Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10286
Peer-review started: May 18, 2022
First decision: June 27, 2022
Revised: July 6, 2022
Accepted: August 25, 2022
Article in press: August 25, 2022
Published online: October 6, 2022
Processing time: 132 Days and 4 Hours
Morphological anomalies of teeth, including talon cusp, dens evaginatus, gemin
A 47-year-old woman who complained of left maxillary first molar loss for half a year presented to our department seeking treatment by dental implant rest
CBCT is a useful tool for diagnosing and planning the management of tooth conc
Core Tip: Diagnosing concrescent teeth through routine clinical examination alone is difficult, and most cases of concrescence are found accidentally during extraction. A definite preoperative diagnosis of concrescence would contribute to a better treatment plan and fewer undesirable complications. Herein, we report a case of concrescence in the posterior maxilla involving an impacted third molar and the second molar to facilitate reasonable preoperative examinations and treatments in similar cases.
- Citation: Su J, Shao LM, Wang LC, He LJ, Pu YL, Li YB, Zhang WY. Concrescence of maxillary second molar and impacted third molar: A case report. World J Clin Cases 2022; 10(28): 10286-10292
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10286.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10286
Morphological anomalies of teeth, including talon cusp, dens evaginatus, gemination, fusion, conc
The presence of concrescence presents challenges for surgical, endodontic, orthodontic, and even prosthodontic treatment. However, diagnosing concrescent teeth through routine clinical examination alone is difficult, and most cases of concrescence are found accidentally during extraction. A definite preoperative diagnosis of concrescence would contribute to a better treatment plan and fewer undesirable complications.
Herein, we report a case of concrescence in the posterior maxilla involving an impacted third molar and the second molar to facilitate reasonable preoperative examinations and treatments in similar cases.
A 47-year-old Chinese woman who complained of left maxillary first molar loss for half a year presented to the Department of Stomatology seeking treatment by dental implant restoration.
The patient had undergone left upper posterior tooth root extraction half a year prior, and after that, she could not chew with her left 3 molars.
Had histories of dental treatment and denied the history of systemic diseases.
Denied personal and family history of systemic diseases.
The intraoral examination revealed that the maxillary first molar was lost. The maxillary second molar was mesially tilted, and only a mesial periodontal pocket with a probing depth of approximately 7 mm was observed. No abnormal mobility of the maxillary second molar was observed.
The preoperative routine blood examination revealed no abnormalities.
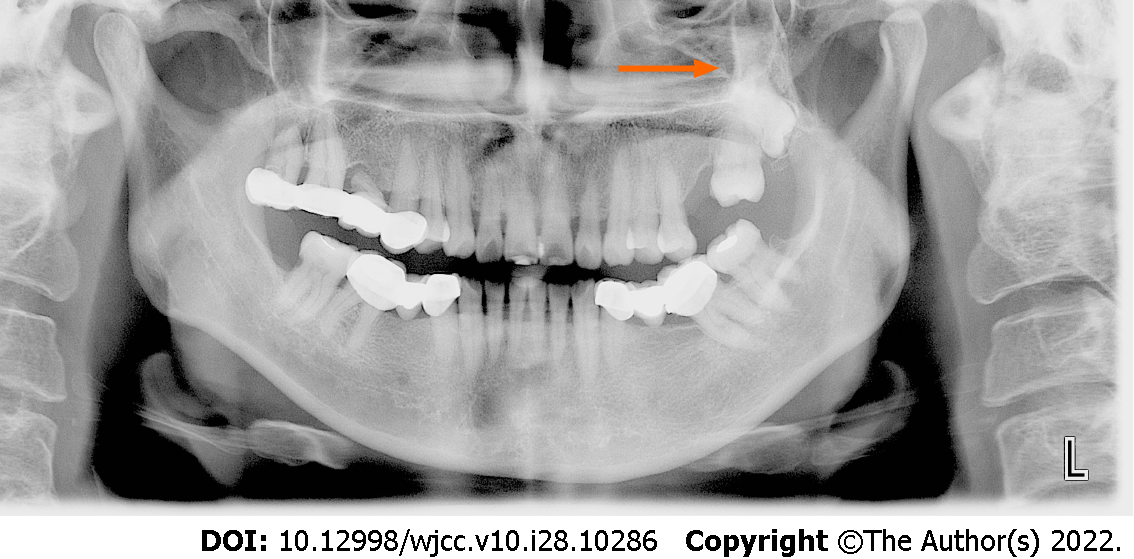
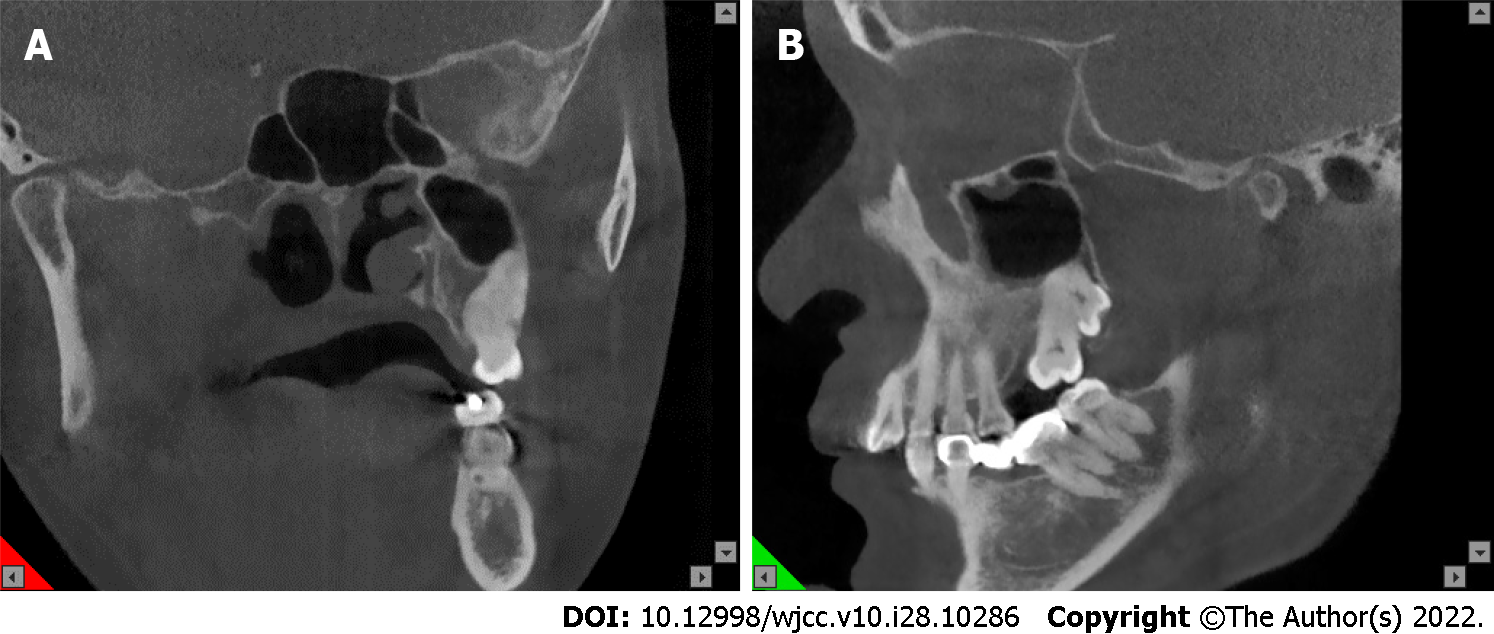
The panoramic film showed angular bone defects located in the mesial aspect of the maxillary second molar. The third molar was completely impacted. The image showed an overlap between the impacted third molar and the second molar, without an obvious dividing line (Figure 1). Cone-beam computed tomography (CBCT) was recommended to determine whether there was fusion of the two molars and the spatial relationship between the root and the maxillary sinus. CBCT showed that the root apex of the third molar was located in the ipsilateral maxillary sinus. The two molars were united along the roots, and the boundary between the distal root of the second molar and the mesial root of the third molar was not clear. The two molars showed separate pulp cavity systems (Figure 2).
An orthodontist was consulted to determine the risk of moving the concrescent teeth to create adequate space for the expected implant prosthesis. The patient was informed of the unpredicted situation and agreed to undergo extraction of the second and third molars followed by implant restoration three months later.
Tooth concrescence.
Before the operation, 10 mL of venous blood was collected from the patient to prepare concentrated growth factor (CGF). The extraction was performed under local anesthesia with articaine (68 mg of articaine with 17 μg of adrenalin). The resistance to dislocation was high during the operation. A horizontal incision was created in the distal alveolar crest of the second molar, followed by flap and bone removal. Finally, the two molars were extracted completely (Figure 3). After the operation, oro-antral communication was not observed, as indicated by a negative Valsalva maneuver. The alveolar fossa was debrided, filled with CGF, and tightly sutured. Routine antibiotics (amoxicillin capsules, 0.5 g, 3 times a day) were taken after the operation.
The patient returned one week later for suture removal. The wound healed well, and the patient reported no discomfort. An appointment was made for a follow-up visit three months later.
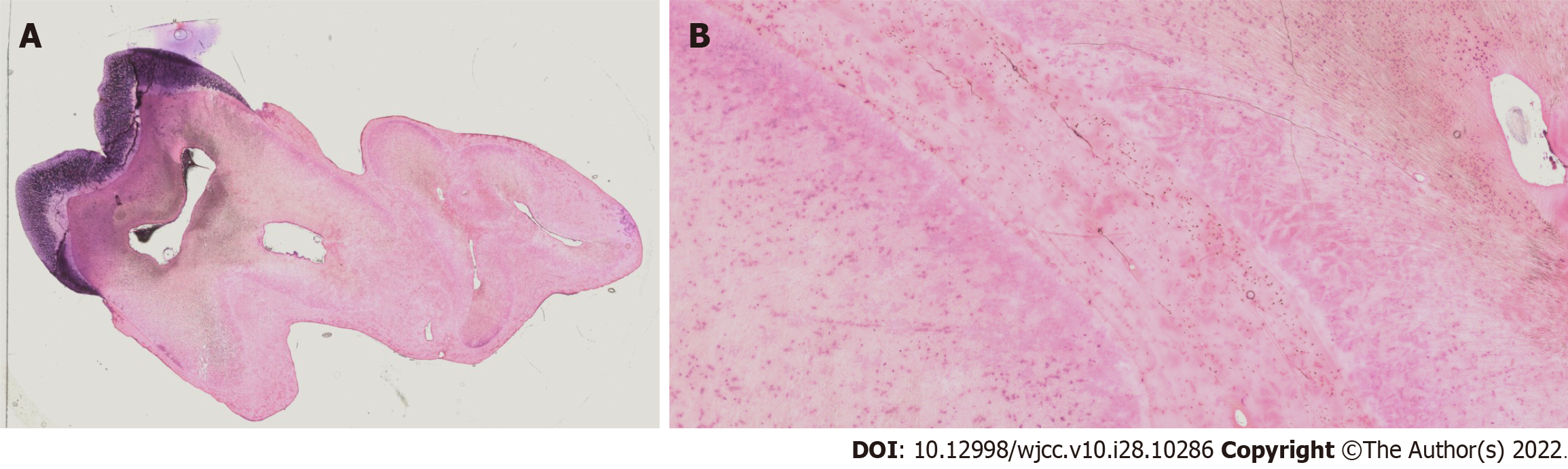
The teeth were kept for examination, serially sectioned, stained, and observed under a slide scanning system (SQS-1000, TEKSQRAY, Shengqiang Technology Co., Ltd., China). The histological observation revealed that the roots of the second and third molars were united with cementum (Figure 4), indicating concrescence of the two molars.
Tooth concrescence is a rare abnormality in which two or more teeth are joined with cementum[6,7]. Concrescent teeth are rarely observed in the mandible and are more commonly observed in the posterior maxilla[8-11]. This twinning anomaly usually occurs between the second molar and an impacted third molar or between the third molar and a supernumerary molar, in either deciduous or permanent dentition[8,10,12-14]. Concrescence can occur during root formation due to insufficient development space (categorized as true concrescence)[15-17]. In addition, even after complete root formation, concrescence may occur due to interdental bone resorption and cementum deposition (also known as acquired concrescence)[15]. It has been speculated that local chronic inflammatory stimuli caused by caries, occlusal trauma and rapid orthodontic tooth movement are involved in acquired concrescence[7,15,18,19]. In this case, thickened cementum at the junction of the two molars was found on histological examination. The first molar of the patient was extracted half a year prior and led to the mesial incline of the second molar. It is unlikely that the distal root would have converged toward the root of the impacted third molar and induced cementum deposition to such an extent in such a short period of time. In addition, no signs of chronic inflammation were found on clinical examination. Instead, the concrescence was likely caused by space restriction and subsequent cementum deposition between adjacent roots during root development. Indeed, the limited space was also confirmed by the failed eruption of the third molar.
Clinically diagnosing concrescent teeth is difficult even with the aid of routine radiography, especially when impacted molars are involved[20]. The identification of concrescent teeth has been reported to occur mainly during or after an extraction procedure. Thus, preoperative ignorance of this condition can lead to unexpected complications and even legal consequences due to inadequate communication. Panoramic radiography provides only vague information regarding the definite spatial relationship of the involved tooth roots. As in this case, concrescent teeth can easily be misdiagnosed as root overlap on routine radiography, undoubtedly increasing the difficulty and reliability of making a diagnosis and planning treatment[16]. However, CBCT images can capture three-dimensional information and show positional relationships between teeth and important anatomical structures, such as adjacent teeth, alveolar bone, and maxillary sinuses[21]. In this case, we could intuitively identify the configuration of the roots and the relationship between the roots and the maxillary sinuses by CBCT, which was very helpful for determining a feasible treatment plan and minimizing possible complications during extraction. Considering the cost and radiation of CBCT, as well as the findings of this case, we suggest that plain radiography be used for the routine examination of patients and that CBCT be used to solve problems that are difficult to solve based on plain radiography alone.
The differential diagnosis of concrescent teeth is fused teeth, which are characterized by the involvement of dentin fusion. It is difficult to distinguish whether dentine fusion is involved using CBCT, as dentin has a density of mineralization close to that of cementum. Ono et al[22] performed postoperative micro-CT to differentiate concrescent teeth from fused teeth, but it seems that performing such a destructive examination before surgery is impractical. In this case, the diagnosis of concrescence was determined by postoperative histological examination. However, it must be realized that the diagnosis of fused teeth is important in cases involving endodontic treatment. As shown in Figure 2, concrescent teeth usually have independent pulp-canal systems, which is an important distinction between concrescent and fused teeth that can be easily identified even on routine radiography[8].
The management of concrescent teeth should be personalized, and various treatments, including extraction, surgical division, endodontic treatment and orthodontic management, have been recommended in reported cases[11,23-25]. If the tooth concrescence does not cause aesthetic problems, functional disturbance, or other undesirable complications, no additional medical management is needed. In this case, surgical division of the concrescent teeth would have been difficult due to the high degree of root union. In addition, considering the estimated bone deficiency for orthodontic movement and the positional relationship between the root of the third molar and the base of the maxillary sinus, it was not feasible to obtain space for a first molar implant by orthodontic traction of the concrescent teeth. Accordingly, the concrescent teeth were extracted. However, the potential impact of the removal of concrescent teeth on masticatory function due to the loss of the second molar must be considered. A definite diagnosis of concrescence and a preoperative conversation can reduce the risk of legal disputes.
Clinically, patients who present with malocclusion or impacted teeth are often treated by orthodontic correction, surgery, or a combination of both, and these patients are mostly children[26,27]. Long-term malocclusion or unilateral chewing may cause associated temporomandibular disorders; additionally, malocclusion and habitual unilateral chewing are very common in adults[28], who are often overlooked. Therefore, clinicians should pay more attention to such conditions during the consultation, especially for adult patients, to provide relevant guidance and treatment.
Tooth concrescence is a rare clinical phenomenon that is not easily diagnosed by intraoral examination and routine radiography. Dentists should be aware of the possibility of concrescence when teeth, especially teeth in the posterior maxillary area, appear to be overlapping on imaging. CBCT is a useful tool for diagnosing and planning the management of tooth concrescence and may be beneficial for reducing unnecessary complications.
| 1. | Rohrer MD. Clinical outline of oral pathology: Diagnosis and treatment. 3rd ed. Philadelphia: Lea & Febiger, 1992: 112-117. |
| 2. | Goswami M, Bhardwaj S, Grewal N. Prevalence of Shape-related Developmental Dental Anomalies in India: A Retrospective Study. Int J Clin Pediatr Dent. 2020;13:407-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | ALHumaid J, Buholayka M, Thapasum A, Alhareky M, Abdelsalam M, Bughsan A. Investigating prevalence of dental anomalies in Eastern Province of Saudi Arabia through digital orthopantomogram. Saudi J Biol Sci. 2021;28:2900-2906. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Guttal KS, Naikmasur VG, Bhargava P, Bathi RJ. Frequency of developmental dental anomalies in the Indian population. Eur J Dent. 2010;4:263-269. [PubMed] |
| 5. | Goutham B, Bhuyan L, Chinnannavar SN, Kundu M, Jha K, Behura SS. Prevalence of Dental Anomalies in Odisha Population: A Panoramic Radiographic Study. J Contemp Dent Pract. 2017;18:549-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Sharma U, Gulati A, Gill NC. Concrescent triplets involving primary anterior teeth. Contemp Clin Dent. 2013;4:94-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Whitaker SB. Oral and maxillofacial pathology. J Am Dent Assoc. 2000;131:718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 8. | Gunduz K, Sumer M, Sumer AP, Gunhan O. Concrescence of a mandibular third molar and a supernumerary fourth molar: report of a rare case. Br Dent J. 2006;200:141-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Syed AZ, Alluri LC, Mallela D, Frazee T. Concrescence: Cone-Beam Computed Tomography Imaging Perspective. Case Rep Dent. 2016;2016:8597872. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Arun D. Concrescence of impacted mandibular third molar with a fourth molar. CODS J Dent. 7:48-49. [DOI] [Full Text] |
| 11. | Foran D, Komabayashi T, Lin LM. Concrescence of permanent maxillary second and third molars: case report of non-surgical root canal treatment. J Oral Sci. 2012;54:133-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Tapadiya V, Ramanojam S, Gelada K, Sethi S, Oswal N. Concrescence of Erupted Second Molar and Impacted Third Molar: A Rare Case Report. IOSR J Dent and Med Sci. 2017;16:74-76. [DOI] [Full Text] |
| 13. | Romito LM. Concrescence: report of a rare case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:325-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Singh A, Bhatia HP, Sharma N. Coexistence of fusion and concrescence of primary teeth: in a child with Down syndrome. Spec Care Dentist. 2017;37:147-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Mader CL. Concrescence of teeth: a potential treatment hazard. Gen Dent. 1984;32:52-55. [PubMed] |
| 16. | Shazli N, Almasri M. Concrescence of an Erupted Maxillary Second Molar with an Impacted Third Molar: A Case Report. SciEP. 2017;5:1-3. [DOI] [Full Text] |
| 17. | Pindborg JJ. Pathology of the dental hard tissues. 1st ed. Philadelphia: W. B. Saunders Company, 1970: 223-226. |
| 18. | Sanjay S. Textbook of Oral Pathology. 1st ed. India: Jaypee Brothers Medical Publishers, 2006: 211-221. |
| 19. | White SC, Michael J. ORAL RADIOLOGY: Principles and interpretation. 6th ed. Oxford: Mosby Elsevier, 1987: 314-338. |
| 20. | Mohan B. Hypercementosis and concrescence of maxillary second molar with third molar: a case report and review of literature. Oral Health Dent Manag. 2014;13:558-561. [PubMed] |
| 21. | Syed AZ, Sin C, Rios R, Mupparapu M. Incidental occurrence of an unusually large mastoid foramen on cone-beam computed tomography and review of the literature. Imaging Sci Dent. 2016;46:39-45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Ono M, Shimizu O, Ueda K, Hashimoto J, Honda K. A case of true concrescence diagnosed with cone-beam CT and in vivo micro-CT. Oral Radiol. 2010;26:106-109. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Venugopal S, Smitha BV, Saurabh SP. Paramolar concrescence and periodontitis. J Indian Soc Periodontol. 2013;17:383-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Suter VG, Reichart PA, Bosshardt DD, Bornstein MM. Atypical hard tissue formation around multiple teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:138-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Stanford ND, Hosni S, Morris T. Orthodontic management of a dental concrescence: a case report. J Orthod. 2017;44:209-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Perillo L, Isola G, Esercizio D, Iovane M, Triolo G, Matarese G. Differences in craniofacial characteristics in Southern Italian children from Naples: a retrospective study by cephalometric analysis. Eur J Paediatr Dent. 2013;14:195-198. [PubMed] |
| 27. | Cavuoti S, Matarese G, Isola G, Abdolreza J, Femiano F, Perillo L. Combined orthodontic-surgical management of a transmigrated mandibular canine. Angle Orthod. 2016;86:681-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (11)] |
| 28. | Matarese G, Isola G, Alibrandi A, Lo Gullo A, Bagnato G, Cordasco G, Perillo L. Occlusal and MRI characterizations in systemic sclerosis patients: A prospective study from Southern Italian cohort. Joint Bone Spine. 2016;83:57-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Isola G, Italy; Memis S, Turkey; Varga ML, Croatia S-Editor: Wang DM L-Editor: A P-Editor: Wang DM