Published online Feb 16, 2022. doi: 10.12998/wjcc.v10.i5.1592
Peer-review started: August 10, 2021
First decision: October 16, 2021
Revised: October 24, 2021
Accepted: January 11, 2022
Article in press: January 11, 2022
Published online: February 16, 2022
Processing time: 184 Days and 17.2 Hours
Unroofed coronary sinus syndrome (UCSS) is a rare congenital heart disease, which has variable morphologic features and is strongly associated with persistent left superior vena cava (PLSVC). However, it is often difficult to visualize the left-to-right shunt pathway through the CS by transthoracic echocardiography (TTE).
A 37-year-old female was admitted to the hepatological surgery department of a hospital with complaint of subxiphoid pain that had started 1 wk prior. Physical examination revealed a grade 3/6 systolic murmur at the left margin of the sternum, between the 2nd and 3rd intercostal cartilage. The patient underwent echocardiography and was diagnosed with ostium primum atrial septal defect (ASD); thus, she was subsequently transferred to the cardiovascular surgery department. A second TTE evaluation before surgery showed type IV UCSS with secundum ASD. Right-heart contrast echocardiography (RHCE) showed that the right atrium and right ventricle were immediately filled with microbubbles, but no microbubble was observed in the CS. Meanwhile, negative filling was observed at the right atrium orifice of the CS and right atrium side of the secundum atrial septal. RHCE identified UCSS combined with secundum ASD but without PLSVC in this patient.
This rare case of UCSS highlights the value of TTE combined with RHCE in confirming UCSS with ASD or PLSVC.
Core Tip: Unroofed coronary sinus syndrome (UCSS) is difficult to diagnose. Transthoracic echocardiography (TTE) of a 37-year-old female revealed ostium primum atrial septal defect (ASD). A second TTE showed type IV UCSS with secundum ASD. Right-heart contrast echocardiography (RHCE) confirmed UCSS and ASD with no persistent left superior vena cava (PLSVC). The patient was misdiagnosed because the defect location was near the endocardial cushions, which was mistaken for a defect of the ostium primum atrial septum. This case highlights the special value of TTE and RHCE for a rare case of type IV UCSS combined with ASD but without PLSVC.
- Citation: Chen JL, Yu CG, Wang DJ, Chen HB. Misdiagnosis of unroofed coronary sinus syndrome as an ostium primum atrial septal defect by echocardiography: A case report. World J Clin Cases 2022; 10(5): 1592-1597
- URL: https://www.wjgnet.com/2307-8960/full/v10/i5/1592.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i5.1592
Unroofed coronary sinus syndrome (UCSS) is a rare congenital heart disease, in which left atrial to right atrial shunt occurs through a partial or complete defect of the roof of the CS[1]. UCSS has variable morphologic features and the clinical syndrome of UCSS varies from symptomless to severe right heart failure, which is mainly determined by the size of the defect between the CS and other associated anomalies, such as persistent left superior vena cava (PLSVC) and atrial septal defect (ASD). UCSS is strongly associated with PLSVC in about 75% of cases[2], and UCSS in the terminal portion (Kirklin and Barratt-Boyes type IV) without PLSVC or other anomalies is classified as a type of ASD, which comprises less than 1% of all ASD cases[1]. However, it is often difficult to visualize the left-to-right shunt pathway through the CS by transthoracic echocardiography (TTE), which can lead to misdiagnosis or a missed diagnosis[3].
We present a rare case of UCSS combined with secundum ASD but without PLSVC, which was misdiagnosed as ostium primum ASD identified by TTE.
A 37-year-old female was admitted to the hepatological surgery department of the hospital with subxiphoid pain that had started 1 wk prior.
The patient's symptoms of intermittent subxiphoid pain began 5 years prior and had recurred and worsened over the past week. She also reported having experienced chest distress occasionally.
Five years ago, the patient began having intermittent subxiphoid pain and was hospitalized due to subxiphoid pain for 1 wk. Ultrasound examination showed a gallstone. Physical examination revealed grade 3/6 systolic murmur at the left margin of the sternum, between the 2nd and 3rd intercostal cartilage. Laboratory examination showed increased arterial partial pressure of oxygen (PaO2; 146 mmHg) but normal partial pressure of carbon dioxide (PCO2; 146 mmHg) and oxygen saturation (SaO2; 99%).
The patient had no previous or family history of similar illnesses.
Physical examination revealed grade 3/6 systolic murmur at the left margin of the sternum, between the 2nd and 3rd intercostal cartilage.
Blood analyses showed increased arterial PaO2 (146 mmHg) but normal PCO2 (146 mmHg) and SaO2 (99%).
The patient underwent echocardiography and was diagnosed with ostium primum ASD; thus, she was subsequently transferred to the cardiovascular surgery de-partment.
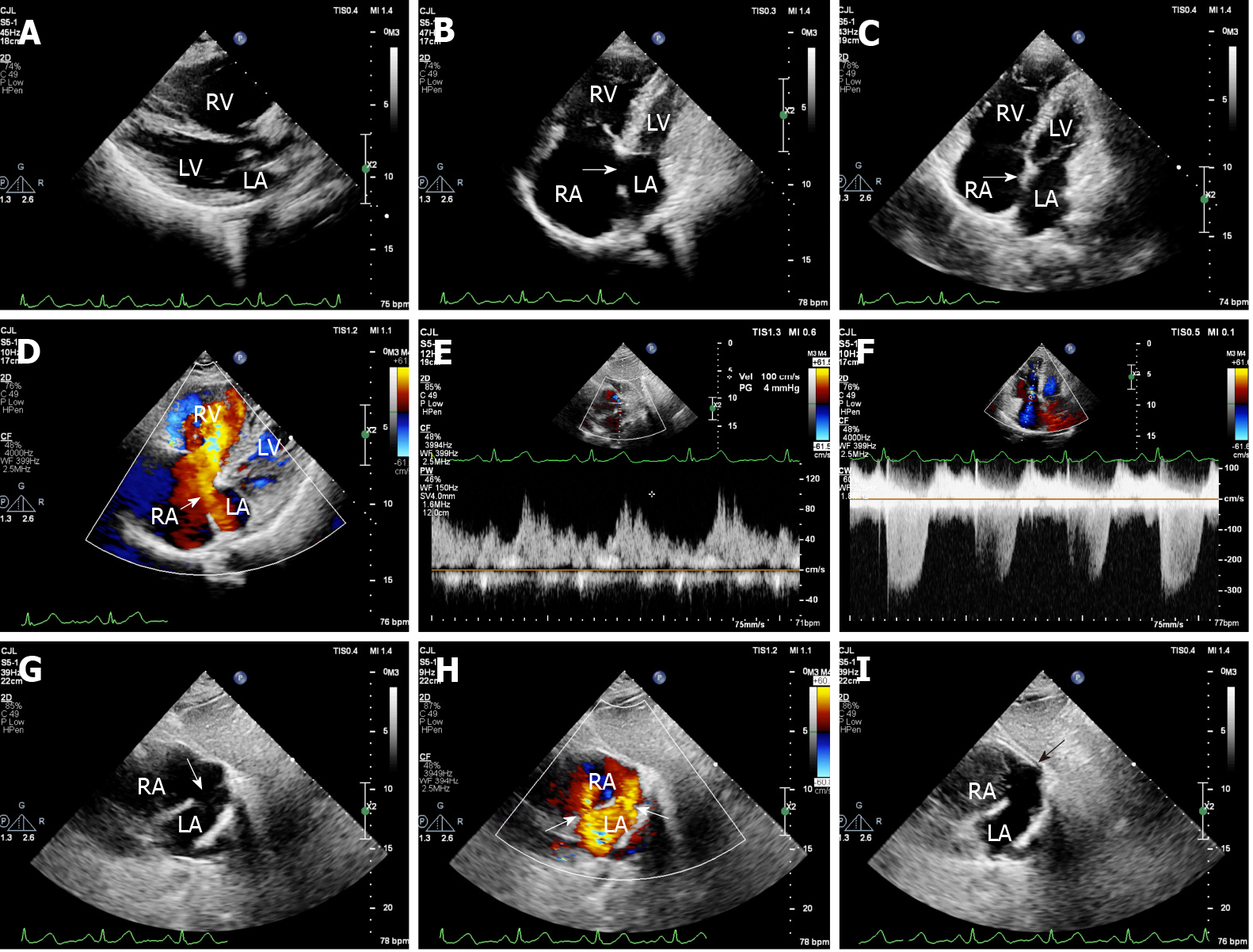
Before surgery, TTE was performed again. TTE showed: Enlargement of the right heart and pulmonary artery, with mildly increased systolic pulmonary arterial flow [velocity 177 cm/s, pressure gradient (PG) 12.5 mmHg]; moderate-to-severe tricuspid valve regurgitation; mild-to-moderate pulmonary hypertension [pulmonary arterial systolic pressure (PASP) 56 mmHg]; a secundum ASD (1.1 cm); and obvious broadening of the CS, with partial defect of the CS roof (3.3 cm × 2.0 cm), through which the left atrial to right atrial shunt occurred (velocity 100 cm/s, PG 4 mmHg) (Figures 1A-1H). There was no ectopic pulmonary vein drainage.
To find evidence of PLSVC, which is the most common associated anomaly, right-heart contrast echocardiography (RHCE) was performed. After agitated 50% glucose was injected into the left antecubital vein, the right atrium and right ventricle were immediately filled with microbubbles but no microbubble was observed in the CS. Negative filling was observed at the right atrium orifice of the CS and right atrium side of the secundum atrial septum. The microbubbles were not observed in the left ventricle or the left atrium. RHCE did not identify PLSVC in this patient (Figure 1I).
Chest X-ray examination showed an increased heart shadow and no abnormality in the aorta, but the pulmonary artery segment showed extrusion.
Pulmonary function tests showed that the diffusing capacity of the lung for carbon monoxide was mildly decreased (78%), but the forced expiratory volume in 1 s and ratio of forced expiratory volume to forced vital capacity remained normal.
Electrocardiogram (ECG) examination showed that the patient had sinus rhythm, a normal ECG axis, and incomplete right bundle branch block.
No genetic testing was performed.
No multidisciplinary expert consultation was conducted.
Type IV UCSS combined with secundum ASD.
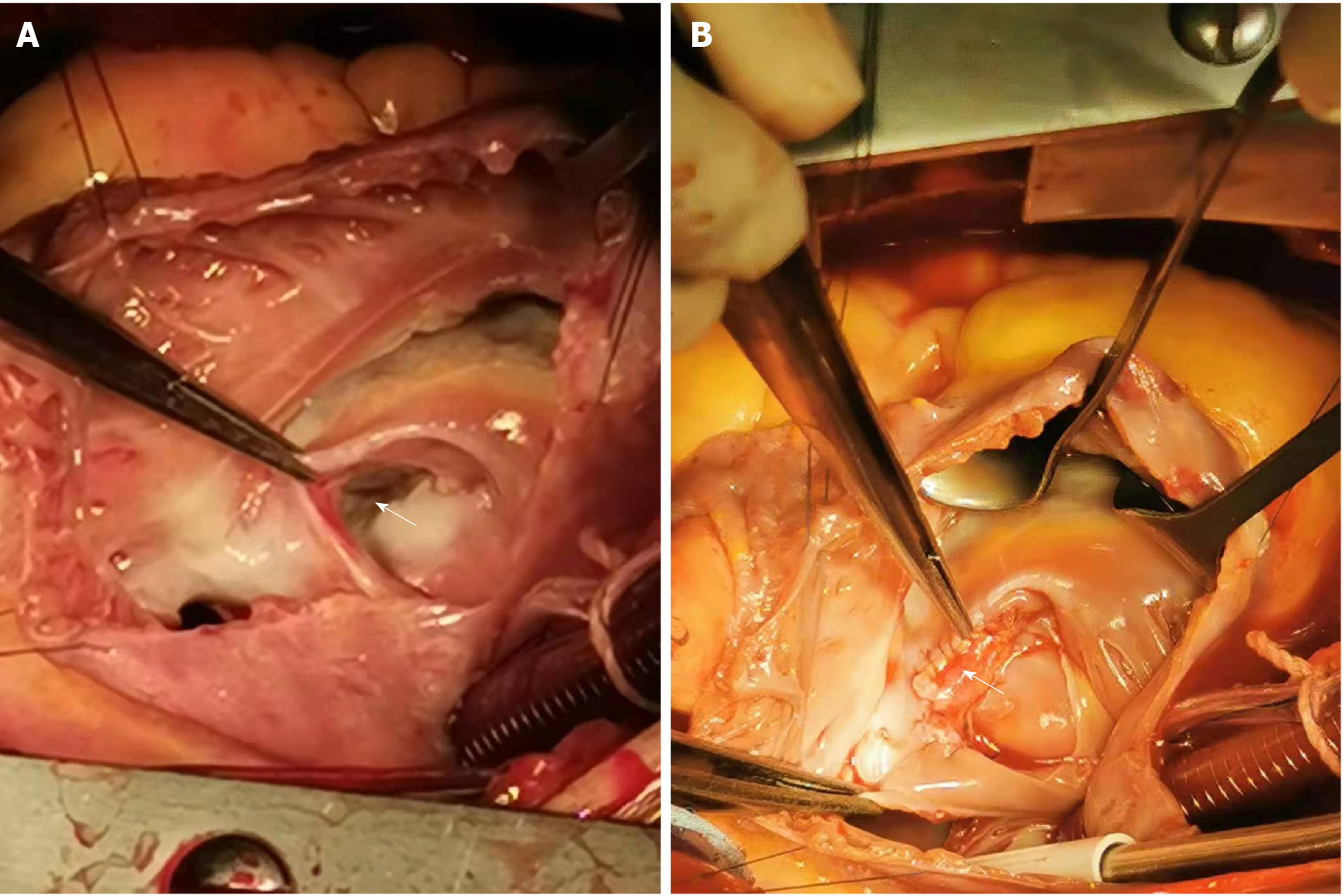
The patient underwent repair surgery for the CS roof defect, secundum ASD closure, and tricuspid annuloplasty. During the operation, obvious broadening of the CS with partial defect of the roof of the CS (3.0 cm × 2.1 cm) and secundum ASD near the oval foramen (1.1 cm) were detected (Figures 2A and 2B). When perfused through the CS, the perfusate reflowed to both the left atrium and right atrium. The moderate-to-severe tricuspid valve regurgitation was due to a significantly dilated tricuspid annulus.
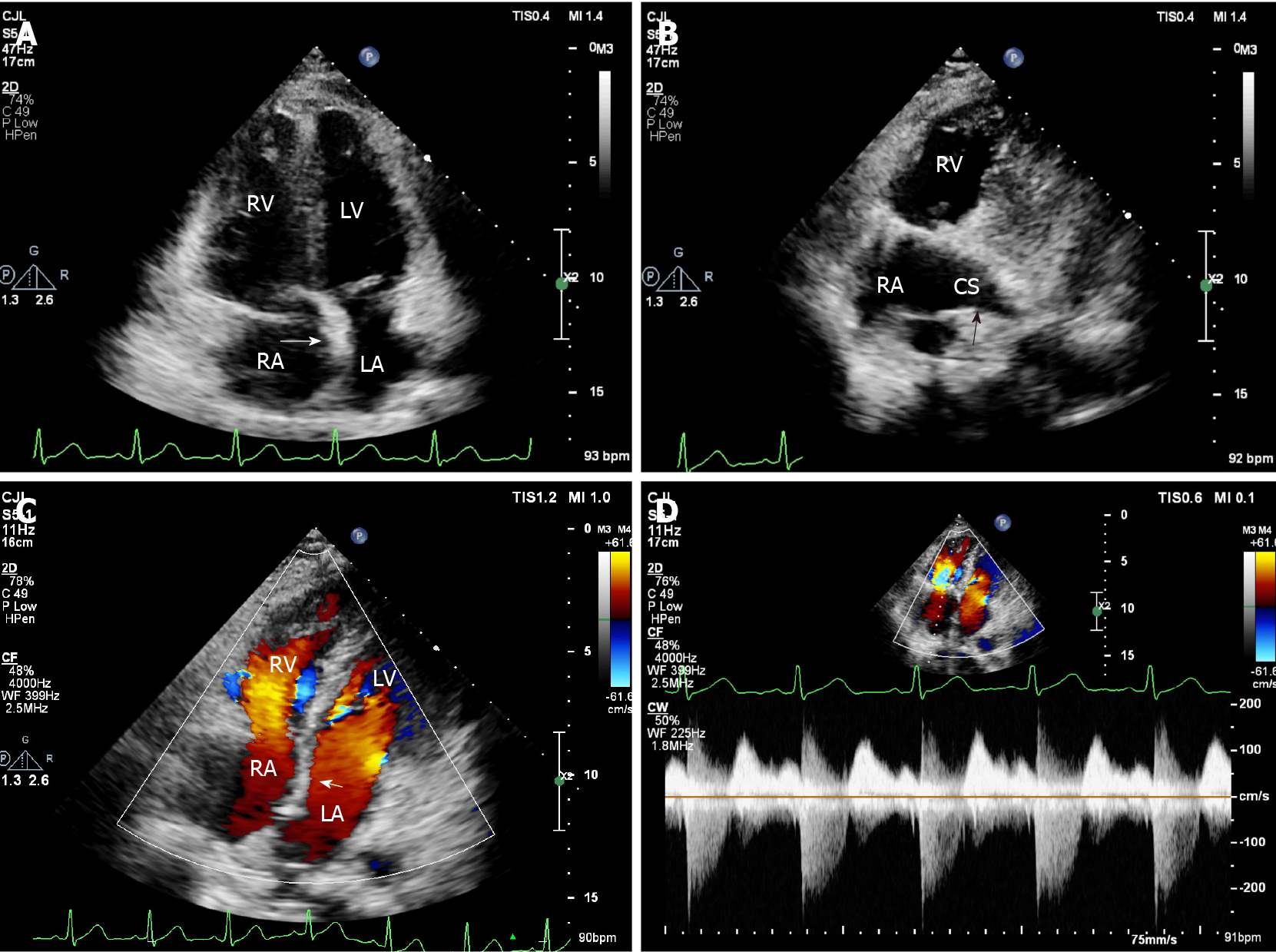
The patient was in good condition and no complications occurred after surgery. The patient was discharged from the hospital about 2 wk after surgery. TTE before discharge showed no shunt through the UCSS or ASD from the left atrium to right atrium, mild tricuspid valve regurgitation (velocity 223 cm/s, PG 20 mmHg), and normal PASP (25 mmHg) (Figures 3A-3D). At the 6-mo follow-up visit, the patient was in good condition.
UCSS is a rare congenital heart disease characterized by communication between the CS and the left atrium through the partial or complete absence of the CS roof. According to the location of the absence, UCSS is classified into the following four morphological types: Completely unroofed with PLSVC (type I); completely unroofed without PLSVC (type II); partially unroofed in the midsection (type III); and partially unroofed in the terminal portion (type IV)[1,4].
In general, UCSS is strongly associated with a PLSVC, which remains the most common association[2]. Moreover, it can also be associated with other congenital heart abnormalities, such as cor triatriatum, canal defects, tetralogy of Fallot, abnormal atrioventricular connection, pulmonary atresia or stenosis, and anomalous pulmonary venous return[5].
TTE is the most widely used noninvasive technique for the diagnosis of UCSS; although posterior structures such as the pulmonary veins or CS may not be seen well in some patients. RHCE using agitated saline or glucose injection through the left arm vein may help indicate PLSVC, the most common association which is characterized by microbubbles in the CS prior to its appearance in the right atrium.
However, it is not easy to determine the type of UCSS due to difficulties in detecting the exact location of the unroofed portion. In the present case, the defect of CS was partially unroofed in the terminal portion (type IV); this UCSS type was misdiagnosed at the first TTE because the location of the defect was near the endocardial cushions on apical four-chamber view, which was mistaken for a defect of the ostium primum ASD. On the second TTE, the defect of the CS in the terminal portion and normal endocardial cushions were detected on apical four-chamber view by scanning backward. Moreover, the CS was significantly dilated and the CS roof structure was not always seen while a shunt from the left atrium was passed through the dilated CS to the right atrium. All evidence led to the diagnosis of UCSS. Meanwhile, a small shunt through the secundum ASD was detected, with the exception of an atrial-level UCSS shunt.
In the present case, RHCE worked in two ways. When injected through the left arm vein, microbubbles first entered the right atrium but no microbubble appeared in the CS, indicating that there was no PLSVC. Moreover, negative filling was observed at the right atrium orifice of the CS and right atrium side of the secundum atrial septal during RHCE, confirming the diagnosis of UCSS and secundum ASD. Although TTE of suitable image sections is the first-line examination to evaluate UCSS, it should be more frequently used in combination with RHCE in these cases.
We highlight a rare case of type IV UCSS combined with secundum ASD but without PLSVC, which was misdiagnosed as ostium primum ASD identified by TTE. TTE combined with RHCE is of value in confirming UCSS with or without ASD and PLSVC.
| 1. | Ootaki Y, Yamaguchi M, Yoshimura N, Oka S, Yoshida M, Hasegawa T. Unroofed coronary sinus syndrome: diagnosis, classification, and surgical treatment. J Thorac Cardiovasc Surg. 2003;126:1655-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 116] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Kim H, Choe YH, Park SW, Jun TG, Kang IS, Yang JH, Eo H, Lee HJ. Partially unroofed coronary sinus: MDCT and MRI findings. AJR Am J Roentgenol. 2010;195:W331-W336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Lee HS, Song BG, Park MJ, Kim KH, Ok HS, Kim BK, Chun WJ, Oh JH. Rare case of an unroofed coronary sinus. Heart Lung. 2012;41:390-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Xie MX, Yang YL, Cheng TO, Wang XF, Li K, Ren PP, Lü Q, Lin H, Li L. Coronary sinus septal defect (unroofed coronary sinus): echocardiographic diagnosis and surgical treatment. Int J Cardiol. 2013;168:1258-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Samuel W, Robert EM. Atrial septal defect, unroofed coronary sinus surgical treatment, e-medicine Cardiothoracic surgery. 2009. |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ong LT S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ