was negative during the first physical examination, but was positive at the next physical examination. Physical findings strongly suggested that the pain was derived from the abdominal wall. Boelens et al[9], reported that a positive Carnett’s test in patients suspected to have ACNES was 88% sensitive, but inconclusive or negative tests were 9% and 3% respectively. In the present patient, Carnett’s test might not have been performed completely due to the patient’s fear of refractory pain. Some clinicians might not perform the physical test with sufficient strength at the first examination. This speculation might explain why the second test became positive.
Trigger point injection[10], transverse abdominis plane block[11] and rectus sheath block[12] and have been reported as useful examinations to establish the diagnosis and also the treatment of ACNES. In the present report, ACNES after a laparoscopic procedure was successfully treated with ultrasound-guided rectus sheath block. We speculate that if the anterior cutaneous nerve is entrapped as defined by ACNES, the main effect of rectus sheath block may be to release the entrapped nerve with hydrodissection rather than the effect of the local anesthetic. Recently, ultrasound-guided nerve hydrodissection has been established as a treatment for nerve entrapment[13]. In experiments using animal models of neuropathic pain, nerve hydrodissection reduces nerve irritability and improves blood flow to the nerve by relieving pressure on the free nerve endings surrounding the epineurium and the feeding vessels[13]. The application of ultrasound-guided techniques to the treatment of ACNES is still in development, and further studies will be needed to determine their efficacy.
The number of laparoscopic procedures is steadily increasing, and chronic pain after laparoscopic surgery is also becoming more common[14]. Some instances of pain were thought to be ACNES[15]. To the best of our knowledge, this is the first report of ACNES induced by a laparoscopic procedure being treated successfully with ultrasound-guided rectus sheath block. Ultrasound-guided rectus sheath block is a potential solution to the etiology of ACNES itself. Effective treatment is needed for ACNES, and ultrasound-guided rectus sheath block may be an important part of the armamentarium.
| 1. | Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, Tai YP, Li MK. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002;235:313-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 200] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 2. | Tan S, Wu G, Zhuang Q, Xi Q, Meng Q, Jiang Y, Han Y, Yu C, Yu Z, Li N. Laparoscopic versus open repair for perforated peptic ulcer: A meta analysis of randomized controlled trials. Int J Surg. 2016;33 Pt A:124-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Joris JL, Georges MJ, Medjahed K, Ledoux D, Damilot G, Ramquet CC, Coimbra CI, Kohnen LP, Brichant JF. Prevalence, characteristics and risk factors of chronic postsurgical pain after laparoscopic colorectal surgery: Retrospective analysis. Eur J Anaesthesiol. 2015;32:712-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Scheltinga MR, Roumen RM. Anterior cutaneous nerve entrapment syndrome (ACNES). Hernia. 2018;22:507-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Chrona E, Kostopanagiotou G, Damigos D, Batistaki C. Anterior cutaneous nerve entrapment syndrome: management challenges. J Pain Res. 2017;10:145-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | van Assen T, Boelens OB, Kamphuis JT, Scheltinga MR, Roumen RM. Construction and validation of a questionnaire distinguishing a chronic abdominal wall pain syndrome from irritable bowel syndrome. Frontline Gastroenterol. 2012;3:288-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Siawash M, Roumen R, Ten WTA, van Heurn E, Scheltinga M. Diagnostic characteristics of anterior cutaneous nerve entrapment syndrome in childhood. Eur J Pediatr. 2018;177:835-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Takada T, Ikusaka M, Ohira Y, Noda K, Tsukamoto T. Diagnostic usefulness of Carnett's test in psychogenic abdominal pain. Intern Med. 2011;50:213-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Boelens OB, Scheltinga MR, Houterman S, Roumen RM. Management of anterior cutaneous nerve entrapment syndrome in a cohort of 139 patients. Ann Surg. 2011; 254: 1054-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Boelens OB, Scheltinga MR, Houterman S, Roumen RM. Randomized clinical trial of trigger point infiltration with lidocaine to diagnose anterior cutaneous nerve entrapment syndrome. Br J Surg. 2013;100:217-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Sahoo RK, Nair AS. Ultrasound Guided Transversus Abdominis Plane Block for Anterior Cutaneous Nerve Entrapment Syndrome. Korean J Pain. 2015;28:284-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 12. | Batistaki C, Saranteas T, Adoni A, Kostopanagiotou G. Ultrasound-guided anterior abdominal cutaneous nerve block for the management of bilateral abdominal cutaneous nerve entrapment syndrome (ACNES). Pain Physician. 2013;16:E799-E801. [PubMed] |
| 13. | Lam KHS, Hung CY, Chiang YP, Onishi K, Su DCJ, Clark TB, Reeves KD. Ultrasound-Guided Nerve Hydrodissection for Pain Management: Rationale, Methods, Current Literature, and Theoretical Mechanisms. J Pain Res. 2020;13:1957-1968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 14. | Macrae WA. Chronic pain after surgery. Br J Anaesth. 2001;87:88-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 478] [Cited by in RCA: 441] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 15. | Smelt H, Pouwels S, Apers JA, Said M, Smulders J. Anterior Cutaneous Nerve Entrapment Syndrome: Two Case Reports of the Forgotten Diagnosis After Bariatric Surgery. Cureus. 2020;12:e8499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Japanese Society of Anesthesiologists, 00006209.
Specialty type: Anesthesiology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Feng J, Zhang XQ S-Editor: Liu JH L-Editor: A P-Editor: Liu JH