Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11549
Peer-review started: June 22, 2022
First decision: August 4, 2022
Revised: August 8, 2022
Accepted: October 9, 2022
Article in press: October 9, 2022
Published online: November 6, 2022
Processing time: 126 Days and 16.5 Hours
Ganglioneuromas are rare tumors of the sympathetic nervous system that ori
A 34-year-old male presented with a 4-month history of progressive paralysis of both upper limbs along with an unsteady gait. The touch sensitivity of both hands was reduced, and there was conspicuously high muscle tonus in his upper and lower limbs, along with hyperactive physiological reflection and deep reflexes. Magnetic resonance imaging showed several nodules around the C2-7 intervertebral foramena, among which the masses lying between C1 and C2 were obviously bilaterally compressing the spinal cord. Successful posterior decom
Multiple and bilateral ganglioneuroams are a rare occurrence in the cervical spine. In this case report, timely resection of the neoplasms around C1 and C2 resulted in spinal cord decompression, with rapid relief of symptoms and a good pro
Core Tip: Ganglioneuromas is common benign tumor but uncommonly existing in the upper cervical spine. Meanwhile, this kind of tumor is rare to be multiple or bilateral. We present a 34-year-old male with the 4 mo history of paralysis in upper limbs and unsteady gait. The magnetic resonance imaging showed bilateral nodes from C2 to C7 intervertebral foramens, among which the bulks between C1 and C2 compressed the spinal cord obviously. The operation of posterior decompression was performed successfully without fixation and the tumors was removed integrally. The pathological diagnosis was ganglioneuromas. Including the current case, we are aware of only seven such cases in the literature, of which four arose from Japan, one from China, and one from Spain. We suppose that ethnicity and geographic associations with this rare disease presentation may be an aspect for future consideration and investigation.
- Citation: Wang S, Ma JX, Zheng L, Sun ST, Xiang LB, Chen Y. Multiple bilateral and symmetric C1-2 ganglioneuromas: A case report. World J Clin Cases 2022; 10(31): 11549-11554
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11549.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11549
Ganglioneuroma (GN) is a type of benign tumor composed of mature ganglion and nerve sheath cells, which generally arises in association with sympathetic nerves or sympathetic nervous tissue[1]. Very rarely, the neoplasm occurs bilaterally in the upper cervical spine, presenting as a dumb-bell shaped mass surrounding the spinal cord. In these circumstances, the spinal cord is potentially compressed by the neoplasm, resulting in symptoms of limb numbness and weakness, potentially progressing to paralysis and respiratory failure[2]. Surgical resection is required to relieve the symptoms and recover limb function.
Here, we present a rare case of bilateral and symmetric dumb-bell ganglioneuromas in the region of C1-2. We discuss this case in the context of only six previously reported cases of ganglioneuroma affecting the upper cervical spine bilaterally.
The patient provided written informed consent for this case study. A 34-year-old male presented with a history of paralysis in both upper limbs and unsteady gait in the last 4 mo.
The symptoms had progressed rapidly in severity in the past 1 mo preceding his hospital visit.
The symptoms had progressed rapidly in severity in the past 1 mo preceding his hospital visit.
The patient was an index case of his family about the history of neurofibromatosis.
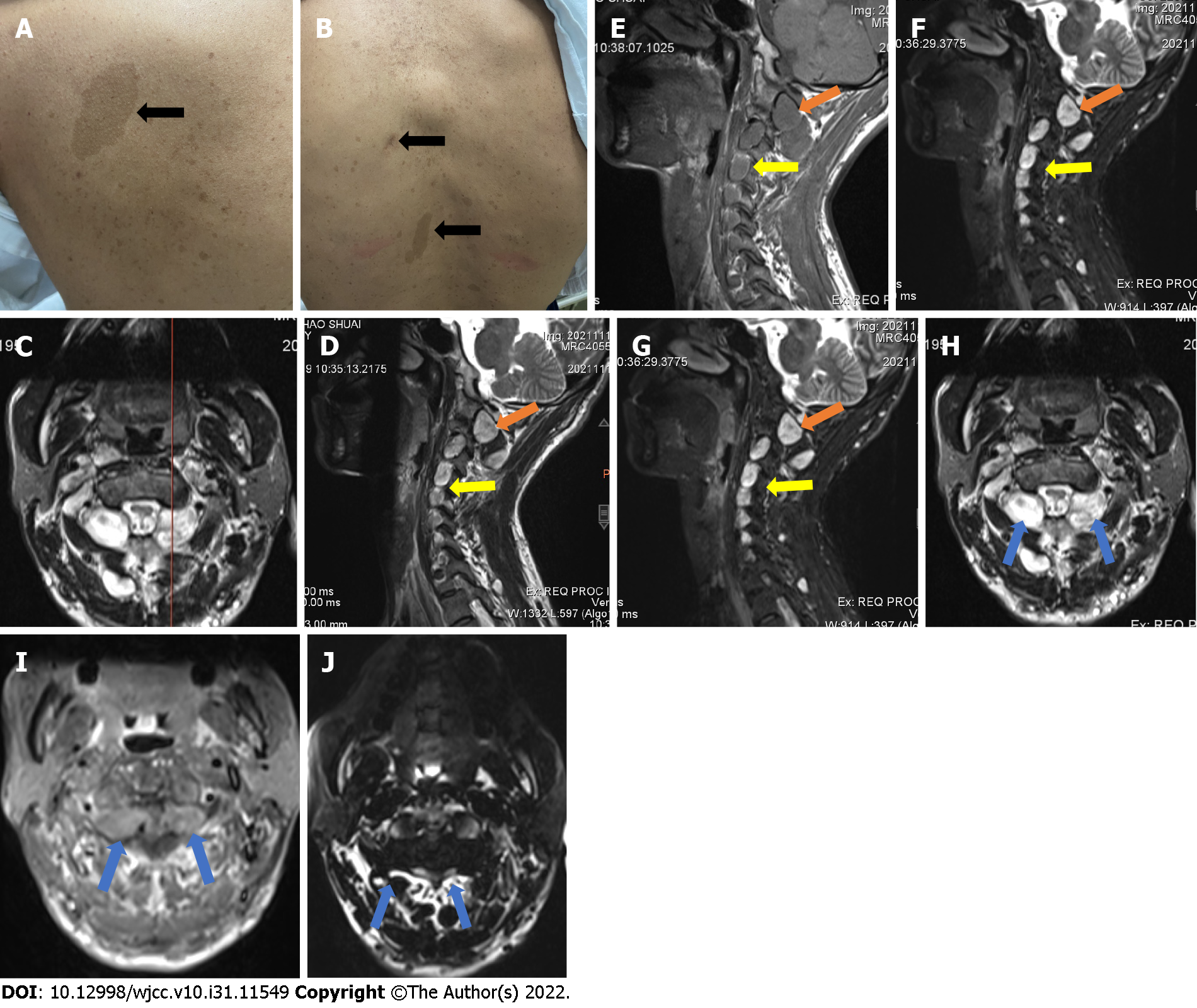
He presented with multiple cafe-au-lait spots on his body (Figure 1A). The vibrotactile sensitivities of both hands were reduced, which indicating that the spinal cord was affected, and the limb strength was normal. Since there was not numbness or pain in specific area of the limbs, we inferred that none of the exact nerve root was oppressed heavily. Muscle tonus was notably elevated in the upper and lower limbs, the muscular tension of the upper and lower limbs was high, and he showed hyperactive deep tendon reflexes. Additionally, his examination shows positive Hoffman and Babinski signs.
None important laboratory examinations were referred for this case.
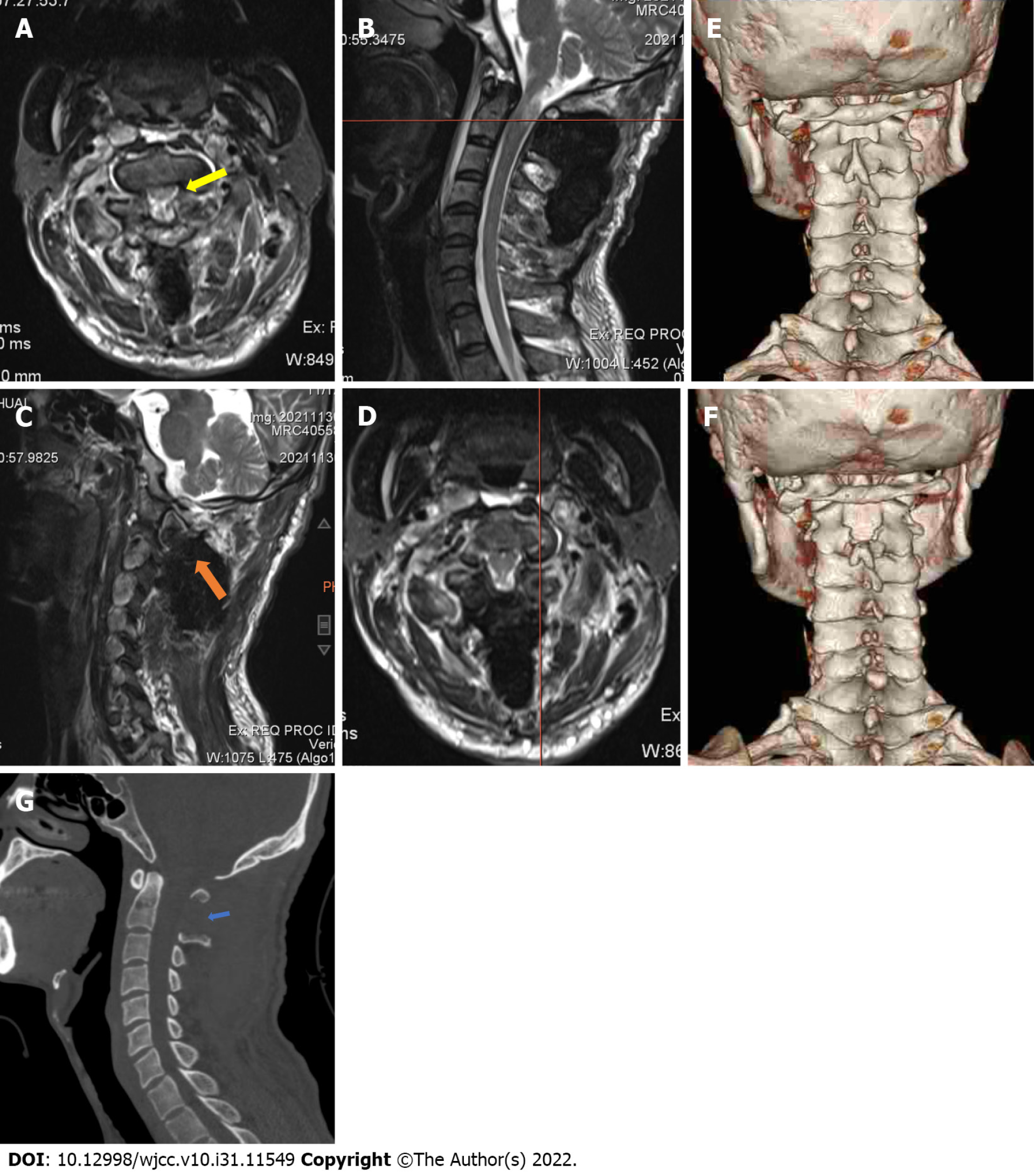
Magnetic resonance imaging (MRI) of the cervical spine revealed several nodules around the C2-7 intervertebral foramens (Figure 1B). Each nodule presented with low signal intensity on T1-weighted images, but with high intensity on T2-weighted and enhanced images. Among the masses, the nodes around C1 and C2 were clearly compressing the spinal cord bilaterally (Figure 1C). The dimension of the lesion in the right side was 17.1 mm × 22.5 mm × 16.8 mm and the dimension of the lesion in the left side was 16.9 mm × 19.8 mm × 17.2 mm. The nodules of both sides between C1 and C2 were removed entirely after the operation and the compression of the spinal cord was relieved thoroughly (Figure 2).
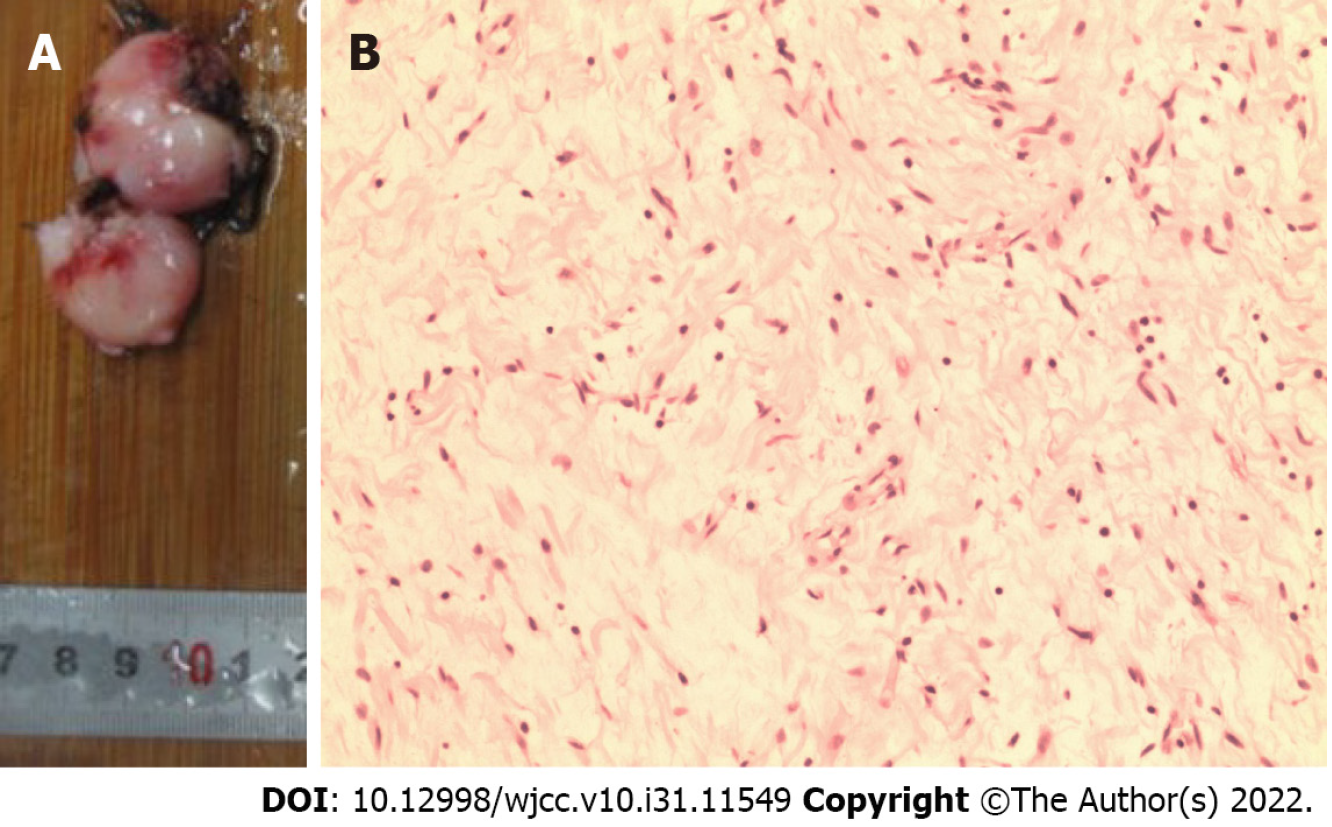
Histological examination confirmed diagnosis of ganglioneuroma (Figure 3).
The operation was performed under general anesthesia with endotracheal intubation, with the patient kept in a prone position. A standard posterior midline surgical approach was performed. The laminae of C2 and C1 were partly resected to expose the tumors thoroughly, whereupon they were excision with margins entirely. After excision of the neoplasm, the compression of the spinal cord was immediately relieved.
At the 3-mo follow-up, the patient’s symptoms had completely resolved.
Ganglioneuromas are usually benign, slow-growing tumors that arise or differentiate from neu
In the current case, the patient had multiple ganglioneuromas bilaterally affecting all cervical nerves from C2 to C7. Also, the café-au-lait marks and history of resection of a neurofibromatosis have previously been associated with ganglioneuromas[4]. In our case, most neoplasms of these nodes were asymptomatic, since there was sufficient space for expansion of the tumors. However, the massive bulks in the upper cervical spine caused severe compression to the spinal cord, resulting in serious sensorimotor symptoms. The spine marrow of this region is important not only to the sensory and motor functions of the limbs but also for controlling the respiratory system, which calls for timely relief of compression. Since ganglioneuromas are often solid and have distinct boundaries between surrounding structures, intact resection could be realized without difficulty, with preservation of the bony structures necessary for maintaining the stability of the spine.
To the best of our knowledge, there are only six previous case reports of bilateral and symmetric GNs in the region of upper cervical spine, so we believe it is important to present our case in the context of the limited literature. In 2001, Ugarriza et al[5] reported a case of bilateral and symmetric C1-2 dumbbell ganglioneuroma. Their patient presented with progressive weakness of the limbs, bladder and bowel incontinence, and respiratory difficulty. After an en bloc operative resection of the tumor, there was some persistence of limb weakness, but the respiratory problems disappeared completely. Similarly, Kyoshima et al[6] reported a 35-year-old patient with sensorimotor and respiratory dysfunctions. The tumors extended from C1-C3, consisting of four bilateral C2 and C3 root-related tumors. After expression, the tumors were resected at the dural side, with retention of intraforaminal and extradural parts. In the cases reported by Miyakoshi et al[2] and Ando et al[7], asymptomatic foraminal and extraforaminal tumors were found in conjunction with bilateral and symmetric C1-2 ganglioneuromas; in both cases, the treatment was removal of the tumors at C1-2. The case of Hioki et al[8], an elderly man (72 years) had progressive incomplete paraplegia and lightheadedness. The bilateral tumors at the C1-2 Level were removed thoroughly, followed by histopathological diagnosis of ganglioneuroma. In 2019, Tan et al[9] reported a 27-year-old man with gradually progressive right upper extremity weakness and numbness in both hands. After total resection of the tumor, the syndromes were relieved. Interestingly, four of these case reports arose from Japan, one from China, and one from Spain. We presume that ethnicity and geographic associations with this rare disease presentation may be an aspect for future consideration and investigation.
We present our case since multiple bilateral ganglioneuromas of the upper cervical spine are a rare occurrence, with scant documentation in the literature. Diagnosis and surgical planning were facile with MRI and computed tomography imaging. We note the need for timely surgery to decompress the spine by removing the bulk of the tumors, while preserving the bony structures required for spinal stabilization. Even in the case of a benign lesion, cord compressive symptoms would mandate surgical excision.
| 1. | Hussain MH, Iqbal Z, Mithani MS, Khan MN. Retroperitoneal Ganglioneuroma in a Patient Presenting With Vague Abdominal Pain. Cureus. 2020;12:e9133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Miyakoshi N, Hongo M, Kasukawa Y, Misawa A, Shimada Y. Bilateral and symmetric C1-C2 dumbbell ganglioneuromas associated with neurofibromatosis type 1 causing severe spinal cord compression. Spine J. 2010;10:e11-e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. Radiographics. 2002;22:911-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 458] [Cited by in RCA: 398] [Article Influence: 16.6] [Reference Citation Analysis (1)] |
| 4. | Bacci C, Sestini R, Ammannati F, Bianchini E, Palladino T, Carella M, Melchionda S, Zelante L, Papi L. Multiple spinal ganglioneuromas in a patient harboring a pathogenic NF1 mutation. Clin Genet. 2010;77:293-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Ugarriza LF, Cabezudo JM, Ramirez JM, Lorenzana LM, Porras LF. Bilateral and symmetric C1-C2 dumbbell ganglioneuromas producing severe spinal cord compression. Surg Neurol. 2001;55:228-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Kyoshima K, Sakai K, Kanaji M, Oikawa S, Kobayashi S, Sato A, Nakayama J. Symmetric dumbbell ganglioneuromas of bilateral C2 and C3 roots with intradural extension associated with von Recklinghausen's disease: case report. Surg Neurol. 2004;61:468-73; discussion 473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Ando K, Imagama S, Ito Z, Hirano K, Tauchi R, Muramoto A, Matsui H, Matsumoto T, Ishiguro N. Cervical myelopathy caused by bilateral C1-2 dumbbell ganglioneuromas and C2-3 and C3-4 neurofibromas associated with neurofibromatosis type 1. J Orthop Sci. 2014;19:676-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Hioki A, Miyamoto K, Hirose Y, Kito Y, Fushimi K, Shimizu K. Cervical symmetric dumbbell ganglioneuromas causing severe paresis. Asian Spine J. 2014;8:74-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Tan CY, Liu JW, Lin Y, Tie XX, Cheng P, Qi X, Gao Y, Guo ZZ. Bilateral and symmetric C1-C2 dumbbell ganglioneuromas associated with neurofibromatosis type 1: A case report. World J Clin Cases. 2019;7:109-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Govindarajan KK, India; Wang F S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ