Published online Mar 6, 2022. doi: 10.12998/wjcc.v10.i7.2294
Peer-review started: September 15, 2021
First decision: October 18, 2021
Revised: October 24, 2021
Accepted: January 25, 2022
Article in press: January 25, 2022
Published online: March 6, 2022
Processing time: 167 Days and 21.4 Hours
An infected hepatic cyst causes clinical symptoms, such as fever and abdominal pain. A cyst with a diameter > 10 cm increases the likelihood of exclusion symptoms in adjacent organs. Herein, we report a case of pancreatitis caused by an infected hepatic cyst.
The patient was an 88-year-old woman with a history of polycystic liver disease and a cyst > 10 cm in diameter. She was referred to our hospital for upper abdominal pain that persisted for four days before consultation. She had a fever of 37.4ºC, and a blood test showed a C-reactive protein level of 23 mg/dL. An infected hepatic cyst was diagnosed by abdominal ultrasonography, computed tomography, and magnetic resonance imaging. Antibacterial therapy and percutaneous cyst puncture did not elicit sufficient therapeutic effects. As the cyst growth continued, laparoscopic hepatic cyst fenestration was performed on hospitalization day 20. Thereafter, symptoms improved, and she was discharged on hospital day 31.
To our knowledge, this is the second case report of pancreatitis associated with hepatic cyst growth. Percutaneous cyst puncture and drainage or surgical therapy can be considered if a slight improvement with antibiotic therapy alone or exclusion of surrounding organs is observed. Further, attention is needed to avoid potential recurrence.
Core Tip: A giant infected hepatic cyst may cause exclusion pancreatitis. Thus, attention should be paid to the appearance of symptoms and elevation in the levels of pancreatic enzymes. In case of a slight improvement in clinical symptoms and imaging findings with antibiotic therapy alone or exclusion of surrounding organs, percutaneous cyst puncture and drainage or surgical therapy can be considered. Further, close follow-up is needed to avoid potential recurrence.
- Citation: Kenzaka T, Sato Y, Nishisaki H. Giant infected hepatic cyst causing exclusion pancreatitis: A case report. World J Clin Cases 2022; 10(7): 2294-2300
- URL: https://www.wjgnet.com/2307-8960/full/v10/i7/2294.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i7.2294
The gradual dilation of remnant abnormal intrahepatic bile ducts supposedly forms the hepatic duct from the embryonic period[1]. The prevalence of simple hepatic cysts is 4.5%-7%[2,3], and they tend to be more common in women than men at a ratio of 1.5:1[4]. They are often incidentally observed in adults aged ≥ 40 years who have undergone computed tomography (CT) and ultrasonography[5].
An infected hepatic cyst is a condition characterized by clinical symptoms such as fever and abdominal pain. Routes of infection include the biliary tract, hematogenous, nearby infection foci, trauma, and unknown[5]. Overall, the routes of infection are most commonly unknown[5]. The risk factors for infected hepatic cysts are female sex, age ≥ 40 years, diabetes mellitus, biliary calculus or stenosis, and post-pancreatic head duodenal surgery[5]. A cyst diameter > 10 cm increases the likelihood of exclusion symptoms in adjacent organs[6]. However, there are no previous reports involving the pancreas.
Herein, we report a case of pancreatitis caused by an infected hepatic cyst.
Upper abdominal pain, fever.
The patient was an 88-year-old woman who could independently perform activities of daily living. She had previously been diagnosed with polycystic liver disease, with a giant cyst > 10 cm in diameter. She was examined by a local doctor for upper abdominal pain that persisted for 4 d before consultation. She had a fever of 37.4ºC, and a blood test showed a C-reactive protein level of 23 mg/dL. She was referred to our hospital for further examination and treatment when abdominal ultrasonography indicated a giant hepatic cyst and intracystic debris. She had a history of hypertension and dyslipidemia. She was taking oral amlodipine 5 mg/d, azilsartan 20 mg/d, and rosuvastatin 2.5 mg/d. Her family history was unremarkable with respect to hepatic or renal cysts.
Her consciousness was clear during examination. Physical findings were as follows: Blood pressure 160/90 mmHg, pulse 94 bpm/regular, body temperature 37.7ºC, respiratory rate 19/min, and SpO2 97% (room air). The upper abdomen was protruded and soft during abdominal examination. No increase or decrease in bowel sounds was observed. The right hypochondriac region was tender, with no rebound pain, Murphy's sign, or pain from liver percussion.
Blood examination showed elevated leukocyte (5300/μL) and neutrophil (66.2%) levels. Similarly, she presented with aspartate aminotransferase level of 18 U/L, alanine aminotransferase level of 15 U/L, lactate dehydrogenase level of 153 U/L, amylase level of 31 U/L, C-reactive protein level of 28.3 mg/dL, and procalcitonin level of 5.89 ng/mL. Other test results are shown in Table 1.
| Parameter | Patient’s value | Reference value |
| White blood cell count (cells/µL) | 5300 | 4500-7500 |
| Neutrophils (%) | 66 | 42-74 |
| Lymphocytes (%) | 28 | 18-50 |
| Monocytes (%) | 6 | 1-10 |
| Hemoglobin (g/dL) | 10.7 | 11.3-15.2 |
| Platelet count/µL | 189 × 103 | 13-35 × 103 |
| Prothrombin time international normalized ratio | 11.5 | 0.80-1.20 |
| Activated partial thromboplastin time (s) | 34.9 | 26.9-38.1 |
| C-reactive protein (mg/L) | 28.3 | ≤ 0.60 |
| Total protein (g/dL) | 6.2 | 6.9-8.4 |
| Albumin (g/dL) | 3.0 | 3.9-5.1 |
| Total bilirubin (mg/dL) | 1.1 | 0.2-1.2 |
| Aspartate aminotransferase (U/L) | 18 | 11-30 |
| Alanine aminotransferase (U/L) | 15 | 4-30 |
| Lactase dehydrogenase (U/L) | 153 | 109-216 |
| Creatine kinase (U/L) | 34 | 40-150 |
| Blood urea nitrogen (mg/dL) | 25.8 | 8-20 |
| Creatinine (mg/dL) | 1.16 | 0.63-1.03 |
| Sodium (mEq/L) | 134 | 136-148 |
| Potassium (mEq/L) | 3.6 | 3.6-5.0 |
| Chloride (mEq/L) | 101 | 98-108 |
| Glucose (mg/dL) | 124 | 70-109 |
| Hemoglobin A1c (%) | 5.8 | 5.6-5.9 |
| Procalcitonin (ng/mL) | 5.89 | ≤ 0.60 |
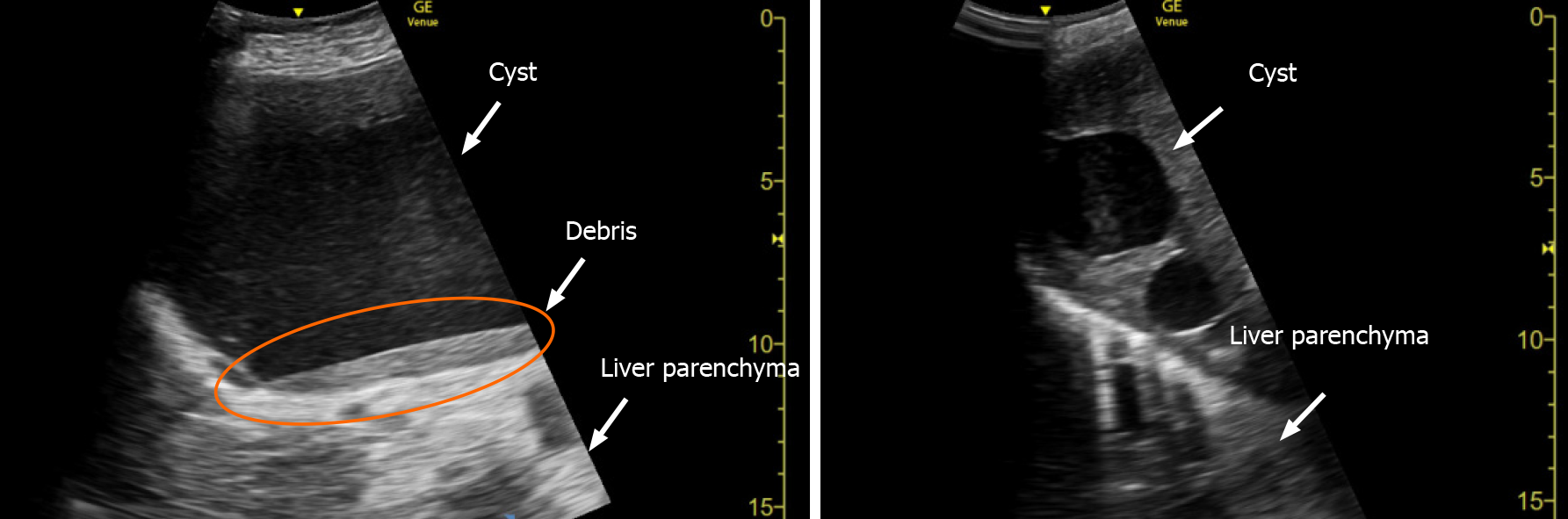
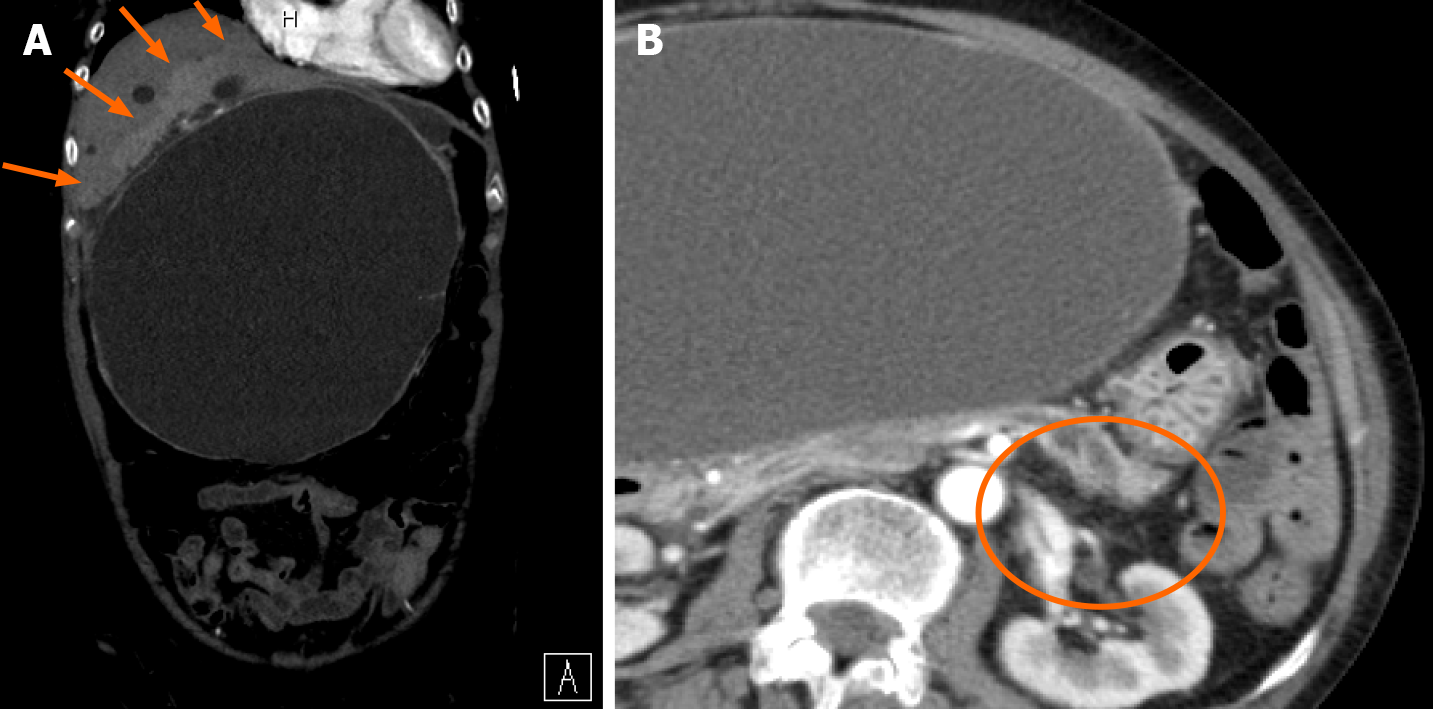
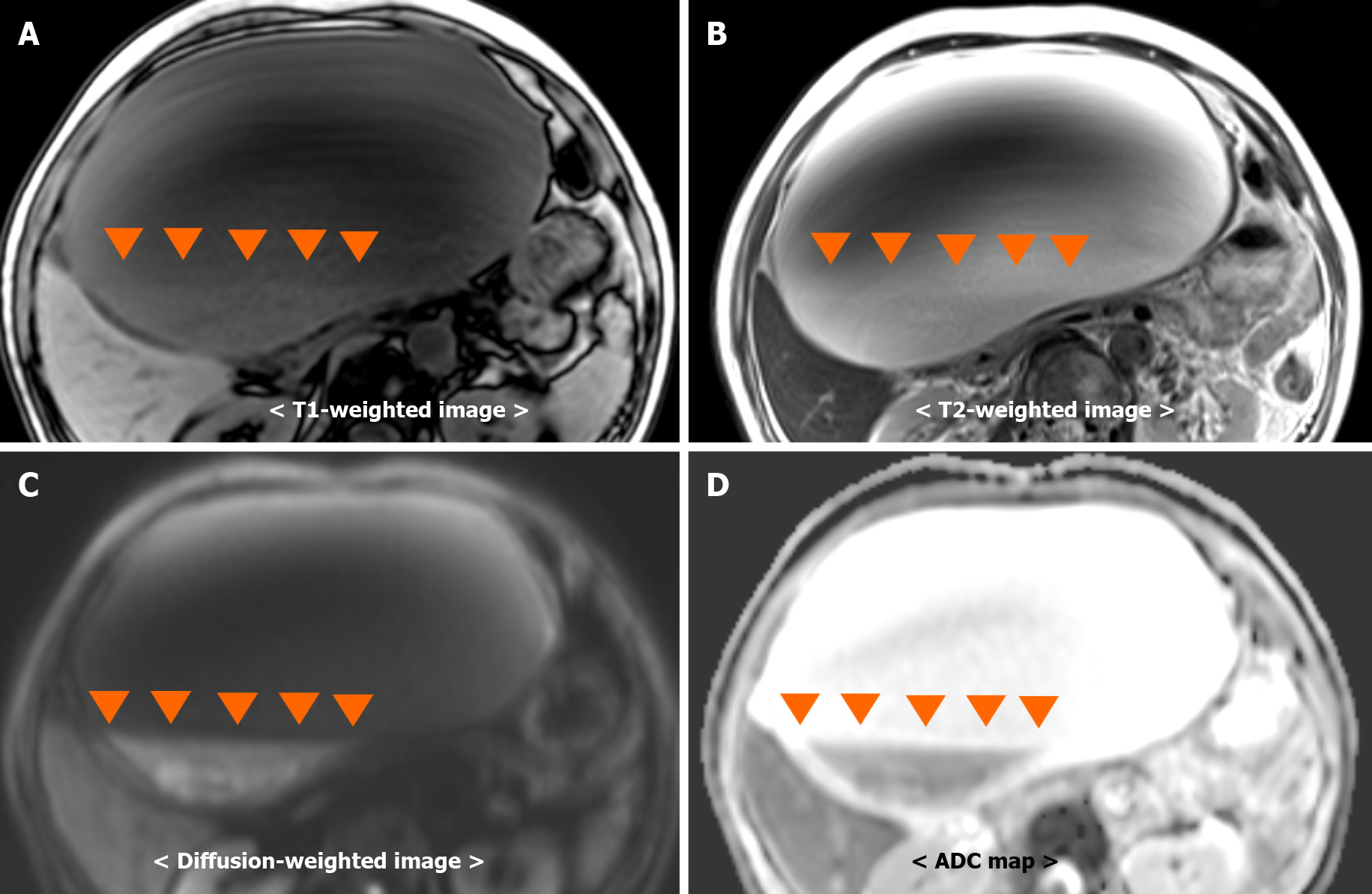
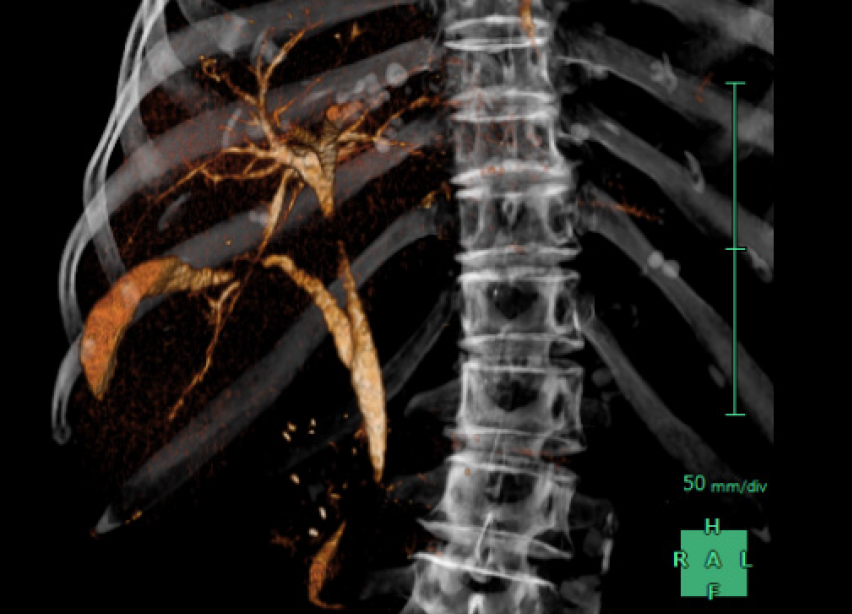
Abdominal ultrasonography revealed multiple cysts in the liver, including a giant one (Figure 1). A non-uniform hyperechoic region inside the cyst was considered debris. Abdominal dynamic CT revealed a contrast effect in the hepatic parenchyma around the cyst (Figure 2). There was no ring enhancement indicating an abscess. The maximum cyst diameter was 203 mm, and the main pancreatic duct at the pancreatic tail was slightly dilated. A simple abdominal magnetic resonance imaging showed a fluid-fluid level from the debris inside the hepatic cyst (Figure 3).
The patient was diagnosed with an infected hepatic cyst.
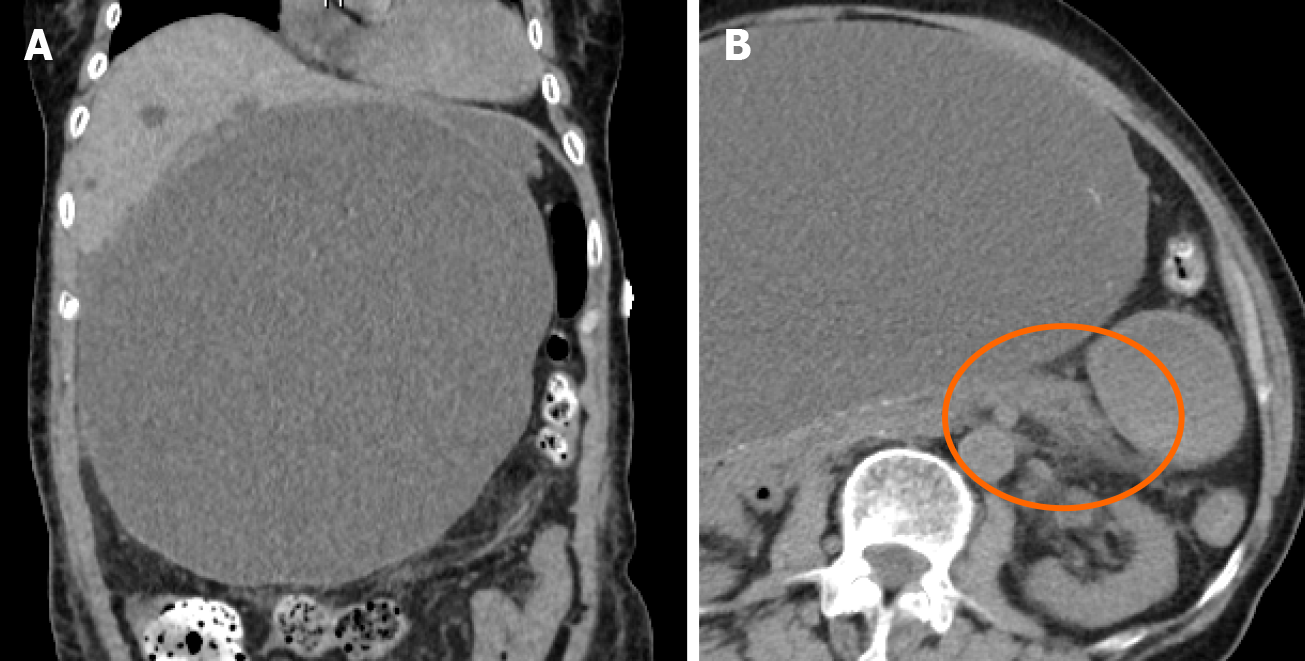
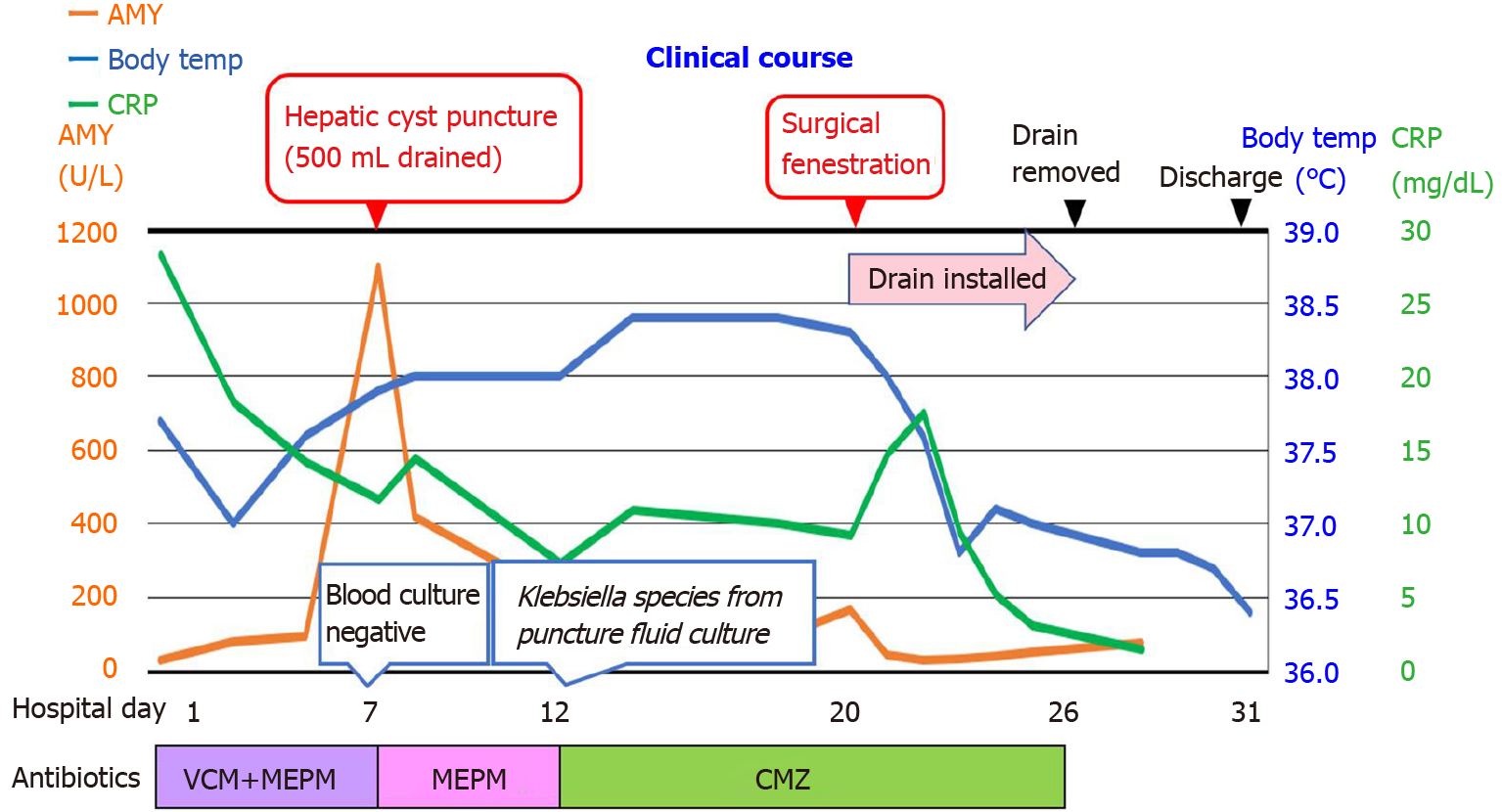
The patient was started on antibacterial therapy with vancomycin and meropenem. Both blood and urine cultures were negative. Despite the antibacterial therapy, her abdominal pain gradually worsened starting around hospitalization day 3. Back pain appeared on hospitalization day 7, and blood amylase and lipase levels increased to 1150 U/L and 850 U/L (reference value; 13-55 U/L), respectively. CT showed hepatic cyst growth, signs of pancreatic exclusion, dilation of the pancreatic duct, and increased adipose tissue density around the pancreas (Figure 4). In addition, three-dimensional drip infusion CT cholangiography showed no organic abnormalities in the common bile duct (Figure 5). These findings led to the diagnosis of exclusion pancreatitis. A percutaneous cyst puncture produced 500 mL of purulent fluid. Klebsiella was detected in a culture of the puncture fluid; therefore, the antibiotic was changed to cefmetazole. Despite the use of an effective antibiotic, cyst growth persisted. Therefore, on hospitalization day 20, we performed a laparoscopic hepatic cyst fenestration. Figure 6 shows the clinical course of the patient.
Thereafter, the abdominal symptoms, inflammatory response, and elevated levels of pancreatic enzymes improved, and the patient was discharged on hospitalization day 31. No recurrence was observed over the following year.
We report a case of exclusion pancreatitis associated with the growth of an infected hepatic cyst. To our knowledge, this is the second case report of pancreatitis occurring as organ damage associated with hepatic cyst growth. The other study referred to exclusion pancreatitis caused by a non-infected hepatic cyst[6].
Liver cysts with bacterial infections often have larger diameters[7]. A cyst diameter > 10 cm increases the chances of exclusion symptoms in adjacent organs[6]. Reported symptoms of exclusion include abdominal pain, nausea, vomiting, obstructive jaundice due to biliary obstruction[5], superior vena cava thrombosis[8], and acute pulmonary embolism[5]. Acute pancreatitis is extremely rare, and only a single case report describes it as being caused by a giant non-infected hepatic cyst[6]. In this case, pancreatitis improved with puncturing, indicating that the increased hepatic cyst size due to bacterial infection was responsible for acute exclusion pancreatitis.
When antibiotics are exclusively used to treat infectious hepatic cysts, the treatment success and recurrence rates are 30% and 20%, respectively[9]. The treatment success rates of combining antibiotics with percutaneous cyst puncture/drainage or surgery are 65% and 100%, respectively[9]. In this case, the giant hepatic cyst location on the hepatic margin made it difficult to install a drain during the first puncture. Therefore, only a single puncture was performed. The symptoms did not improve with antibiotic therapy alone and recurred after cyst puncture. Therefore, surgical fenestration was performed.
We reported a case of exclusion pancreatitis associated with the growth of an infectious hepatic cyst. In rare cases, a giant infected hepatic cyst may cause exclusion pancreatitis; therefore, the appearance of symptoms and elevation of pancreatic enzymes should be carefully observed. In case of poor improvement in clinical symptoms and imaging findings with antibiotic therapy alone or when there is exclusion of surrounding organs, percutaneous cyst puncture and drainage or surgical therapy can be considered. Given the possibility of recurrence, close follow-up is recommended.
| 1. | Cowles RA, Mulholland MW. Solitary hepatic cysts. J Am Coll Surg. 2000;191:311-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 74] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 2. | Caremani M, Maestrini R, Occhini U, Sassoli S, Accorsi A, Giorgio A, Filice C. Echographic epidemiology of cystic hydatid disease in Italy. Eur J Epidemiol. 1993;9:401-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Regev A, Reddy KR, Berho M, Sleeman D, Levi JU, Livingstone AS, Levi D, Ali U, Molina EG, Schiff ER. Large cystic lesions of the liver in adults: a 15-year experience in a tertiary center. J Am Coll Surg. 2001;193:36-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 74] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Surgery of the Liver and Biliary Tract (2nd ed). Churchill Livingstone Inc, 1994; p. 1197. |
| 5. | Miyamoto M, Oka M, Izumiya T, Nagaoka T, Ishihara Y, Ueda K, Enomoto S, Yanaoka K, Arii K, Tamai H, Shimizu Y, Ichinose M. Nonparasitic solitary giant hepatic cyst causing obstructive jaundice was successfully treated with monoethanolamine oleate. Intern Med. 2006;45:621-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Fantola G, Barth X, Monneuse O. Education and imaging. Hepatobiliary and pancreatic: Pancreatitis associated with a large hepatic cyst. J Gastroenterol Hepatol. 2010;25:1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Miyazato M, Tomiyama M, Natomi H, Shiroma Y, Yonamine K, Nishizawa M, Mabuchi H, Kinjou Y, Nakachi N, Shimajiri H, Tomiyama R. A study of 23 cases of infected liver cysts treated at our hospital. Kanzo. 2019;60:117-126. |
| 8. | Torzilli G, Santambrogio R, Vellini S, Palmisano A, Donadon M, Cornalba G, Montorsi M. Inferior vena cava thrombosis: an unusual complication of a large simple non-parasitic liver cyst requiring an integrated approach. Hepatogastroenterology. 2003;50:2188-2191. [PubMed] |
| 9. | Lantinga MA, Geudens A, Gevers TJ, Drenth JP. Systematic review: the management of hepatic cyst infection. Aliment Pharmacol Ther. 2015;41:253-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chen Y, Zhu CF S-Editor: Liu JH L-Editor: A P-Editor: Liu JH