Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.985
Peer-review started: November 14, 2020
First decision: July 16, 2021
Revised: July 26, 2021
Accepted: December 22, 2021
Article in press: December 22, 2021
Published online: January 21, 2022
Processing time: 426 Days and 21.4 Hours
Intravascular fasciitis (IVF) is a rare nodular fasciitis that often involves the layers and lumens of blood vessels; therefore, it is easily misdiagnosed as a malignant tumor with invasion into blood vessels.
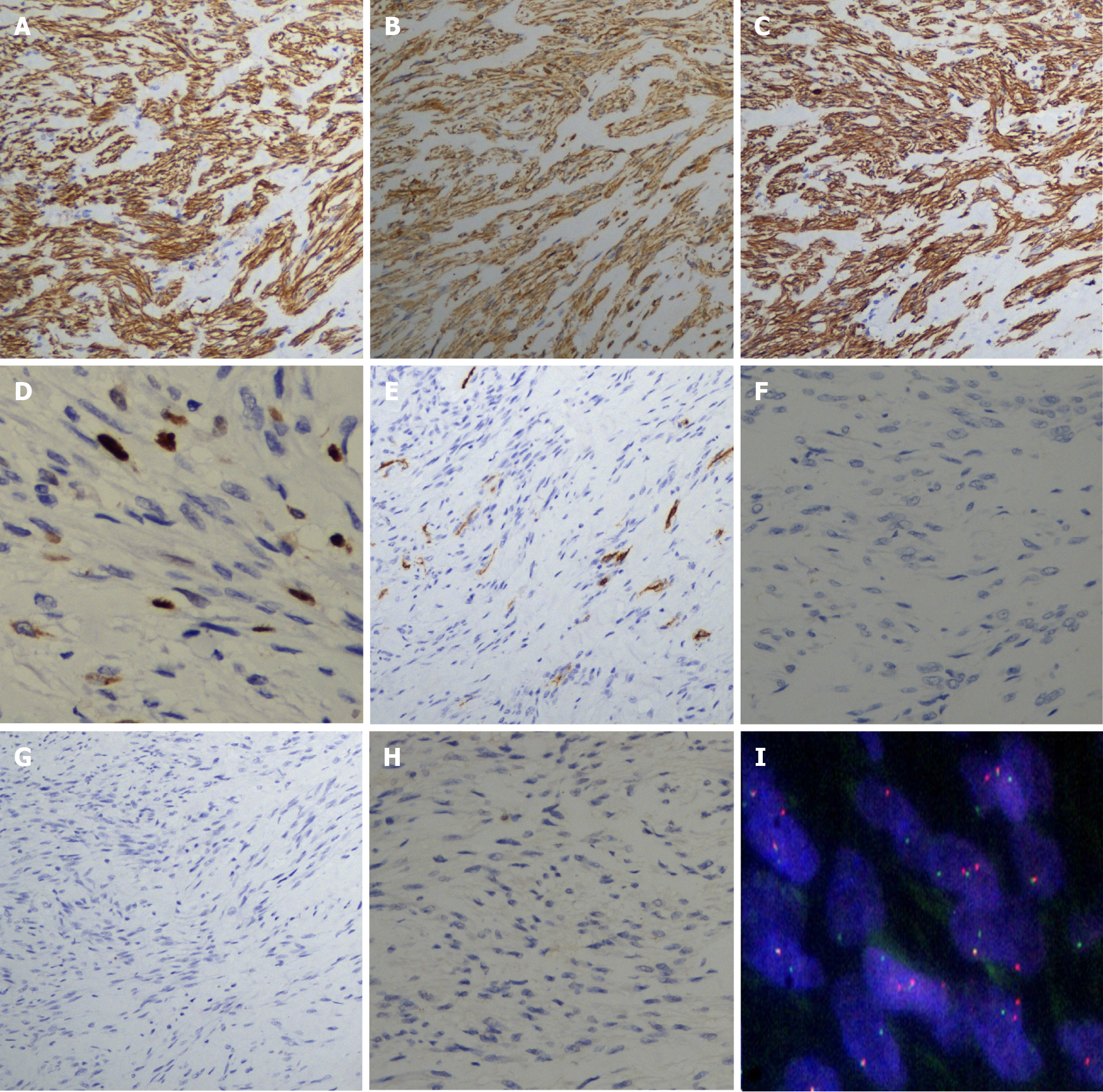
A 13-year-old boy was admitted due to a mass on the left side of his neck. Duplex ultrasonography revealed a circular solid hypoechoic mass in the external jugular vein, and magnetic resonance imaging revealed an enhanced longitudinal mass-like lesion in the left supraclavicular fossa. Surgical treatment was arranged and completed, histopathological analysis showed a large amount of spindle cell proliferation, and immunohistochemistry showed that the spindle cells were positive for the expression of vimentin, caldesmon, and smooth muscle actin and negative for the expression of S-100 protein, desmin, CD34, and c-kit; Ki-67 staining revealed a low proliferative index (5%-10%), which confirmed the differentiation characteristics of myofibroblasts. Fluorescence in situ hybridization detected the rearrangement of USP6. IVF was subsequently diagnosed.
IVF is characterized by intraluminal, intramural and extramural involvement of small to large arteries or veins. Unless the doctor has a deep understanding of the disease or suspects that there is an initial indicator, IVF may be confused with other intravascular malignancies, leading to unnecessary radical surgery. Imaging examination combined with histopathological examination can improve the diagnostic accuracy of this disease.
Core Tip: Intravascular fasciitis (IVF) is a rare vascular-associated nodular fasciitis that is easily misdiagnosed as other tumors. We report a case of this rare disease and provide insights on IVF, with the hope of improving the recognition of non-neoplastic lesions to avoid misdiagnosis.
- Citation: Meng XH, Liu YC, Xie LS, Huang CP, Xie XP, Fang X. Intravascular fasciitis involving the external jugular vein and subclavian vein: A case report . World J Clin Cases 2022; 10(3): 985-991
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/985.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.985
Intravascular fasciitis (IVF) was first proposed by Patchefsky et al[1] in 1981 as a special type of nodular fasciitis involving the small and medium veins or arteries. The disease is rare and rarely reported domestically or internationally. Intravascular fasciitis is a variant of nodular fasciitis, which is caused by the reactive intravascular proliferation of myofibroblasts. The histology of IVF is very similar to that of typical nodular fasciitis, but it often involves the layers and lumens of blood vessels, frequently leading to an overdiagnosis of vascularized malignancies[2,3]. IVF most commonly occurs in the upper extremities, head and neck, followed by the lower extremities and trunk, but there have been reports of rare sites, such as the mouth and maxillofacial region[4-7]. This study reports intravascular nodular fasciitis of the external jugular vein and subclavian vein and explores its clinical and pathological features, diagnosis and differential diagnosis combined with a literature review to raise awareness of rare lesions and avoid misdiagnosis.
A 13-year-old boy came to our clinic with his parents due to a mass on the left side of his neck for 1 mo.
One month prior to admission, the patient accidentally felt a mass on his left neck, approximately 2 cm × 2 cm in size, and there was no local discomfort such as redness, swelling and tenderness. After learning this, his parents brought him to the hospital for treatment.
The patient had been in good health until he showed evidence of the disease.
The patient was not from a consanguineous marriage and there was no family history of similar disease.
During the physical examination, a clear soft tissue mass was palpated on the left supraclavicular area and was determined to be an ovoid-shaped mass of approximately 2 cm × 2 cm in size.
The results of laboratory examinations on admission were normal, including routine blood and coagulation function tests, liver and kidney function tests, tumor markers, urine tests and stool tests.
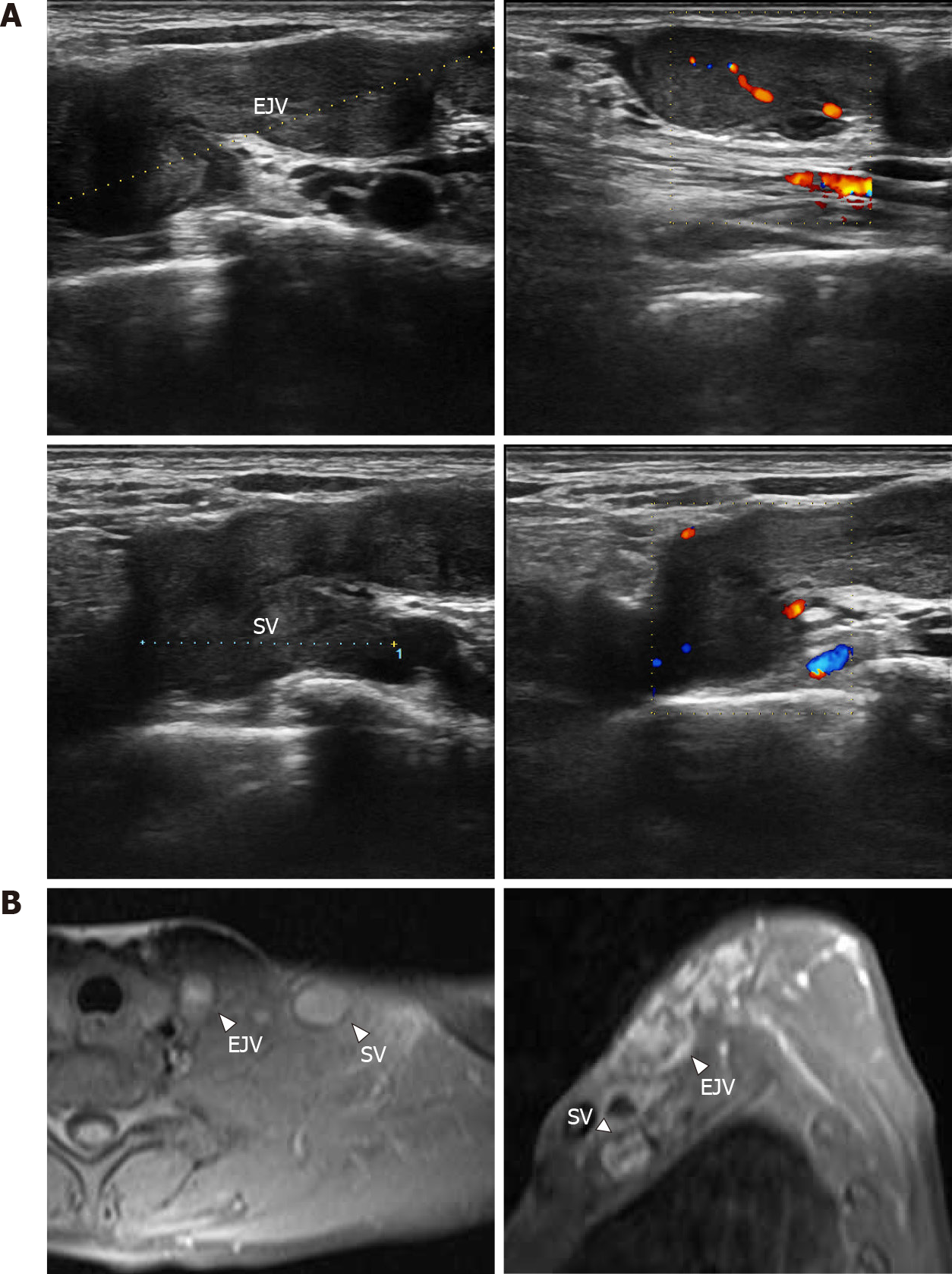
Duplex ultrasonography showed that a circular solid hypoechoic mass could be seen on the left clavicle along the external jugular vein, with a general length of approximately 4.2 cm (Figure 1A). There was no blood flow signal passing through the lumen, and the mass invaded into the subclavian vein along the external jugular vein. Hypoechoic masses were observed in some areas of the subclavian vein, involving a length of approximately 2.1 cm, and no obvious involvement was observed in the left internal jugular vein (Figure 1A). Similarly, the left supraclavicular fossa showed irregular patchy patterns on cervical magnetic resonance imaging. The lesion was mostly located between the left common jugular vein and the sternocleidomastoid muscle, and the boundary was not clear. The contrast-enhanced scan showed slight enhancement, and the wall of the adjacent left subclavian vein was thickened. Lesions with abnormal signals in the left supraclavicular fossa were tested by biopsy, considering the possibility of lymphatic or granulomatous lesions (Figure 1B). The abnormal signal in the left supraclavicular fossa was considered to indicate lymphatic or granulomatous lesions, and biopsy was recommended.
The pathologist reported that the mass was a spindle cell mesenchymal tumor without definite malignant features, but the specific tumor type and nature needed to be determined by routine histology and immunohistochemistry. Surgery was then performed; because only the mass was removed, no vein reconstruction was required.
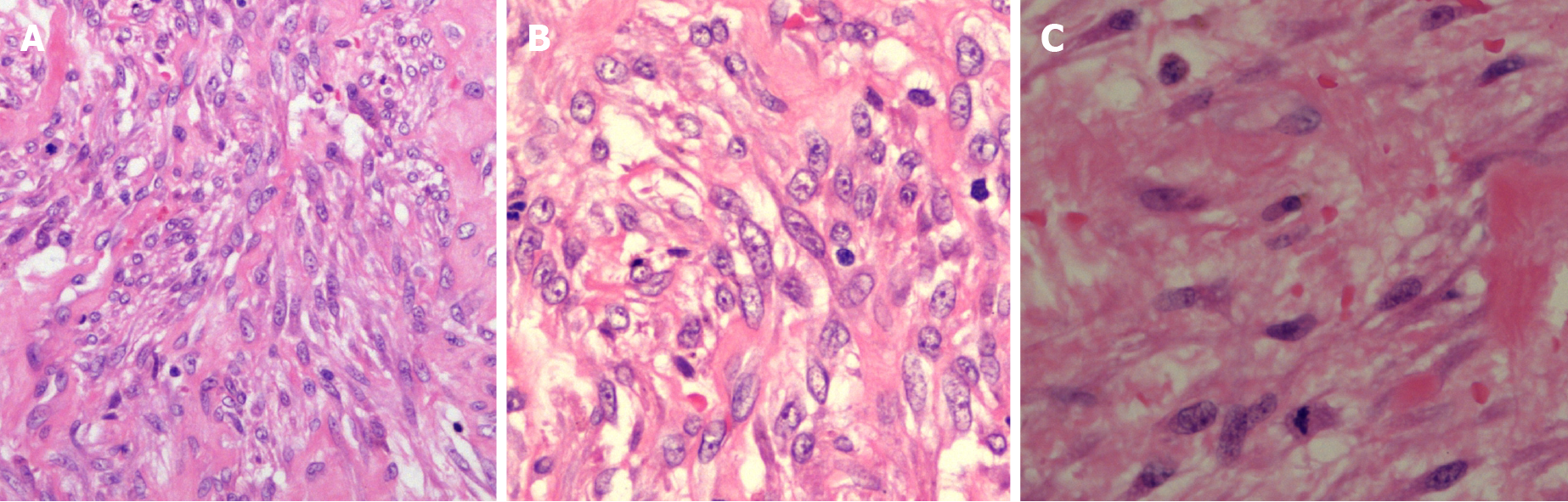
Pathologic examination was based on a microscopic investigation, which reported that the mass from the left jugular vein was a fibroblast/myofibroblast tumor, consistent with intravascular nodular fasciitis. Hematoxylin-eosin staining showed that the mass was composed of spindle cells, which were mainly fibroblasts and myofibroblasts. The cell morphology was relatively consistent, with an irregular fascicular-shaped arrangement. The atypia was mild, with a small amount of nuclear division, a small amount of mucous degeneration and collagen deposition in the stroma, as well as scattered inflammatory cell infiltration and erythrocyte extra
Left external jugular vein and subclavian vein IVF.
Conservative treatment of this disease has a certain cure rate, so both clinical observation with conservative treatment and surgical treatment options are available for this disease. Surgical indications were present in this patient, and the surgical treatment option was selected by the patient and his family. Therefore, the patient underwent left neck mass resection after the relevant examinations. After surgical treatment, he had no neurological symptoms or swelling of his arm.
The surgery began with an 8 cm skin incision that was made along the left supraclavicular vein, and the solid mass in the external jugular vein was visible on the deep surface of the left supraclavicular platysma muscle. The solid mass, approximately 4 cm long, grew along the blood vessel and involved the left subclavian vein and its surrounding branches. As requested by the patient's family members, no clavicu
The patient had no thoracic duct injury or pneumothorax after the operation and was discharged four days after the operation. The outpatient review was good one month after discharge. Through telephone follow-up one year after discharge, the patient noted that the left neck did not have a lump or discomfort. The next follow-up will be two years after discharge. The disease will be mainly monitored for potential malignant behavior.
Nodular fasciitis is a nonneoplastic myofibroblastic hyperplasia that grows quickly, is sometimes rich in cells and has certain atypicality. This condition can be seen with a high number of mitotic figures and is easily misdiagnosed as various types of soft tissue sarcoma; therefore, it is also known as pseudosarcoma fasciitis. IVF is a rare and special type of nodular fasciitis; thus far, only seven cases have been reported in the domestic literature, and thirty-six cases have been reported internationally. IVF generally occurs in adolescent and young adult patients, with an average age of onset of 26.5 years worldwide. Of these thirty-six patients, 80% were under the age of thirty. There is no significant difference in the incidence rate between males and females, and the ratio is close to 1:1[8-10]. However, among the cases reported domestically, the epidemiological characteristics are inconsistent with those of foreign cases, which may be caused by an insufficient number of reported cases. Usually, before the onset of the disease, the patients were healthy, and even after disease development, the patients generally had no feelings of discomfort, such as pain, tenderness or decreased mobility. IVF is most commonly found in the upper extremities, head and neck, followed by the lower extremities and trunk, and there have been reports of rare sites[5-7]. Most of the clinical manifestations have been painless masses that grow slowly under the skin. A few may have pain or tenderness. Most of the lesions were solitary nodules, and a few patients presented with multiple nodules, the size of the lesion ranged from a minimum of 0.6 cm to 5 cm, and the course of the disease ranged from 2 wk to 8 years[11]. IVF is a benign disease that is usually cured by simple local excision. Thus far, the pathogenesis of endovascular fasciitis is still unclear. It was confirmed that spindle cells are derived from myofibroblasts based on their immunohistochemical characteristics. A few cases have suggested that this condition may be related to previous trauma, thrombosis, and high levels of estrogen[12].
IVF mainly involves small veins or arteries, where lesions extend longitudinally along the vessels and pass through the vessel wall into surrounding connective tissue and adjacent vessels. Due to the small size of the vessels, the lesions may have a polynodular appearance, and intracavitary lesions are separated from the main tumor. The histological features are myofibroblast proliferation with a fractured structure, erythrocyte exosmosis, and a mucous background, but interstitial mucous degeneration is not evident, and there is no pleomorphism and rarely mitosis[6,7]. The intravascular component of IVF can be identified by immunohistochemical staining for elastin and smooth muscle actin. Immunohistochemical staining for smooth muscle actin, caldesmon and vimentin indicates positivity for spindle cells, Ki-67 staining reveals a low proliferative index (< 10%), and staining for c-kit, S100 protein, desmin, CD31 and CD34 is negative, suggesting that IVF involves myofibroblastic differentiation[5,11]. USP6 gene rearrangement has been recently demonstrated in nodular fasciitis, and the presence of fusions involving the USP6 gene in most cases provides a useful tool for diagnostic confirmation[13,14]. Because of its vessel involvement, IVF may be mistaken for a malignancy. When IVF cells undergo atypical changes, more mitotic signs may occur, often involving various layers and lumens of blood vessels, which may lead to the overdiagnosis of malignant tumors, such as fibrosarcoma, leiomyosarcoma, and mucinous liposarcoma. Despite the invasive growth of these lesions, there is no evidence of invasive clinical behavior, recurrence or metastasis[7]. The absence of large atypical hyperchromatic nuclei, and the presence of abnormal mitotic figures and immunohistochemical characteristics of the spindle cells can identify IVF[11,15].
Intravascular fasciitis is a rare vascular-associated nodular fasciitis that is easily misdiagnosed as other tumors. We report a case of this rare disease and provide insights on IVF, with the hope of improving the recognition of non-neoplastic lesions to avoid misdiagnosis.
We thank all the histology technologists at the Department of Pathology, Hangzhou First People's Hospital for their technical support.
| 1. | Patchefsky AS, Enzinger FM. Intravascular fasciitis: a report of 17 cases. Am J Surg Pathol. 1981;5:29-36. [PubMed] |
| 2. | Pan H, Zhou L, Deng C, Zheng J, Chen K, Gao Z. A Rare Case of Intravascular Fasciitis Misdiagnosed as Deep Venous Thrombosis. Ann Vasc Surg. 2020;62:499.e5-499.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Pomoni A, Sotiriadis C, Gay F, Jouannic AM, Qanadli SD. Percutaneous endovascular biopsy of intravascular masses: efficacy and safety in establishing pre-therapy diagnosis. Eur Radiol. 2018;28:301-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Takahashi K, Yanagi T, Imafuku K, Kitamura S, Inamura-Takashima Y, Yamaguchi Y, Hata H, Shimizu H. Ultrasonographic features of intravascular fasciitis: case report and review of the literature. J Eur Acad Dermatol Venereol. 2017;31:e457-e459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Bártů M, Dundr P, Němejcová K, Prokopová P, Zambo I, Černý Š. Intravascular fasciitis leading to an aortic dissection. A case report. Cesk Patol. 63:196-199. [PubMed] |
| 6. | Kim HK, Han A, Ahn S, Min S, Ha J, Min SK. Intravascular Fasciitis in the Femoral Vein with Hypermetabolic Signals Mimicking a Sarcoma: The Role of Preoperative Imaging Studies with Review of Literature. Vasc Specialist Int. 2021;37:50-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Kuklani R, Robbins JL, Chalk EC, Pringle G. Intravascular fasciitis: report of two intraoral cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121:e19-e25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Li N, Hong DK, Zheng XX, Zhou YD, Chen XS. Images in Vascular Medicine: Intravascular fasciitis of the common femoral vein mimicking deep venous thrombosis. Vasc Med. 2020;25:602-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Le P, Servais AB, Salehi P. Intravascular fasciitis presenting as recurrent deep venous thrombosis. J Vasc Surg Cases Innov Tech. 2020;6:609-611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (2)] |
| 10. | Kang JH, Kim DI, Chung BH, Heo SH, Park YJ. A Case Report of the Intravascular Fasciitis of a Neck Vein Mimicking Intravascular Tumorous Conditions. Ann Vasc Dis. 2018;11:553-556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | He Y, Huang G, Wang Y, Zhao H, Zheng Z, Lin W, Zhou L, Zhu Z, Wang C. Intravascular fasciitis of the hip joint in a postpartum female: misdiagnosed as low grade fibromyxoid sarcoma. Int J Clin Exp Pathol. 2021;14:519-525. [PubMed] |
| 12. | Min SI, Han A, Choi C, Min SK, Ha J, Jung IM. Iliofemoral vein thrombosis due to an intravascular fasciitis. J Vasc Surg Cases. 2015;1:73-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Lu Y, He X, Qiu Y, Chen H, Zhuang H, Yao J, Zhang H. Novel CTNNB1-USP6 fusion in intravascular fasciitis of the large vein identified by next-generation sequencing. Virchows Arch. 2020;477:455-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Wang JC, Li WS, Kao YC, Lee JC, Lee PH, Huang SC, Tsai JW, Chen CC, Chang CD, Yu SC, Huang HY. Clinicopathological and molecular characterisation of USP6-rearranged soft tissue neoplasms: the evidence of genetic relatedness indicates an expanding family with variable bone-forming capacity. Histopathology. 2021;78:676-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Wang T, Tang GC, Yang H, Fan JK. Occipital nodular fasciitis easily misdiagnosed as neoplastic lesions: A rare case report. World J Clin Cases. 2020;8:6144-6149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Silano F S-Editor: Zhang H L-Editor: Webster JR P-Editor: Zhang H