Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12375
Peer-review started: August 11, 2022
First decision: September 25, 2022
Revised: October 20, 2022
Accepted: October 26, 2022
Article in press: October 26, 2022
Published online: November 26, 2022
Processing time: 104 Days and 7.3 Hours
Screening colonoscopies are routinely performed and have low occurrences of adverse events such as perforation, bleeding, infection, and post-polypectomy syndrome. True device related adverse events are rarely reported in the literature.
We report a case of a 51-year-old patient without past medical history who presented for her first screening colonoscopy. The patient was thought to have friable mucosa in the cecum and oozed upon water irrigation during screening colonoscopy. It was later identified that the colonoscope used during the index procedure had malfunctioned and produced a pin-point water jet which damaged the colon mucosa of cecum. The maintenance service identified a piece of rubber fragment lodged in the instrument component at the tip of the scope, resulting in high pressure water jet. Repeat colonoscopy with a functioning colonoscope confirmed normal colon mucosa without friability.
This is the first report of mucosa injury from a colonoscope water jet malfunction. Endoscopists should recognize the potential for endoscopic malfunction.
Core Tip: We report a case of colon mucosal injury due to a colonoscope water jet malfunction. During a screening colonoscopy, a patient was found to have friable oozing colon mucosa upon water irrigation. We later found that the water jet of the colonoscope was abnormally narrow with high pressure, resulting in mucosal injury. Removal of a piece of rubber lodged at the tip of the scope normalized the water pressure. The patient’s subsequent colonoscopy showed normal colon mucosa. This is the first reported case of iatrogenic injury from a colonoscope water jet malfunction.
- Citation: Patel P, Chen CH. Colon mucosal injury caused by water jet malfunction during a screening colonoscopy: A case report. World J Clin Cases 2022; 10(33): 12375-12379
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12375.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12375
Screening colonoscopies are routinely performed to prevent colon cancer by detecting and removing precancerous polyps and by the early detection of colon cancer. Devices currently approved for screening colonoscopies offer excellent diagnostic and therapeutic abilities while meeting safety standards[1]. Known adverse events related to colonoscopy include perforation, bleeding, infection, and post-polypectomy syndrome[2]. Perforation is the most feared complication which occurs mostly in recto-sigmoid colon and its rate has been estimated to be 0.02%-0.08%, depending on the indication for colonoscopy[3]. However, true device-related adverse events are rare and upon literature review, we only identified cases related to infection transmission through endoscopes[4]. Current endoscopic system has an integrated water jet connected through an external irrigation pump to assist with endoscopic visualization[5]. To date, there has been no safety report of a water jet related adverse event. Here, we report a case of colon mucosal injury related to malfunction of the water jet.
A 51-year-old female presented for her first asymptomatic screening colonoscopy.
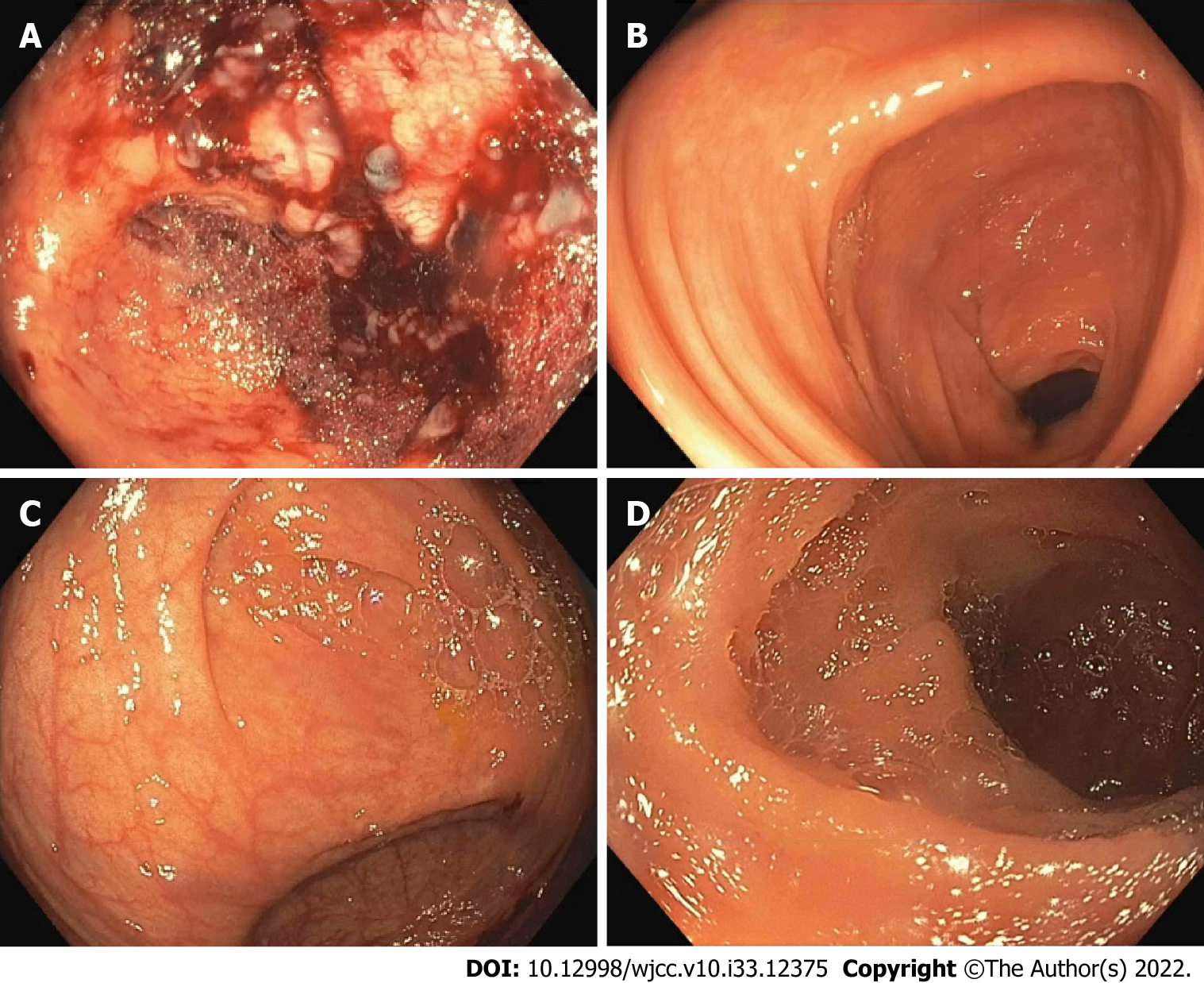
The patient underwent bowel preparation with SUPREPTM split prep, and the procedure was performed with monitored anesthesia care using propofol. During the colonoscopy, her cecum was thought to be friable and oozed upon water irrigation to clear the debris. Despite prolonged and copious irrigation, clear visualization of the cecum could not be achieved due to mucosal friability (Figure 1A). The rest of the colon was clear, without debris that would require cleansing with water jet, and appeared to have normal mucosa (Figure 1B).
Later in the same endoscopy unit, during a colonoscopy on another patient, a different endoscopist found that the water jet of the colonoscope (Olympus, CF-HQ190L) had a very narrow stream of water, which resulted in focal mucosal damage and hemorrhage upon irrigation. After the procedure, the scope was identified to be the same scope used in the previous case with “cecal mucosal friability”. The high water pressure generated from the sharp pin-point water jet was the suspected cause of mucosal damage. When the scope was sent for repair, the maintenance service found that a piece of rubber was lodged in the hole of C-Cover (an instrument component at the tip of the scope) which resulted in a sharper water stream. The water pressure was very high but normalized after the piece of rubber was removed. That piece of rubber was a component of the scope which broke off and lodged there.
No known past medical conditions.
No family history of colon cancer.
No abnormalities were noted on the abdominal exam.
Normal hemoglobin value of 13.4 g/dL, and normal platelets count of 320 K/cumm. Other values of basic chemistries and of a complete blood panel were within normal limits.
No relevant imaging data.
Iatrogenic colon mucosa injury due to water jet malfunction.
Given that the colonoscopy finding was due to a water jet malfunction, no specific therapy or treatment was given or needed.
Three months later, the patient underwent a repeat colonoscopy and had a normal terminal ileum and normal mucosa of the entire colon, including of the cecum (Figure 1C and D). The patient did have a 2 mm sessile polyp at the cecum base that was removed with cold biopsy forceps. The pathology showed that the polyp was a tubular adenoma. It is possible that this polyp was not seen during the index colonoscopy due to limited visualization in the setting of extensive mucosal injury. There were no other abnormalities found in the colon during this examination.
To our knowledge, we have not identified any other case of water irrigation related mucosal injury in the literature. The manufacturer of the scope, Olympus, also was not aware of prior similar incident (personal communication). This case highlights the importance of recognizing the potential for iatrogenic mucosa damage from a high-pressure water jet. When the water-jet pressure is high enough, the water stream can penetrate the mucosa and into the submucosal space. In fact, pin-point high-pressure water jets have been utilized in commercial products for needle-free submucosal injection to create a submucosal cushion (for example, HybridAPC, Erbe United States). Water jets have also been used extensively as a hydrosurgery dissecting tool for burn wound debridement[6]. Endoscopists should be aware of the power of high-pressure water jets, their potential application, and the possibility of iatrogenic damage.
In our endoscopy unit, all endoscopes undergo routine maintenance and processing as recommended by the manufacturer. Nevertheless, endoscopists or endoscopy lab staff should still check the endoscope and water jet before procedures to ensure proper instrument function. To recognize the high-pressure narrow water jet stream during the instrument check, awareness and vigilance are required. In addition, this case highlighted the need for studies to identify the threshold of water pressure that the mucosa can withstand without injury, as well as additional safety measures that include checking the water jet and pressure before procedures. We hope that the publication of this case report will increase awareness of this uncommon but important issue so it can be detected before procedures are conducted and thus avoid potential damage and complications.
In our case, the high water jet pressure was caused by a piece of rubber lodged in the scope. The piece of rubber was a component of the scope that broke off and lodged under the C-Cover. Given its location, it would not be possible to see or find the piece of rubber during inspection or brushing during reprocessing of the scope. Although this incident was not preventable, we were able to link the patient with cecal mucosal damage to the scope with water jet malfunction because in our endoscopic unit the identification number of every scope utilized is meticulously documented. From the standpoint of patient safety and quality improvement, it is very important to document the scope identification number so that any potential adverse event is traceable, and the patients involved can be contacted as needed.
In summary, we report a case of iatrogenic colon mucosa damage from high-pressure water jet due to colonoscope malfunction. Endoscopists should be vigilant to recognize this potential endoscopic complication.
| 1. | ASGE Technology Committee. High-definition and high-magnification endoscopes. Gastrointest Endosc. 2014;80:919-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Kim SY, Kim HS, Park HJ. Adverse events related to colonoscopy: Global trends and future challenges. World J Gastroenterol. 2019;25:190-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 91] [Cited by in RCA: 188] [Article Influence: 26.9] [Reference Citation Analysis (9)] |
| 3. | Rai V, Mishra N. Colonoscopic Perforations. Clin Colon Rectal Surg. 2018;31:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Ofstead CL, Heymann OL, Quick MR, Eiland JE, Wetzler HP. Residual moisture and waterborne pathogens inside flexible endoscopes: Evidence from a multisite study of endoscope drying effectiveness. Am J Infect Control. 2018;46:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 89] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 5. | Nakano T, Sato C, Sakurai T, Kamei T, Nakagawa A, Ohuchi N. Use of water jet instruments in gastrointestinal endoscopy. World J Gastrointest Endosc. 2016;8:122-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (2)] |
| 6. | Ziegler B, Fischer S, Pieper D, Mathes T, Kneser U, Hirche C. Evidence and Trends in Burn Wound Debridement: An Evidence Map. Plast Surg (Oakv). 2020;28:232-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ko J, South Korea; Nakamura K, Japan; Serban ED, Romania; Sulbaran MN, Brazil; Tan Y, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH