Published online Nov 16, 2022. doi: 10.12998/wjcc.v10.i32.11921
Peer-review started: June 20, 2022
First decision: September 9, 2022
Revised: September 22, 2022
Accepted: October 17, 2022
Article in press: October 17, 2022
Published online: November 16, 2022
Processing time: 132 Days and 2.3 Hours
Primary tracheobronchial mucoepidermoid carcinoma (MEC), derived from salivary mucus glands, is an uncommon neoplasm in adults. At present, surgery is still the preferred treatment for adult bronchial MEC, although it may cause significant trauma and loss of lung function. Here, we report a patient with endobronchial MEC who received the interventional bronchoscopic therapy to remove the neoplasm and no recurrence occurred during follow-up.
A 28-year-old man was admitted to our unit with mild hemoptysis for 3 d. Physical examination did not show any abnormal signs, and the serological indexes were all in the normal range. Chest computed tomography (CT) indicated an intraluminal nodule in the bronchus intermedius with homogeneous density and a well-defined margin. Upon fiberoptic bronchoscopy, an endobronchial pedunculated polypoid was discovered without submucosal involvement. As the neoplasm was confined to the bronchus, interventional bronchoscopy was performed to remove the mass by high-frequency electric knife and laser resection. Tissue was sampled and histopathological examination confirmed the diagnosis of low-grade MEC. As the proliferation index was low, no further treatment was given. During 2 years of follow-up, the patient’s condition was good and no relapse was discovered under fluorescence bronchoscopy or CT scan.
Interventional bronchoscopy can be considered for treatment of low-grade bronchial MEC, with few complications and preserved lung function.
Core Tip: At present, surgery is still the mainstay of treatment for primary pulmonary mucoepidermoid carcinoma (MEC), although it will cause significant trauma and loss of lung function. We report a case with MEC in the bronchus intermedius who received interventional bronchoscopy to remove the mass successfully. Our results indicate the effectiveness and safety of the interventional bronchoscopic therapy in the treatment of low-grade bronchial MEC.
- Citation: Ding YM, Wang Q. Endoscopic resection of bronchial mucoepidermoid carcinoma in a young adult man: A case report and review of literature. World J Clin Cases 2022; 10(32): 11921-11928
- URL: https://www.wjgnet.com/2307-8960/full/v10/i32/11921.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i32.11921
Primary pulmonary mucoepidermoid carcinoma (MEC) is a rare airway tumor of salivary glands in adults, constituting only 0.1%-0.2% of primary lung malignancies[1]. MECs are characterized by a combination of intermediate cell types with myxopoiesis, a gland, and squamous epithelial cells and are classified based on histology into low- and high-grade groups[2]. The treatment of pulmonary MEC is usually surgical by traditional resection, sleeve lobectomy, or pneumonectomy performed with an open or video-assisted technique. For low-grade MEC, surgical resection is considered the first-line treatment, which can lead to complete recovery and excellent prognosis[3,4]. However, for tracheobronchial patients whose tumors are in the large airways, surgical resection may inevitably impair lung function and cause considerable trauma, which make the treatment challenging. Recently, interventional bronchoscopic therapy has attracted considerable attention in the treatment of bronchial MEC because of its few complications and preservation of lung function[5,6].
We present a 28-year-old male patient with symptom of hemoptysis, whose computed tomography (CT) showed a mass in the bronchus intermedius. Interventional bronchoscopic therapy was performed to eradicate the neoplasm successfully. The patient was eventually diagnosed with low-grade MEC and no further treatment was given. At 2 years of follow-up, he showed no recurrence. A literature review of the application of interventional bronchoscopic therapy in the treatment of MEC is also provided.
A 28-year-old man with mild hemoptysis for 3 d came to our unit in April 2020.
The symptoms started 3 d ago, once or twice daily. The patient denied cough, chest pain, fever or respiratory distress.
The patient had normal growth and no previous hemoptysis.
The patient had no history of smoking, allergy or specific disease. He had no family history of tumor.
The physical examination did not show any abnormal signs.
Routine blood tests indicated normal counts of white blood cells, neutrophils, hemoglobin and platelets. The tumor markers including carcinoma embryonic antigen (CEA) (1.47 g/L), neuron-specific enolase (12.24 g/L) and squamous cell carcinoma antigen (1.2 g/L) were all in the normal range. The serum C-reactive protein, the coagulation tests including prothrombin time, activated partial thromboplastin time and D-dimer were all normal. The antinuclear antibodies, erythrocyte sedimentation rate and myocardial enzyme were also negative.
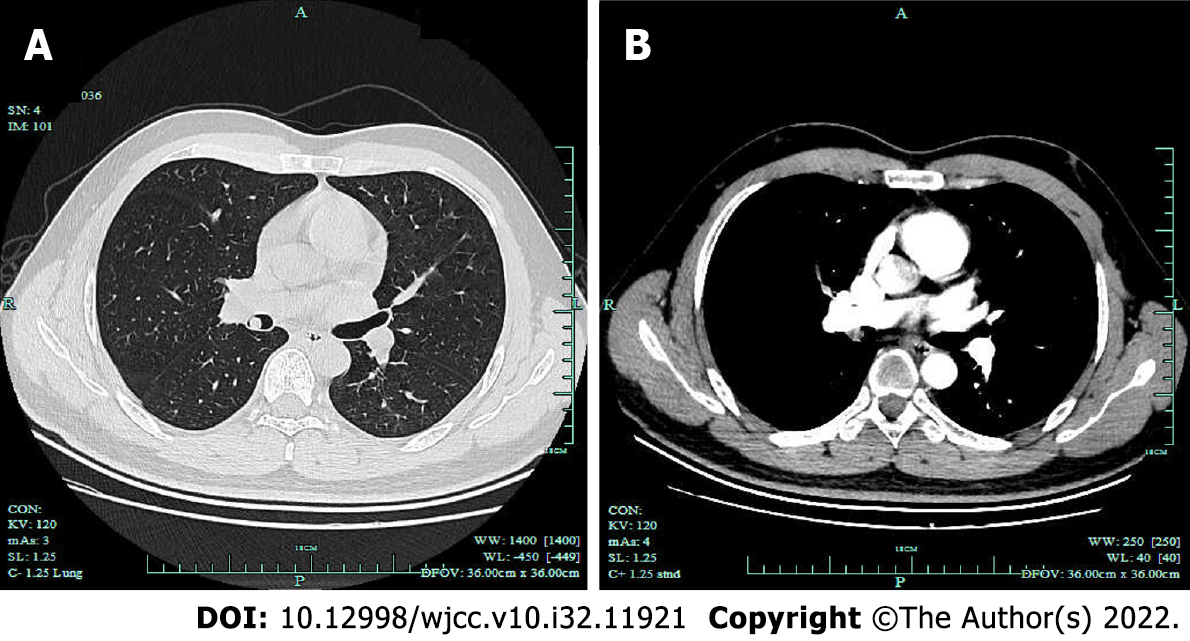
Contrast-enhanced chest CT was performed and showed a 9-mm intraluminal nodule in the bronchus intermedius with homogeneous density, well-defined margin and moderate enhancement (Figure 1). No mediastinal lymph nodes were enlarged according to CT. Following CT, the patient underwent bronchoscopy, which revealed an endobronchial pedunculated polypoid confined in the bronchus intermedius with rich vascularity and no submucosal involvement.
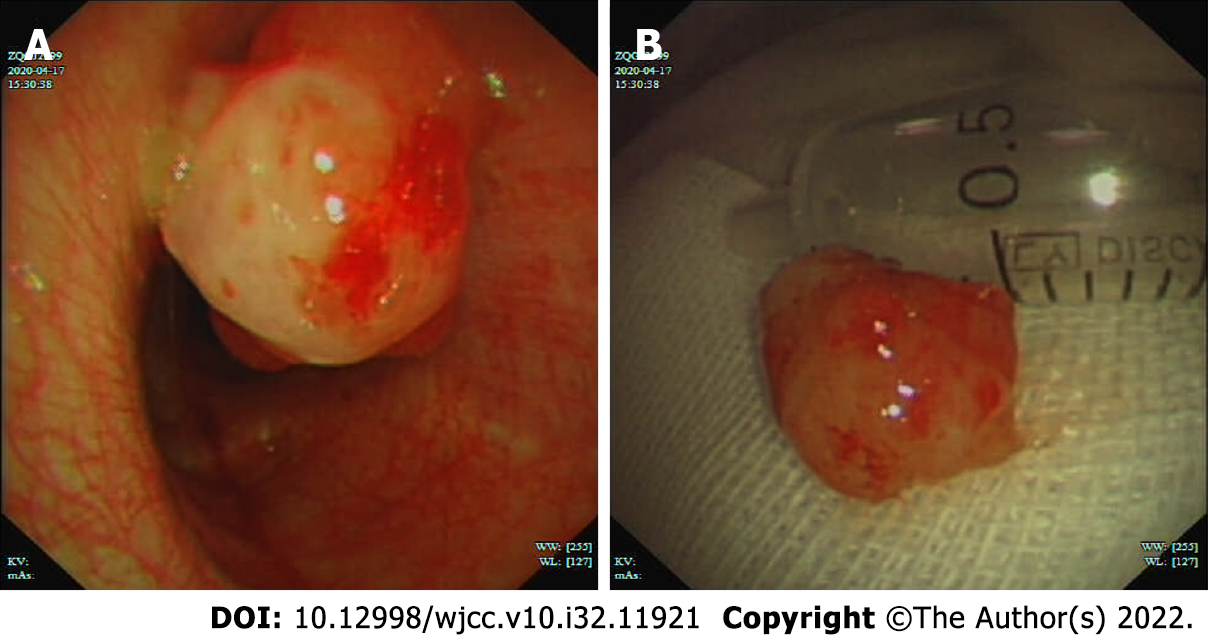
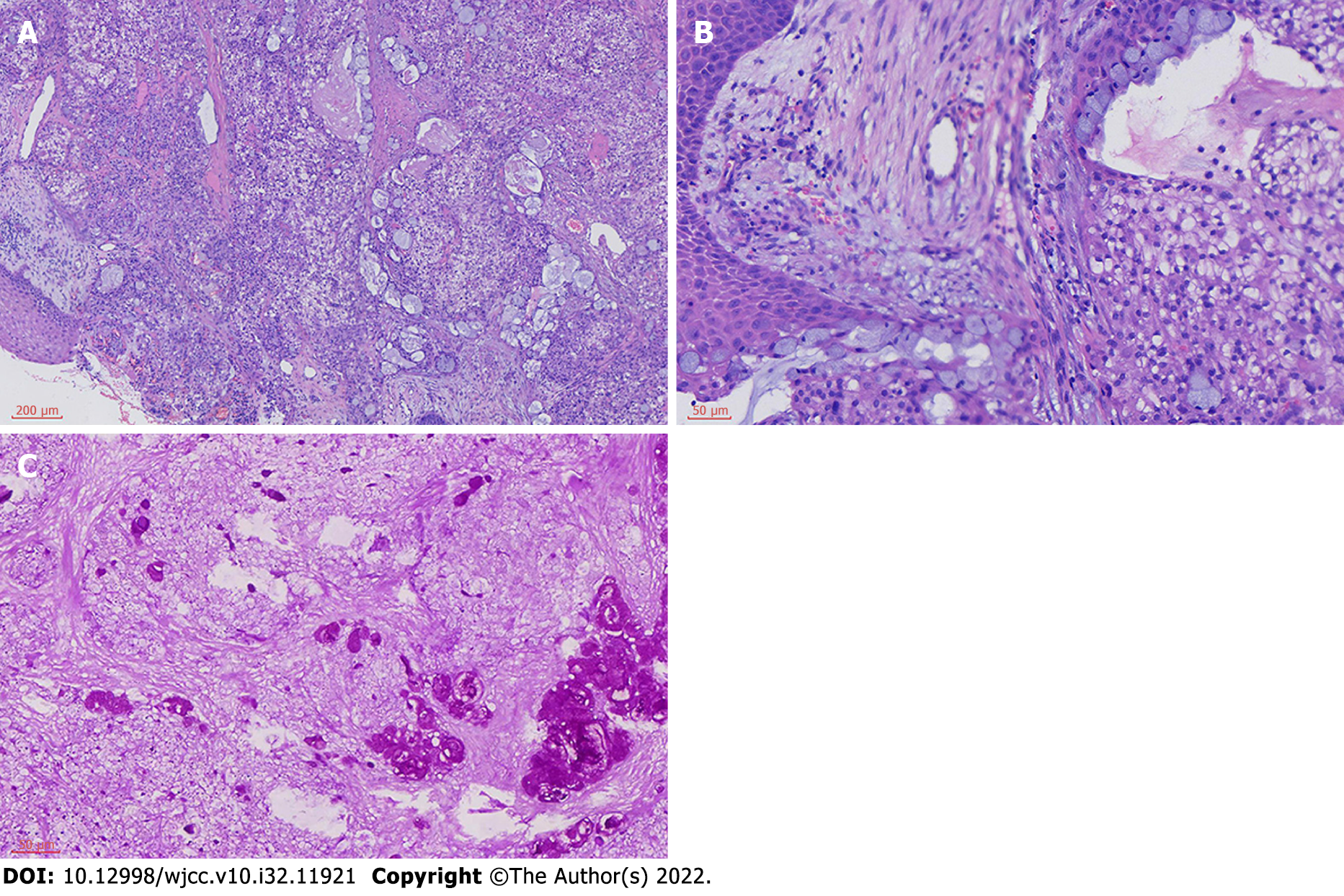
Interventional bronchoscopy was performed by high-frequency electric knife and laser resection to remove the mass (Figure 2). The tumor mass was sampled, and histopathologic analysis revealed tumor cells that included epidermoid, mucous, and intermediate cells, with moderately pleomorphic, moderate mucus secretion, and low proliferation index (Figure 3). Additional immunohistostaining was positive for P63, CKpan, epithelial membrane antigen (EMA), CEA and negative for smooth muscle actin (SMA), calponin and S100. Fluorescence in situ hybridization performed on the specimens didn’t detect the MAML2 rearrangement. Based on these findings, we considered the final diagnosis was low-grade MEC.
As the patient was diagnosed low-grade MEC, no further treatment was given. After interventional bronchoscopic therapy, the patient felt well, and the hemoptysis was relieved.
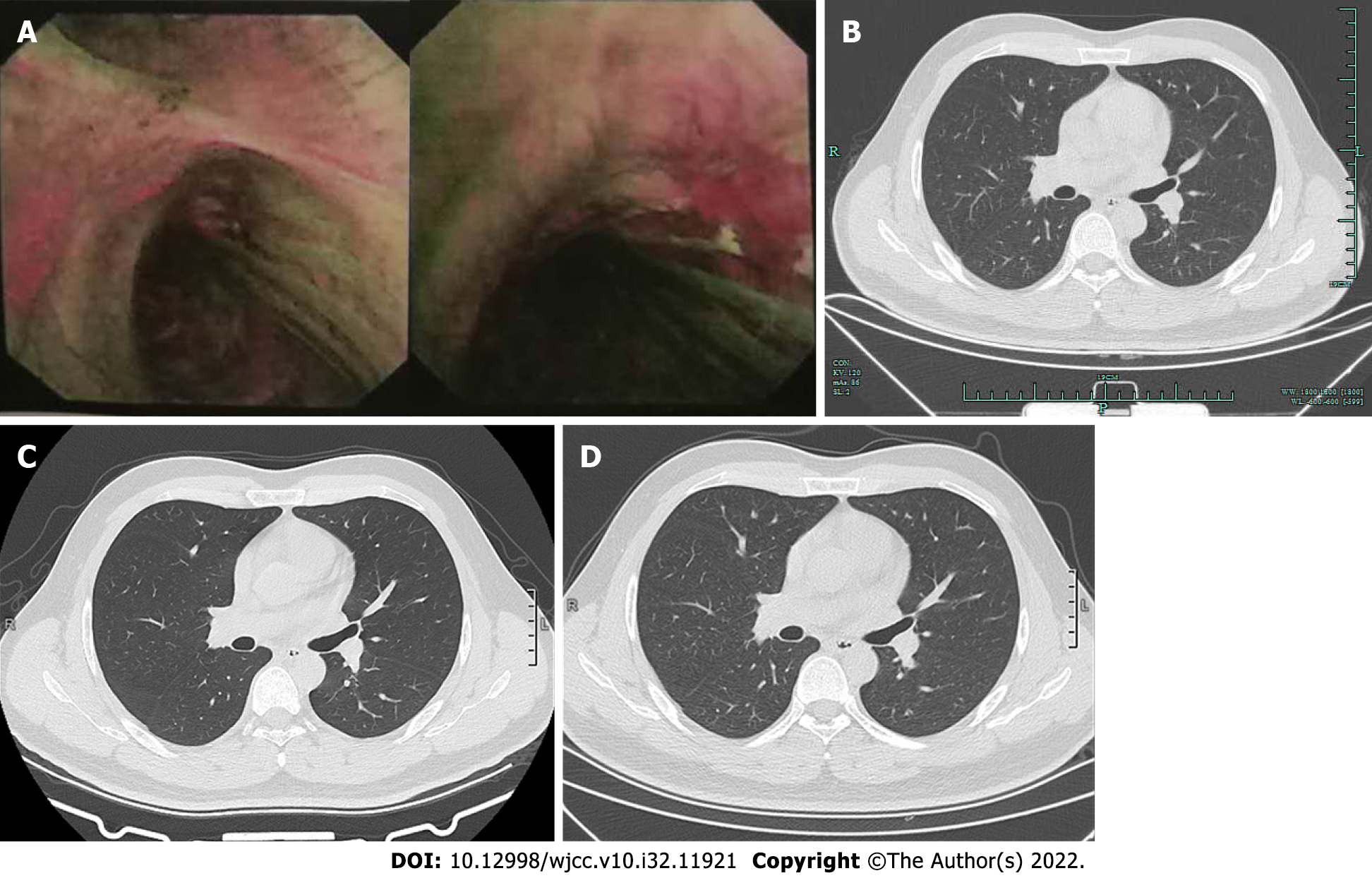
After 3 mo, follow-up fluorescence bronchoscopy was performed and showed normal mucosa (Figure 4A). During follow-up of 2 years, the patient was in good general condition and chest CT was performed periodically at 6 mo (Figure 4B), 19 mo (Figure 4C) and 2 years (Figure 4D) with no signs of relapse.
Primary pulmonary MEC is an uncommon disease, accounting for < 1% of all lung cancers. According to the World Health Organization classification of tumors, MEC is defined as a salivary gland-type tumor characterized by a combination of mucus-secreting, squamous and intermediate cell types[1,7]. Pulmonary MEC affects people of all ages but mostly young patients. In a series of 56 cases published by Fois et al[8], > 50% of the patients were under 30 years of age, and the mean age was 34 years. The case presented here was a young male patient.
Since these neoplasms mainly involve the lobular or segmental bronchi, the symptoms and signs are consistent with large airway obstruction, that is, cough, hemoptysis, bronchitis, wheezing, asthmatic symptoms and nonresolving pneumonia[9-12]. One-third of patients are asymptomatic. Less than 5% of low-grade MECs spread to lymph nodes, and high-grade MECs commonly metastasize distantly[13].
Common findings of MEC on chest radiographs manifested with nodules inside the lobar or segmental lumen, often associated with obstruction, that is, postobstructive pneumonia/pulmonary abscess, subsegmental atelectasis, mucoid impaction and obstructive emphysema[14]. The tumor’s appearance includes a circumferential or elevated soft tissue nodule with either a smooth or polypoid margin[15]. Ban et al[16] reported that MEC usually showed a hilar type, well-defined margin, regular shape and marked heterogeneous contrast enhancement. Patchy areas of low density can be observed in MEC, and calcification has a low incidence[17]. High-grade MEC may have heterogeneous density, lobular contours, and poorly defined margins[18]. Chen et al[19] revealed an uncommon sign of pulmonary MEC with cystic airspace, which might indicate early and rapid metastasis. In our case, the patient’s chest CT showed an oval, well-circumscribed and homogeneous mass within the bronchus intermedius with moderate enhancement.
Flexible bronchoscopy represents the main diagnostic tool for MECs, as it may allow direct visualization of the lesions and biopsies. The fiber optic bronchoscopy view of a MEC tumor usually appear as pedunculated, polypoidal, smooth, exophytic mass with rich vascularity[20]. Immunostaining was positive for p63, EMA, cytokeratin (CK)7, CK5/6 and negative for TTF-1, SMA, S100 and calponin[21,22]. The CRTC1/CRTC3-MAML2 fusion transcripts are present in approximately 33.7%-69.7% in cases of MEC[23]. Several studies have demonstrated the fusion might signal a better prognosis[23,24]. However, some subsequent studies showed that the fusion may occur infrequently in high-grade cases[25] and was not correlated with tumor grade or survival[26,27]. In our case, the MAML2 rearrangement was negative, but we still observed a good prognosis of the patient during 2 years follow-up.
Prognosis of MEC depends on the pathological grade and TNM staging. As opposed to high-grade MEC, the prognosis of low-grade MEC is excellent[28]. Shen et al’s[29] retrospective study of 45 patients showed 100% of the overall 5-year survival rates compared with 69.1% between the TNM stage I and stage II-IV, and 3-year survival rates of 100% in the low-grade patients vs 81.8% in high-grade patients. Old age, large lesions, metastases, high ki-67 index and poor differentiation were considered to be the independent prognostic factors for worse survival[30,31]. Komiya et al’s study suggested that the tumor in the main bronchus or upper lobe had significantly decreased 5-year disease-specific survival rate[32].
At present, surgical resection is still the first-line treatment for bronchial MEC. Surgical resection of low-grade MEC can lead to complete recovery and good prognosis[3,4,33]. However, since MEC usually grows in large airways, surgery may pose a significant loss of lung function with serious postoperative complications. In addition, the tumor in large airways may cause significant respiratory distress that may make the patient unsuitable for surgery. Bronchoscopic intervention has attracted extensive attention in the treatment of MEC patients over the past few years. Multiple bronchoscopic interventions including rigid bronchoscopy, argon plasma coagulation, CO2 cryotherapy, and electric loop can be conducted to remove the mass. Zhang et al[34] reported the effectiveness and safety of bronchoscopic interventions for patients with low-grade intratracheal MEC with rare bronchoscopy-associated complications. Yang et al[35] reported 4 children with low-grade MEC under bronchoscopic resection. No major bleeding or pneumothorax occurred during or after operation. Chen et al[36] retrospectively analyzed 11 adult patients with bronchial MEC and found that the symptoms of all patients improved significantly after bronchoscopic interventions without serious complications such as bleeding, pneumothorax or mediastinal emphysema. Kim et al[37] collected patients with primary pulmonary salivary gland-type tumors, including 12 MEC patients, and found no significant difference in overall survival between the surgery and bronchoscopic intervention groups in patients with low-grade MEC. For more serious cases, one-fifth of the patients need bronchoscopic intervention as a bridge therapy before surgery because of respiratory distress. Moreover, there were several case reports indicating the promising effect of interventional bronchoscopy for treatment of bronchial MEC[38,39]. In this case, we also found that interventional bronchoscopy could successfully eradicate the neoplasm and provide good prognosis for the patient without significant trauma. Although these retrospective studies had small samples, and only a few case reports discuss interventional bronchoscopic therapy as the main treatment for MEC, we consider that, for low-grade MEC, since it is usually superficial and restricted to the bronchus, bronchoscopic intervention can completely eradicate the mass with few complications, preserve lung function and provide good prognosis similar to that of surgery. For high-grade bronchial MEC, interventional bronchoscopic therapy could quickly relieve life-threatening obstruction as a bridge therapy prior to surgery. For bronchial MEC with distant metastasis, bronchoscopic intervention can provide significant palliative relief of patients’ respiratory distress and improve life quality.
We present a case of bronchial MEC that was successfully treated with interventional bronchoscopy. Since bronchial intervention has few complications and avoids loss of lung function, more applications can be expected in the treatment of bronchial MEC, especially in bronchial low-grade MEC. More prospective studies with larger samples are required to further evaluate its effectiveness and safety.
The authors thank Zhe-Yan Yu for her help in collecting patient’s data and obtaining the patient’s consent for publication.
| 1. | Kalhor N, Moran CA. Pulmonary mucoepidermoid carcinoma: diagnosis and treatment. Expert Rev Respir Med. 2018;12:249-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Zhang Y, Liu X, Gu Y, Zhang S. Clinical, laboratory, pathological, and radiological characteristics and prognosis of patients with pulmonary salivary gland-type tumors. J Cancer Res Clin Oncol. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 3. | Hsieh CC, Sun YH, Lin SW, Yeh YC, Chan ML. Surgical outcomes of pulmonary mucoepidermoid carcinoma: A review of 41 cases. PLoS One. 2017;12:e0176918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (1)] |
| 4. | Bishnoi S, Puri HV, Asaf BB, Pulle MV, Kumar A. Lung preservation in mucoepidermoid carcinoma of tracheobronchial tree: A case series. Lung India. 2021;38:18-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | Kimura M, Miyajima K, Ishikawa R, Yamada Y, Kono T, Okunaka T, Iwaya K, Ikeda N. Photodynamic therapy for pulmonary mucoepidermoid carcinoma. Respir Med Case Rep. 2021;33:101431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Zhang QC, Ouyang WJ, Zhang XJ. Bronchoscopic intervention for a patient with bronchial mucoepidermoid carcinoma. Chin Med J (Engl). 2020;133:1501-1502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Falk N, Weissferdt A, Kalhor N, Moran CA. Primary Pulmonary Salivary Gland-type Tumors: A Review and Update. Adv Anat Pathol. 2016;23:13-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Fois AG, Diana G, Arcadu A, Marras V, Crivelli P, Putzu C, Ginesu GC, Canu S, Pirina P. Bronchial mucoepidermoid carcinoma: A case report. Int J Surg Case Rep. 2017;31:159-162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Tri TT, Vu LT, My TT, Thach PN, Duc NM. Mucoepidermoid lung carcinoma in a pediatric patient confused with pneumonia. Radiol Case Rep. 2021;16:2749-2753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Vu LT, Duc NM, Tra My TT, Bang LV, My LT, Phuong Thuy LT, Sy HV. Pulmonary mucoepidermoid lung carcinoma in pediatric confused with asthma. Respir Med Case Rep. 2021;33:101471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 11. | Murakami T, Fujita Y, Takamura K, Taniguchi S, Fukuyama C, Marutsuka K, Shimamoto T. Tracheal Mucoepidermoid Carcinoma Mimicking Deteriorated Bronchial Asthma during Pregnancy. Case Rep Obstet Gynecol. 2021;2021:7259496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Shiiba R, Himeji D, Beppu K, Marutsuka K, Mitsuoka M, Nabeshima K. Bronchial mucoepidermoid carcinoma, recurrent asthmatic symptoms, and pneumonia presenting in pregnancy. Respirol Case Rep. 2020;8:e00626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Omesh T, Gupta R, Saqi A, Burack J, Khaja M. A rare case of endobronchial mucoepidermoid carcinoma of the lung presenting as non-resolving pneumonia. Respir Med Case Rep. 2018;25:154-157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 14. | Han X, Zhang J, Fan J, Cao Y, Gu J, Shi H. Radiological and Clinical Features and Outcomes of Patients with Primary Pulmonary Salivary Gland-Type Tumors. Can Respir J. 2019;2019:1475024. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Cheng DL, Hu YX, Hu PQ, Wen G, Liu K. Clinicopathological and multisection CT features of primary pulmonary mucoepidermoid carcinoma. Clin Radiol. 2017;72:610.e1-610.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 16. | Ban X, Shen X, Hu H, Zhang R, Xie C, Duan X, Zhou C. Predictive CT features for the diagnosis of primary pulmonary mucoepidermoid carcinoma: comparison with squamous cell carcinomas and adenocarcinomas. Cancer Imaging. 2021;21:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Li X, Yi W, Zeng Q. CT features and differential diagnosis of primary pulmonary mucoepidermoid carcinoma and pulmonary adenoid cystic carcinoma. J Thorac Dis. 2018;10:6501-6508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Patel T, Arora P, Jakhetiya A, Pandey A. Left lower lobectomy for uncommon endobronchial mucoepidermoid carcinoma in a 15-year-old male. J Postgrad Med. 2021;67:241-242. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Chen Y, Zhang F, Chen X, Yan L, Zhang X, Zheng C. Rapid metastasis of stage IA primary pulmonary high-grade mucoepidermoid carcinoma with a cystic airspace: a case report and reflection. J Int Med Res. 2021;49:3000605211038137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Chin M, Gupta A, Gomes MM, Maziak D, Mulpuru S. Dyspnea, focal wheeze, and a slow growing endobronchial tumor. Respir Med Case Rep. 2021;32:101360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Zhou X, Zhang M, Yan X, Zhong Y, Li S, Liu J, Peng L, Gan X. Challenges in diagnosis of pulmonary mucoepidermoid carcinoma: A case report. Medicine (Baltimore). 2019;98:e17684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Mashiana S, Duarte EM. Metastatic mucoepidermoid carcinoma to the pleura: a case report. J Med Case Rep. 2022;16:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Salem A, Bell D, Sepesi B, Papadimitrakopoulou V, El-Naggar A, Moran CA, Kalhor N. Clinicopathologic and genetic features of primary bronchopulmonary mucoepidermoid carcinoma: the MD Anderson Cancer Center experience and comprehensive review of the literature. Virchows Arch. 2017;470:619-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Okumura Y, Nakano S, Murase T, Ueda K, Kawakita D, Nagao T, Kusafuka K, Urano M, Yamamoto H, Kano S, Tsukahara K, Okami K, Hanai N, Iwai H, Kawata R, Tada Y, Nibu KI, Inagaki H. Prognostic impact of CRTC1/3-MAML2 fusions in salivary gland mucoepidermoid carcinoma: A multiinstitutional retrospective study. Cancer Sci. 2020;111:4195-4204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Taniuchi M, Kawata R, Terada T, Higashino M, Nishimura H, Kurisu Y, Kuwabara H, Hirose Y. Management and outcome of parotid mucoepidermoid carcinoma by histological grade: A 21-year review. Laryngoscope Investig Otolaryngol. 2022;7:766-773. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Birkeland AC, Foltin SK, Michmerhuizen NL, Hoesli RC, Rosko AJ, Byrd S, Yanik M, Nor JE, Bradford CR, Prince ME, Carey TE, McHugh JB, Spector ME, Brenner JC. Correlation of Crtc1/3-Maml2 fusion status, grade and survival in mucoepidermoid carcinoma. Oral Oncol. 2017;68:5-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 27. | Saade RE, Bell D, Garcia J, Roberts D, Weber R. Role of CRTC1/MAML2 Translocation in the Prognosis and Clinical Outcomes of Mucoepidermoid Carcinoma. JAMA Otolaryngol Head Neck Surg. 2016;142:234-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 28. | Lin G, Liang H, Wang W, Liu J, Li J, Liang W, He J. Nomogram for predicting the survival rate of primary pulmonary mucoepidermoid carcinoma patients: a retrospective study based on SEER database. Ann Transl Med. 2021;9:407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Shen W, Yang T, Fan Y, Li X, Ai C, Wang X, Wang D, Zhou X. Pulmonary mucoepidermoid carcinoma: A clinicopathological study of 45 patients. Thorac Cancer. 2022;13:2385-2389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 30. | Qin BD, Jiao XD, Liu K, Wu Y, He X, Liu J, Zang YS. Clinical, pathological and treatment factors associated with the survival of patients with primary pulmonary salivary gland-type tumors. Lung Cancer. 2018;126:174-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 31. | Qiu L, Song P, Chen P, Wang H, Li F, Shu M, Gong GC, Song X, Huang C, Jia H, Li N, Zhang G. Clinical Characteristics and Prognosis of Patients With Pulmonary Mucoepidermoid Carcinoma: A SEER-Based Analysis. Front Oncol. 2021;11:601185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 32. | Komiya T, Perez RP, Yamamoto S, Neupane P. Primary lung mucoepidermoid carcinoma: analysis of prognostic factors using surveillance, epidemiology and end results program. Clin Respir J. 2017;11:847-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 33. | Wang Y, Cai S, Xue Q, Mu J, Gao Y, Tan F, Mao Y, Wang D, Zhao J, Gao S, He J. Treatment outcomes of patients with tracheobronchial mucoepidermoid carcinoma compared with those with adenoid cystic carcinoma. Eur J Surg Oncol. 2020;46:1888-1895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 34. | Zhang JL, Zhou YZ, Zhang N, Zou H, Wang HW, Liu JK, Li DM, Wang H, Lv J, Li CX, Mao JF. Different effects of bronchoscopic interventions on children and adults with tracheobronchial mucoepidermoid carcinoma. Tumori. 2022;108:134-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Yang HM, Yin J, Li G, Liu XC. [Clinical features and interventional bronchoscopic treatment of primary airway tumor in 8 children]. Zhonghua Er Ke Za Zhi. 2021;59:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 36. | Chen H, Zhang J, Qiu XJ, Wang J, Pei YH, Wang YL. Interventional Bronchoscopic Therapy in Adult Patients with Tracheobronchial Mucoepidermoid Carcinoma. Chin Med J (Engl). 2017;130:2453-2458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 37. | Kim BG, Lee K, Um SW, Han J, Cho JH, Kim J, Kim H, Jeong BH. Clinical outcomes and the role of bronchoscopic intervention in patients with primary pulmonary salivary gland-type tumors. Lung Cancer. 2020;146:58-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 38. | Zheng X, Herth FJF, Sun J. Initial Experience with Hybrid Argon Plasma Coagulation as a Novel Local Treatment Method for Tracheobronchial Mucoepidermoid Carcinoma. Respiration. 2019;98:461-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 39. | Hanif Khan A, Faisal M, Mohd Ali R, Abdul Rahaman JA. Resolution of asthmatic symptoms following successful endoscopic resection of tracheal mucoepidermoid carcinoma. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Respiratory system
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ait Addi R, Morocco; Andriolo LG, Italy; Gupta L, Indonesia; Ni W, United States S-Editor: Liu JH L-Editor: A P-Editor: Liu JH