Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11597
Peer-review started: July 1, 2022
First decision: September 5, 2022
Revised: September 15, 2022
Accepted: September 27, 2022
Article in press: September 27, 2022
Published online: November 6, 2022
Processing time: 117 Days and 14 Hours
Neurofibromatosis type 1 (NF-1) is a common autosomal dominant genetic disorder. It is characterized by café-au-lait spots and cutaneous neurofibromas. Although NF-1 typically involves the skin, nerves, bones, and eyes, vascular manifestation in the form of devastating hemorrhage can occur rarely.
We present the case of a 47-year-old female with NF-1 who had a ruptured right lower limb arterial malformation. She presented with sudden right lower limb swelling for two hours and symptoms of hemorrhagic shock on admission. The physical examination revealed a right lower limb presenting as elephantiasis and visible dark-brown pigmentation over a large area. Computed tomography angiography showed right lower limb arteriovenous malformation. Therefore, the patient underwent emergency right lower limb digital subtraction angiography (DSA) and vascular embolization after blood transfusions. However, after DSA, vascular embolization, and repeated blood transfusions, the anemia and right lower limb swelling and tenderness did not improve. As a result, the patient underwent right lower extremity above-knee amputation. After amputation, the patient's hemoglobin level improved significantly without blood transfusion, and she was discharged from the hospital after the incision healed. Postoperative pathological examination suggested neurogenic tumors. No other complications had occurred 1-year follow-up.
Vascular malformation and rupture are fatal complications of NF-1. Embolization may not provide complete relief, the patient might need to undergo neurofibroma resection or amputation.
Core Tip: We present the case of a 47-year-old female with neurofibromatosis type 1 with a rupture of right lower limb arterial malformation. She presented with sudden right lower limb swelling for two hours and symptoms of hemorrhagic shock on admission. Computed tomography angiography showed right lower limb arteriovenous malformation, and the patient underwent emergency vascular embolization. However, the patient did not experience any improvement in hemorrhagic shock symptoms. As a result, the patient underwent right lower extremity above-knee amputation. After amputation, the patient's hemoglobin level improved significantly without blood transfusion, and she was discharged from the hospital after the incision healed.
- Citation: Shen LP, Jin G, Zhu RT, Jiang HT. Hemorrhagic shock due to ruptured lower limb vascular malformation in a neurofibromatosis type 1 patient: A case report. World J Clin Cases 2022; 10(31): 11597-11606
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11597.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11597
Neurofibromatosis type 1 (NF-1) is a multisystem, autosomal dominant disorder of the peripheral nerves affecting nearly 1 in 3000 individuals worldwide[1]. There are a variety of features that characterize NF-1, including neurofibromas, café-au-lait spots, axillary and inguinal freckling, and pigmented hamartomas in the iris (Lisch nodules), which represent some of the diagnostic criteria for this disease[2-5]. Most often, NF-1 is associated with vascular abnormalities in medium to large arteries, such as aneurysms and stenoses of the aorta, renal arteries, and mesenteric arteries[6]. The majority of vascular lesions occur in people over 50 years[7]. Vascular changes are associated with fibromuscular dysplasia, thickening of the tunica intima of vessel walls, and degeneration of smooth muscle tissue[8]. Progression of these abnormalities can cause spontaneous arterial rupture, which has the potential to be fatal.
In the present report, we describe a case of NF-1 presenting with hemorrhagic shock due to spontaneous rupture of vascular abnormalities in the right lower limb. The patient eventually underwent right lower extremity amputation after failure of vascular embolization.
A 41-year-old woman with NF-1 was admitted to the Emergency Department with hemorrhagic shock and a large lump in the right lower limb.
Without incentive, the patient suddenly felt swelling in the right lower limb, which was accompanied by pain 2 h later. When the patient was taken to the emergency room, her blood pressure at admission was 86/51 mmHg, her heart rate was 115 bpm, and her oxygen saturation was 92%. The patient was conscious, indifferent, and answered clearly.
The patient complained of a lump on the right lower limb for 5 years, with symptoms worsening for 2 years. She said a chestnut-sized lump appeared on the front of her right calf 5 years prior, and the lump gradually increased in size. The patient was ambulatory, but there was occasional swelling and pain. At the same time, a dark-brown coloration appeared on the skin of the right lower limb, perineal region, buttocks, waist, and abdomen. Then, after accidentally falling on the right lower limb two years before the current incident, she noticed that the lump began to grow rapidly, eventually presenting as elephantiasis. Beginning the same year, the patient was no longer ambulatory and experienced intensifying nocturnal pain.
The family history revealed that the maternal grandmother, mother, two maternal uncles, a sister and a brother were diagnosed with NF-1.
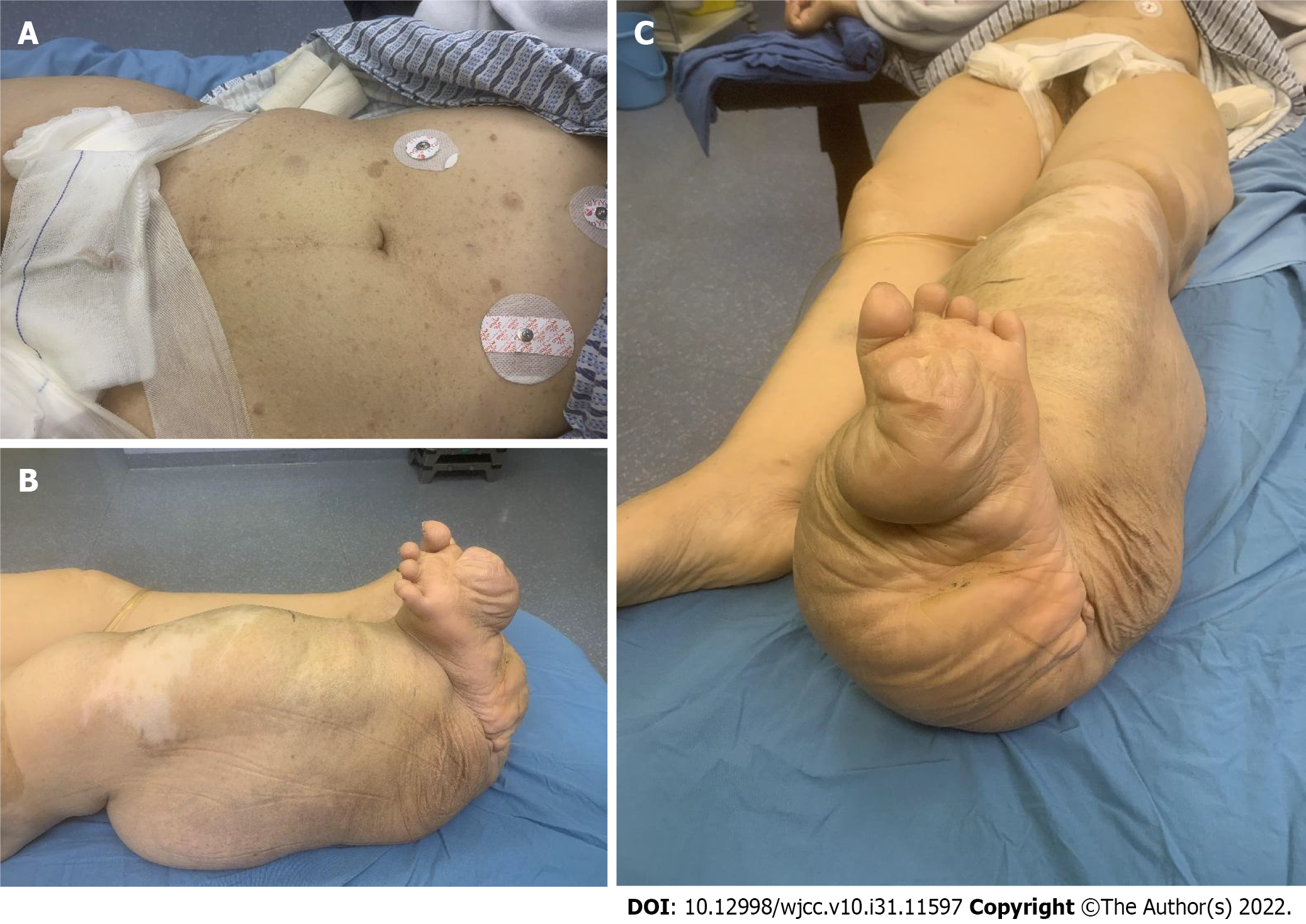
The physical examination upon admission revealed the following: Visible dark-brown pigmentation over a large area (Figure 1A); bilateral congenital talipes equinovarus and right lower limb presenting as elephantiasis (Figure 1B). The patient had almost lost range of motion in the right knee and ankle. The longest trail of the lump was 77 cm, and the largest circumference was 50 cm (Figure 1C). The rest of the limbs were basically normal.
At admission, laboratory investigation showed that the patient had moderate anemia (hemoglobin 66 g/L), with normal coagulation, hepatic and renal functions.
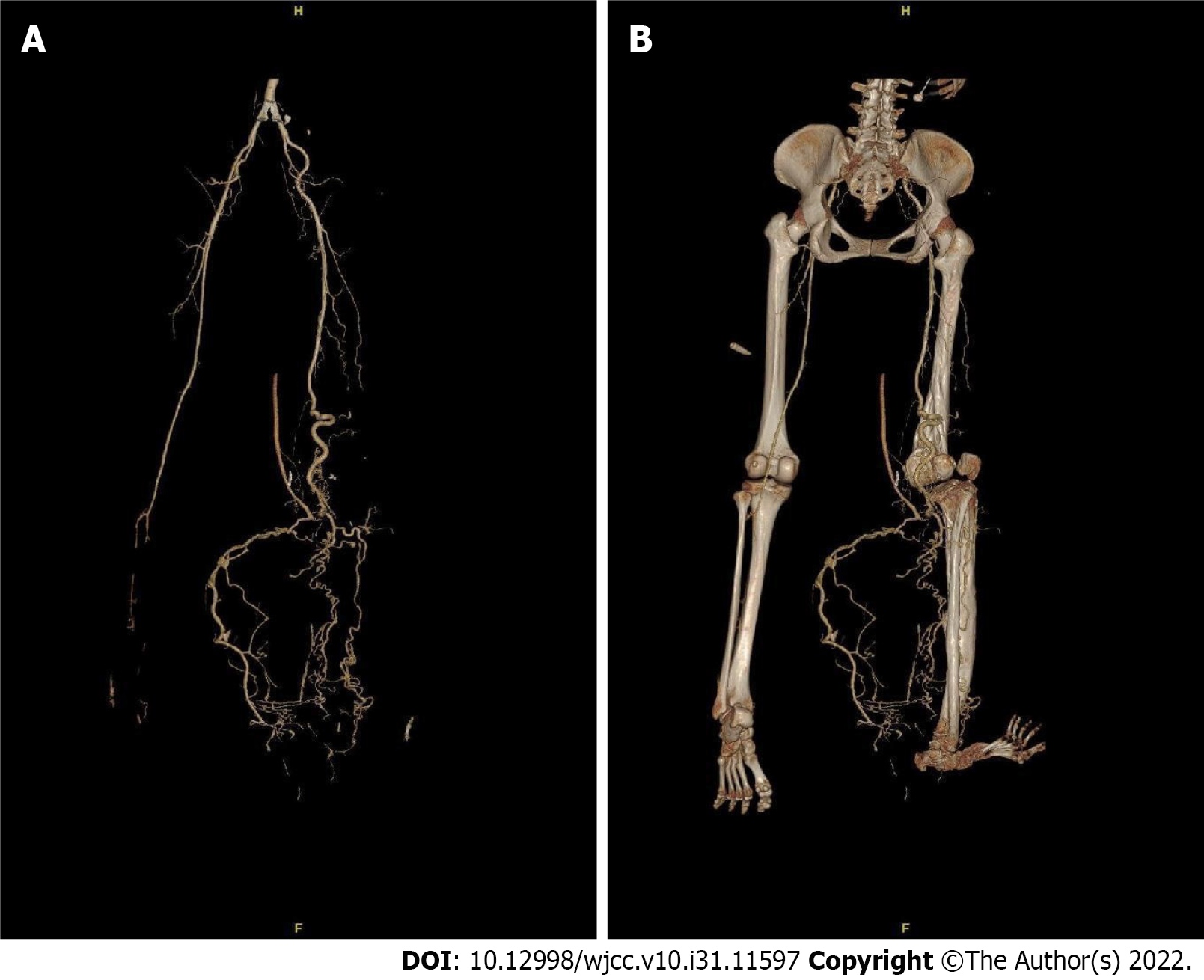
The X-ray examination revealed soft tissue and skeletal changes in the right lower extremity with growth disturbance at the distal femur, degenerative changes in the right knee joint (Figure 2A and B), and bone morphological changes in the lower segment of the right tibia (Figure 2C and D). Emergency color Doppler ultrasonography showed the following: (1) No obvious abnormalities of the liver, gallbladder, spleen, pancreas, kidneys, ureter, bladder, or perineum; (2) Multiple, nonuniform echo lumps on the front of the right calf; and (3) Extensive mixed echoes and flocculent echoes in the subcutaneous area in the right lower limb, with unclear boundaries and no obvious blood flow signal. Regrettably, bedside emergency ultrasound imaging was of poor quality, and images were not preserved. We believed the cause of the patient’s hemorrhagic shock was active bleeding in the right lower limb. After anti-shock therapy, the patient underwent emergency computed tomographic angiography (CTA) examination.
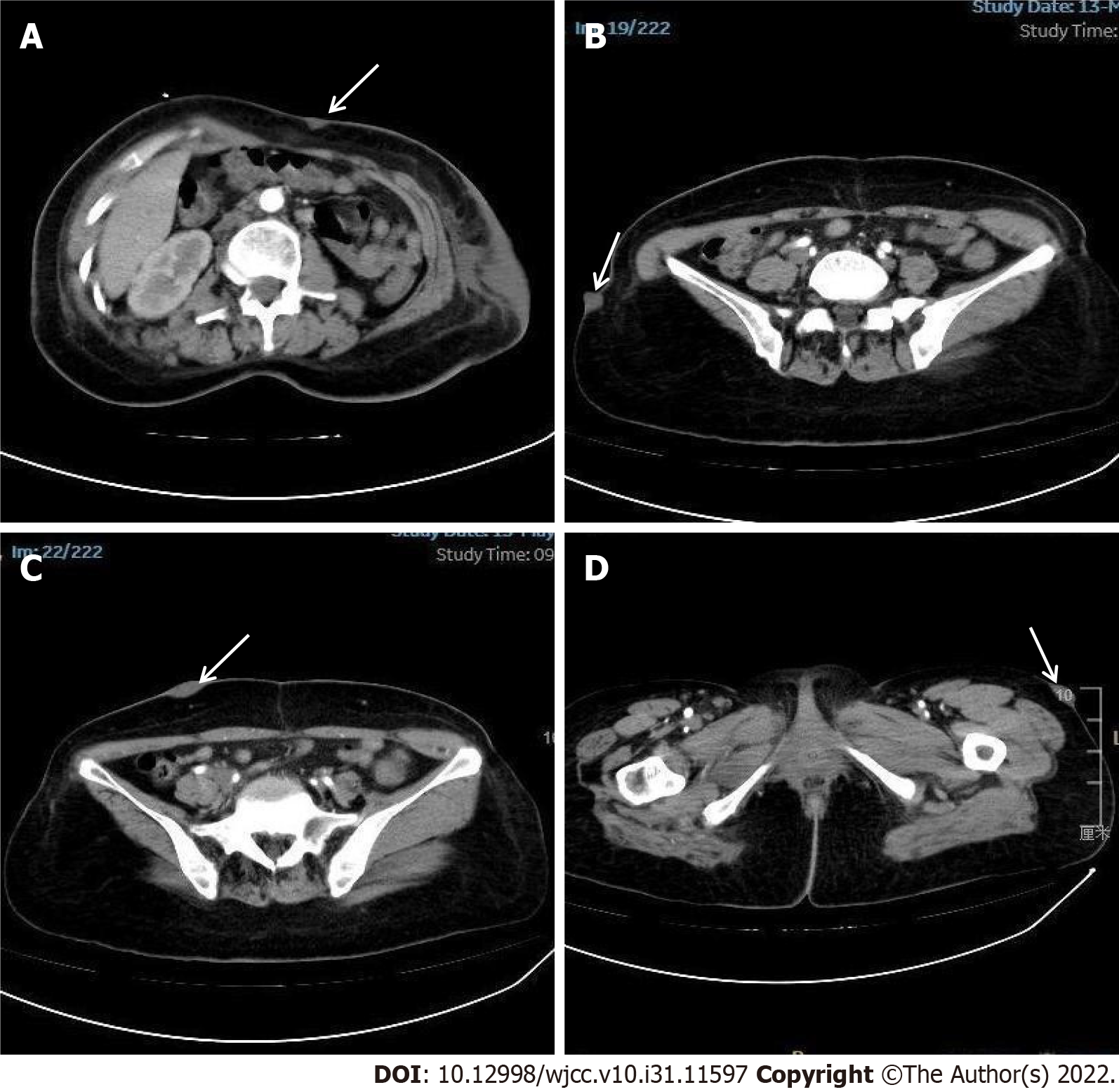
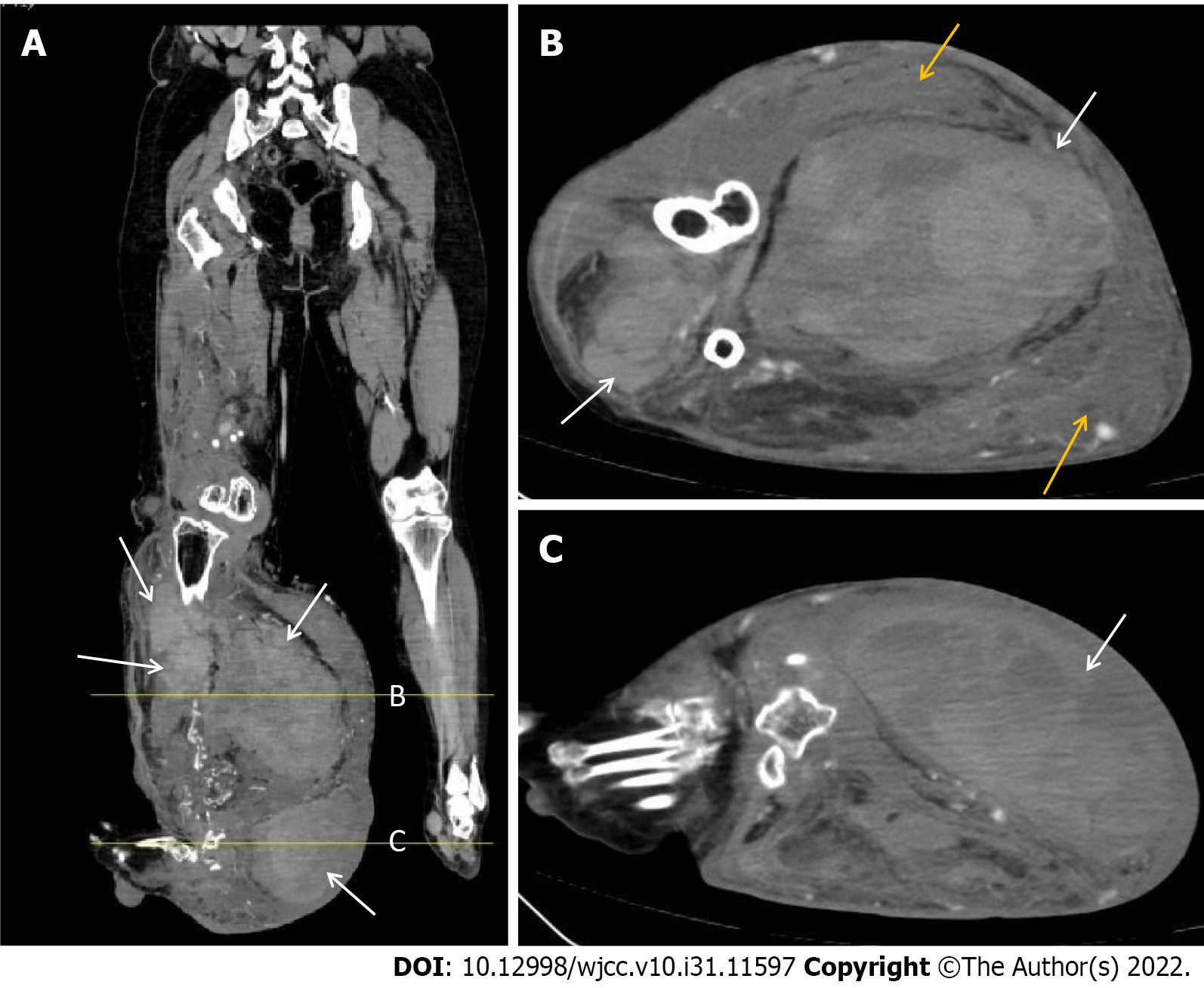
CTA examination showed that the right popliteal and posterior tibial arteries were thickened and tortuous, that multiple collateral small blood vessels were formed, and that the superficial veins of the right calf were increased and thickened (Figure 3). Multiple mixed high-density shadows (CT value approximately 23-58 Hu) were seen in the distal right thigh, right knee joint and right calf muscle space. No obvious abnormality was found in the left lower extremity blood vessels. 3D reconstruction of the right lower extremity skeleton revealed skeletal changes in the right lower extremity with growth disturbance and right knee subluxation (Figure 3B). The soft tissue window showed the following: (1) Multiple nodules on the epidermis of the abdomen growing inward and outward (white arrow, Figure 4); (2) Multiple large masses in the front and back of the right calf (white arrow, Figure 5); and (3) A subcutaneous hematoma behind the right calf (yellow arrow, Figure 5).
The patient was diagnosed with NF-1 with a giant neurofibroma on the right lower limb. At the same time, the hemorrhagic shock was secondary to rupture and hemorrhage of vascular malformation in the right lower limb neurofibroma.
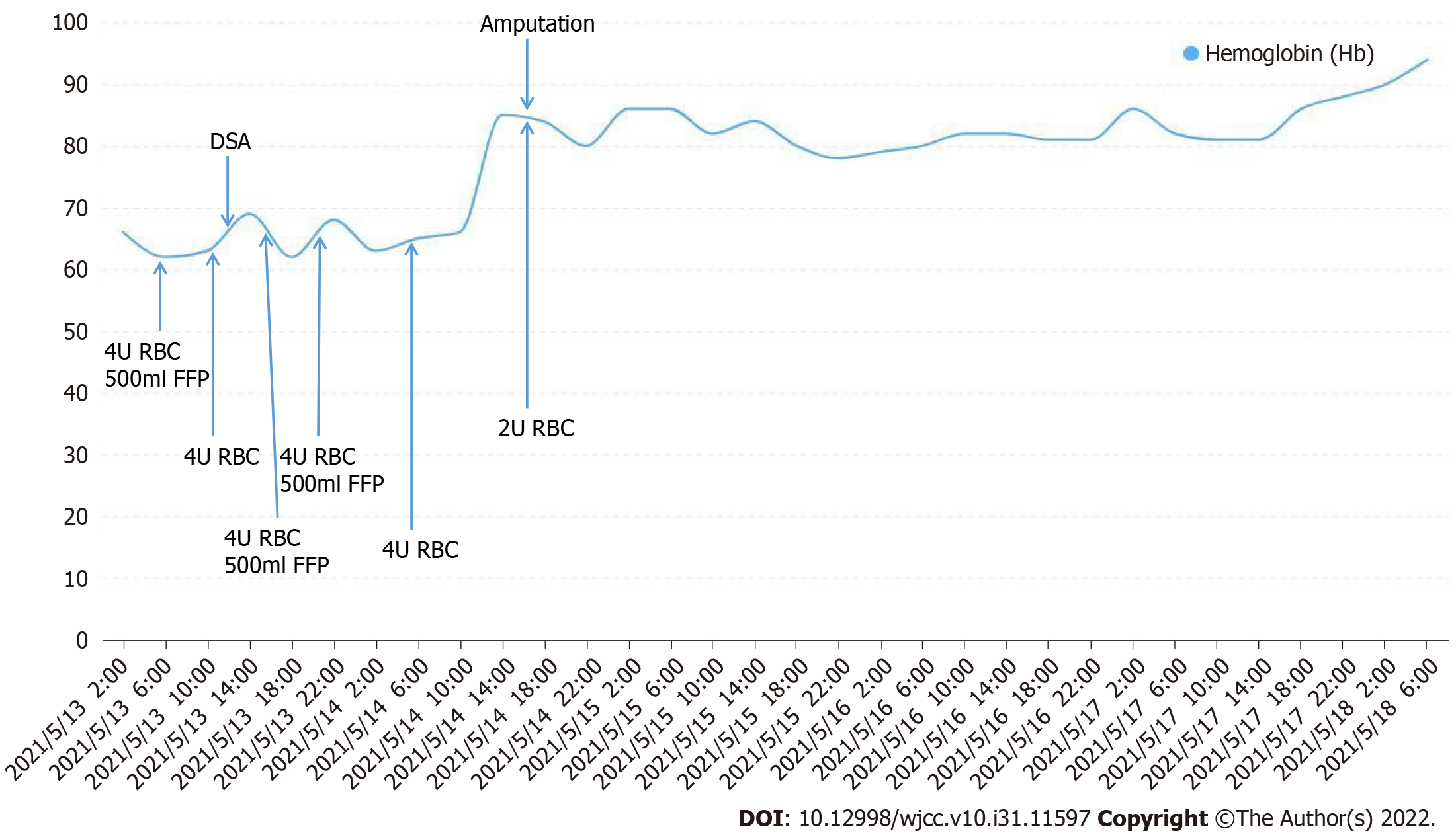
To treat hemorrhagic shock and increase blood volume, the patient was admitted to the emergency intensive care unit after a transfusion of 4 units of red blood cells (RBCs) and 500 mL of fresh frozen plasma (FFP). Routine blood examination after blood transfusion showed that the hemoglobin level continued to drop (hemoglobin 62 g/L). This indicated that the patient had active bleeding in the right lower limb. Therefore, the patient underwent emergency right lower limb digital subtraction angiography (DSA) and vascular embolization after reinfusion of 4 units of RBCs.
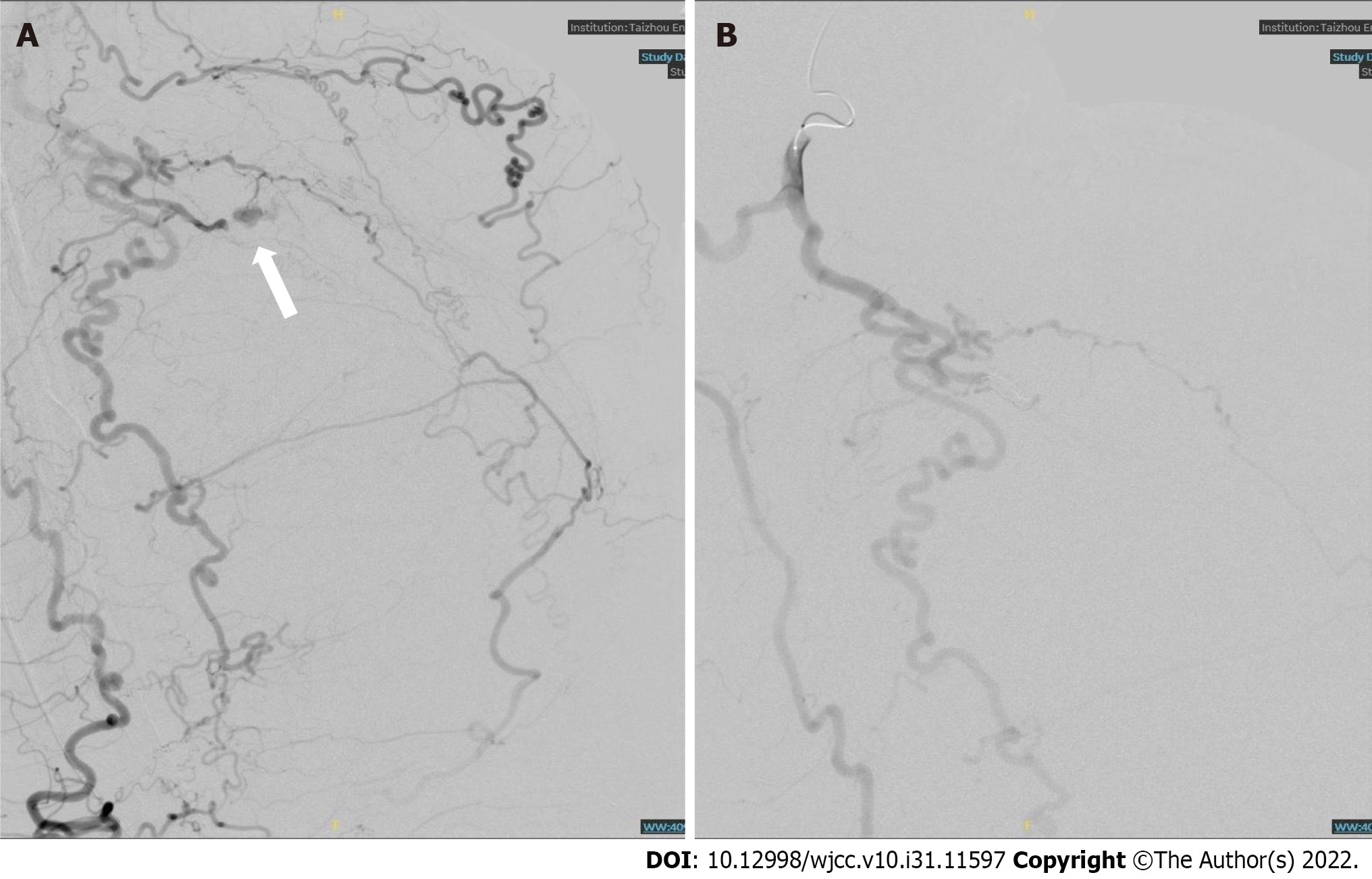
DSA showed that the right popliteal and tibiofibular arteries were tortuous, and disordered tumor-like blood vessels were seen (Figure 6A). Contrast medium extravasation was seen in the local arterial branches in the right calf (Figure 6A, white arrow). During vascular embolization, 3 coils of 3 mm × 140 mm and 1 coil of 4 mm × 140 mm were used, and no contrast medium extravasation was found in the second angiography (Figure 6B).
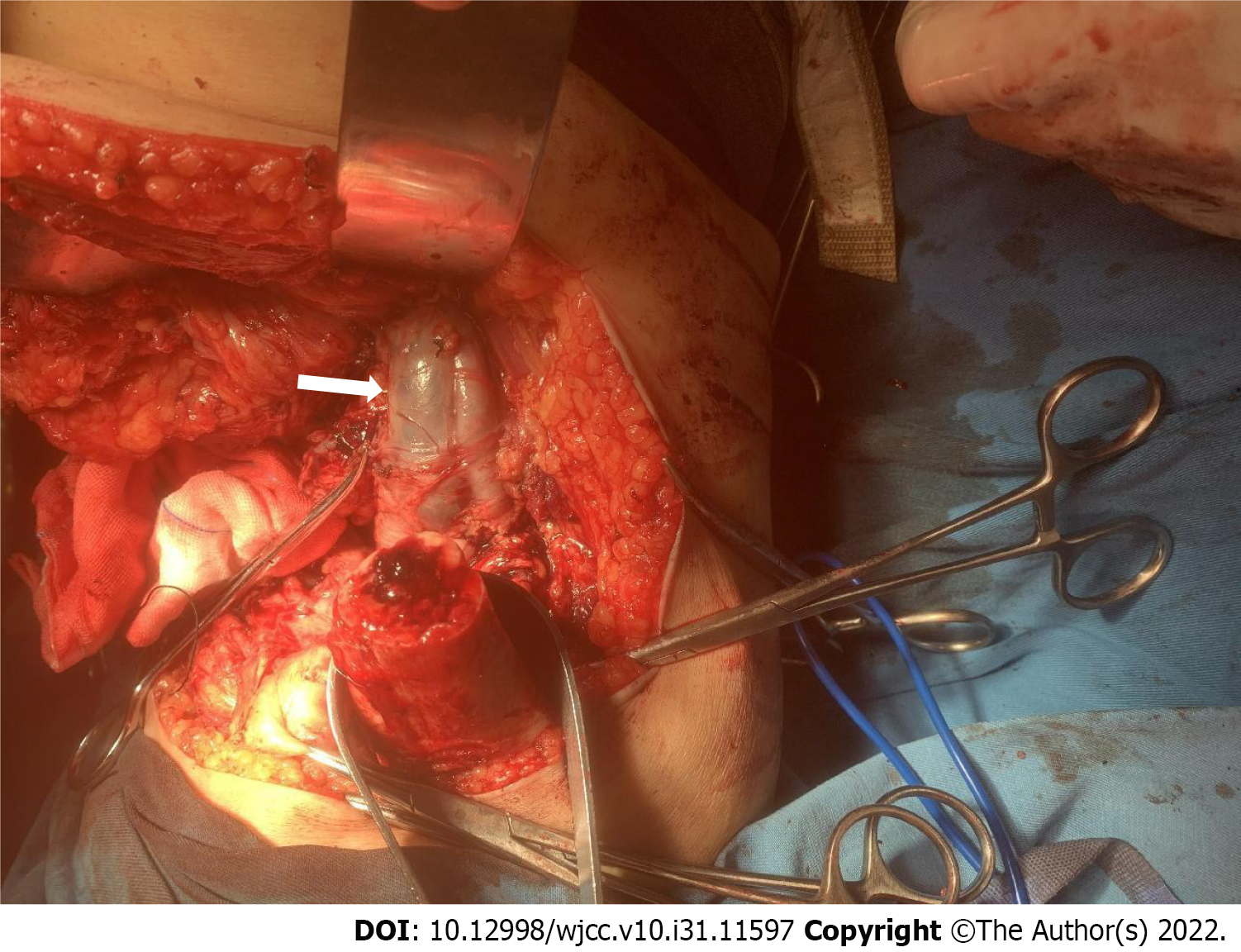
After DSA and vascular embolization, the patient received repeated blood transfusions (total 20 units RBCs and 1000 mL FFP before amputation), but the anemia and right lower limb swelling and tenderness did not improve. After a multidisciplinary consultation, it was believed that the patient still had active bleeding in the right lower limb. Eventually, the patient underwent a right lower limb above-knee amputation. During the operation, the femoral artery and vein were obviously thickened and tortuous (Figure 7). After intraoperative transfusion of 2 units of RBCs, routine blood tests showed a hemoglobin level of 85 g/L 2 h after the operation. After that, the patient's hemoglobin levels gradually recovered without further blood transfusion. All treatment measures administered for the patient as well as hemoglobin trends are shown in Figure 8.
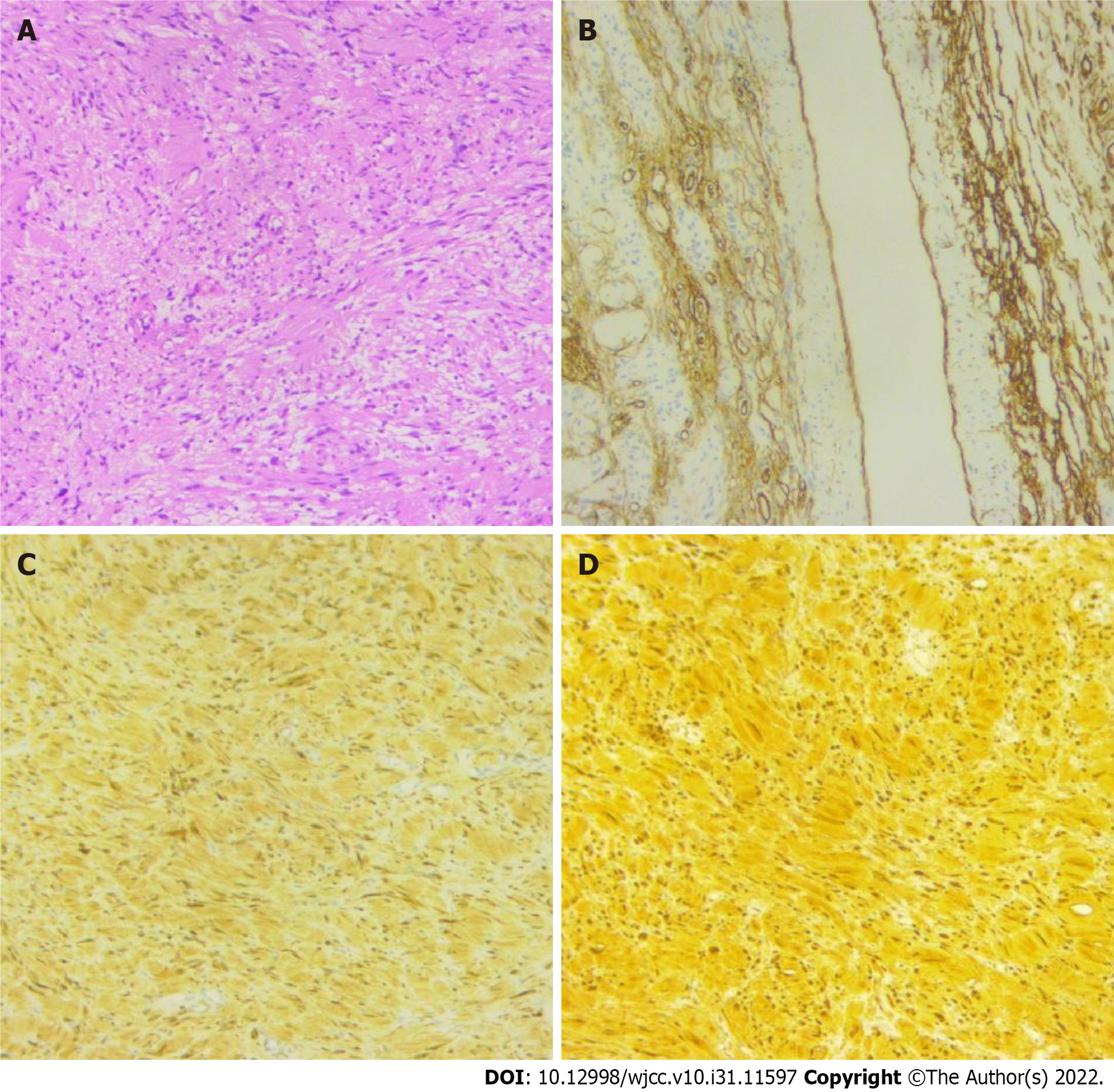
One week after the operation, the incision of the patient's right lower extremity had healed well, and routine blood examination showed that the hemoglobin level was 95 g/L. Postoperative pathological examination revealed neurogenic tumors (Figure 9). At the 1-year follow-up, the incision had healed, and no other complications had occurred.
We hereby report a rare case of hemorrhagic shock caused by ruptured right lower limb vascular malformation in a patient with NF-1. The patient had a giant neurofibroma of the right lower limb that caused vascular malformation. Neurofibromas are benign tumors that occur alone or in multiple forms and often present with slow-growing painless nodules or lumps[1]. The disease is called NF when the nodules spread throughout the body[9]. The National Institutes of Health Consensus Development Conference criteria for the diagnosis of NF-1 are satisfied in an individual if 2 or more of the following signs are found: Six or more café-au-lait spots with the greatest diameter larger than 5 mm in pre
Vascular complications in patients with NF-1, although rare, can be fatal when they occur. Vascular lesions usually occur in medium or large arteries, and aneurysms, stenosis and arterial malformations are common manifestations. Spontaneous arterial rupture associated with NF-1 has been described in nearly all medium to large arteries, including the aorta and the subclavian, mesenteric, and vertebral arteries[10,11]. Vascular lesions of the brain, endocrine system, gastrointestinal tract, and heart have also been reported[12]. However, arterial rupture and hemorrhage caused by lower limb arterial malformations have rarely been reported. In general, patients with vascular malformations should be considered for the presence of pseudoaneurysms. A previous study showed that ultrasound examination is crucial in evaluating such patients because it provides diagnostic findings of pseudoaneurysms[13]. In this report, we described a middle-aged NF-1 patient with hemorrhagic shock and a large neurofibroma in the right lower limb. Although pseudoaneurysms were ruled out by ultrasonography, bedside emer
Treatment options for artery rupture include resection of the artery with ligation or endovascular therapy. Treatment is dependent on the patient’s age, as well as the type and location of the lesion. In our case, the patient had symptoms of hemorrhagic shock on admission, and treatment for hemostasis was required immediately. Previous studies have suggested that the less invasive endovascular approach might be preferable for treating NF-1-related vascular rupture. NF-1-related vasculopathy lesion sites are diverse, and intraoperative angiography would help confirm the diagnosis[15]. Therefore, we chose to perform vascular embolization on the patient. However, although the bleeding point disappeared during the operation, the patient's symptoms of anemia and hemorrhagic shock did not improve after surgery, and blood transfusion therapy was also ineffective. This might be because neurofibroma tissue contains many blood sinuses with thin and poorly contractible sinus cavities[16].
After failure of arterial embolization, we also excluded arterial ligation and removal of lumps containing arterial malformations as options. Because the patient's lower extremity arterial malformation range was large, it was very difficult to find the bleeding point through incision, and it was almost impossible to complete. In addition, resection of solitary neurofibromas containing arterial malformations has been shown to fail. In 2012, Zhou et al[14] reported a giant neurofibroma in the right lower limb of a young NF-1 patient. In their report, the patient underwent neurofibroma resection first but presented with uncontrollable infection and finally had to undergo amputation to ensure survival. Therefore, we ended up opting for above-knee amputation. During amputation surgery, sufficient blood should be available. In our report, we observed that the femoral artery and vein were tortuous and thickened, and there was more blood oozing in the muscle space. Although 20 units of RBCs were transfused before amputation, 2 units of RBCs were transfused again during the operation.
Vascular malformation and rupture are fatal complications of NF-1. Although previous reports have described that arterial embolization can achieve good clinical results, in ruptured arteries inside giant neurofibromas, vascular embolization may not provide complete relief and may prolong the patient's condition. For limb dysfunction caused by giant neurofibromas of the lower limb with or without arterial hemorrhage, amputation appears to be the best option.
| 1. | Fukushima N, Aoki H, Takenaga S, Morikawa K, Ogawa M, Yanaga K. Ruptured visceral artery aneurysms in a patient of neurofibromatosis type 1 (NF-1) successfully treated by endovascular treatment. Surg Case Rep. 2020;6:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Antônio JR, Goloni-Bertollo EM, Trídico LA. Neurofibromatosis: chronological history and current issues. An Bras Dermatol. 2013;88:329-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Riccardi VM. Von Recklinghausen neurofibromatosis. N Engl J Med. 1981;305:1617-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 836] [Cited by in RCA: 737] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 4. | Zamora AC, Collard HR, Wolters PJ, Webb WR, King TE. Neurofibromatosis-associated lung disease: a case series and literature review. Eur Respir J. 2007;29:210-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 85] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Ueda K, Honda O, Satoh Y, Kawai M, Gyobu T, Kanazawa T, Hidaka S, Yanagawa M, Sumikawa H, Tomiyama N. Computed tomography (CT) findings in 88 neurofibromatosis 1 (NF1) patients: Prevalence rates and correlations of thoracic findings. Eur J Radiol. 2015;84:1191-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Oderich GS, Sullivan TM, Bower TC, Gloviczki P, Miller DV, Babovic-Vuksanovic D, Macedo TA, Stanson A. Vascular abnormalities in patients with neurofibromatosis syndrome type I: clinical spectrum, management, and results. J Vasc Surg. 2007;46:475-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 275] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 7. | Falcone JL, Go MR, Baril DT, Oakley GJ, Makaroun MS, Chaer RA. Vascular wall invasion in neurofibromatosis-induced aortic rupture. Vasc Endovascular Surg. 2010;44:52-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Makino K, Kurita N, Kanai M, Kirita M. Spontaneous rupture of a dissecting aneurysm in the superior rectal artery of a patient with neurofibromatosis type 1: a case report. J Med Case Rep. 2013;7:249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Sehgal VN, Sharma S, Oberai R. Evaluation of plexiform neurofibroma in neurofibromatosis type 1 in 18 family members of 3 generations: ultrasonography and magnetic resonance imaging a diagnostic supplement. Int J Dermatol. 2009;48:275-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Greene JF Jr, Fitzwater JE, Burgess J. Arterial lesions associated with neurofibromatosis. Am J Clin Pathol. 1974;62:481-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 197] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Lehrnbecher T, Gassel AM, Rauh V, Kirchner T, Huppertz HI. Neurofibromatosis presenting as a severe systemic vasculopathy. Eur J Pediatr. 1994;153:107-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Hamilton SJ, Friedman JM. Insights into the pathogenesis of neurofibromatosis 1 vasculopathy. Clin Genet. 2000;58:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 183] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 13. | Corvino A, Catalano O, de Magistris G, Corvino F, Giurazza F, Raffaella N, Vallone G. Usefulness of doppler techniques in the diagnosis of peripheral iatrogenic pseudoaneurysms secondary to minimally invasive interventional and surgical procedures: imaging findings and diagnostic performance study. J Ultrasound. 2020;23:563-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Zhou J, Li M, Luo C, He Q, Yin Z, Peng H, Chen Z, Chen J, Zhong S, Huiqing X. Giant neurofibroma in the right lower limb of a 26-year-old woman: report of a case. Int Surg. 2012;97:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Matsuura S, Hashimoto T, Suhara M, Deguchi J. Ruptured tibial artery in neurofibromatosis type 1: A case report. Int J Surg Case Rep. 2021;83:106012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 16. | Fernandez-Delgado J, Rodriguez-Merchan EC, Martinez-Mendez JR. First giant gluteal neurofibroma reported in the literature in a person with haemophilia and its high risk of massive bleeding to death. Haemophilia. 2005;11:419-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corvino A, Italy;